
Extracorporeal membrane oxygenation use in a 26-week pregnant female with a severe COVID-19 infection: case report
Introduction
The SARS-COV-19 (COVID-19) pandemic has been a global crisis that has affected society as a whole in an unprecedented way. One population of particular interest has been pregnant women. Pregnant women have historically been at higher risk of infection with other coronaviruses and preliminary studies indicate that pregnancy may be a risk factor in the development of severe COVID-19 (1,2). Indeed, pregnant women with COVID-19 face higher rates of severe infection, preeclampsia/eclampsia, preterm delivery, and maternal and infant mortality (3). Mother-to-child transmission of COVID-19 has also been documented previously in the literature (4). We present a case of a profoundly hypoxic COVID-19 positive woman presenting at our emergency department (ED) at ~26 weeks 2 days (26w2d) gestation that required venovenous extracorporeal membrane oxygenation (VV ECMO) leading to preterm intrauterine fetal demise (IUFD) and a spontaneous en caul vaginal delivery. We present the following article in accordance with the CARE reporting checklist (available at https://jeccm.amegroups.com/article/view/10.21037/jeccm-22-11/rc).
Case presentation
History of present illness (HPI)
The patient is a 23-year-old female, G5P1AB4, at ~26w2d gestation with no significant past medical history who presented to the ED via Emergency Medical Services (EMS) complaining of profoundly worsening shortness of breath. She was diagnosed with COVID-19 10 days prior to presentation and states that her symptoms severely worsened about 2 to 3 days prior to calling EMS. Furthermore, the patient stated that she was unvaccinated against COVID-19.
ED course
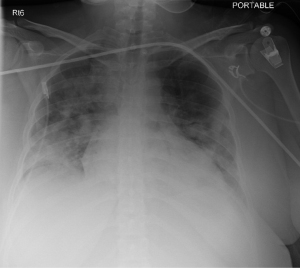
On arrival to the ED, exam revealed an anxious appearing, diaphoretic female in moderate respiratory distress with oxygen saturations of 75% on 15-L of oxygen via a non-rebreather (NRB). The patient was started on high flow nasal cannula (HFNC) with semi-proning attempted; however, despite maximum settings, her oxygensaturation did not exceed 85%. Bilevel positive airway pressure (BiPAP) was attempted, but the patient was unable to tolerate it. Ultimately, patient was intubated and heroxygen saturation did not exceed 89% despite maximum vent settings [positive end-expiratory pressure (PEEP) 18, tidal volume (TV) 400, respiratory rate (RR) 24, fraction of inspired oxygen (FiO2) 100%]. Computed tomography (CT) pulmonary embolism (PE) was negative for a PE and her lung imaging was consistent with multifocal pneumonia/COVID-19. Obstetrics/gynecology (OB/GYN) and the ECMO teams were consulted during her stay in the ED and the patient was admitted to the medical intensive care unit (MICU) (Figure 1).
Hospital course
Day 1 (16:00): patient cannulated for VV ECMO via right internal jugular approach;
Day 2 (04:00): labor and deliver nurse unable to detect fetal heart tones on tocometry—determined to be an IUFD. OB/GYN discussed possible induction;
Day 2 (10:15): spontaneous en caul vaginal delivery in the MICU;
Day 4: patient’s clinical status improved and she was decannulated from ECMO;
Day 7: developed post-partum pre-eclampsia and started on a magnesium drip;
Day 9: patient extubated without difficulty;
Day 10: downgraded out of the ICU to the OB/GYN service;
Day 14: patient left against medical advice.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). The patient and her family were unable to be contacted after being discharged despite multiple attempts so informed consent was not obtained. All means were taken to protect the identity of this patient and all patient identifiers were removed from the report.
Discussion
We describe a patient with COVID-19 related hypoxia at 26 weeks gestation, who experienced IUFD after VV ECMO cannulation and post-partum pre-eclampsia but ultimately recovered from infection. COVID-19 infection can cause a drop in O2 saturation, and VV ECMO may be needed to treat the unstable oxygen levels (5). VV ECMO is often used when the lungs need transient respiratory support to facilitate lung healing, but is rarely prescribed in pregnancy (6). The outcomes of VV ECMO in pregnancy tend to be very positive, with one systematic review concluding that 91% of mothers and 78% of newborns survived following VV ECMO (7). However, it is important to note that existing literature focuses on the use of VV ECMO in the setting of pregnancy induced acute respiratory distress syndrome (ARDS) rather than respiratory complications due to COVID-19 pneumonia.
The relationship between COVID-19 and IUFD is still up for debate. Curi et al. found that in a population of 33 COVID-19 positive patients in the Bronx, 2 patients experienced IUFD (8). However, this study did not calculate statistics about whether there was a statistically significant relationship between COVID-19 and IUFD. Nayak et al. conducted a study about the relative effect of COVID-19 on pregnancy by comparing outcomes in COVID-19 negative patients with COVID-19 positive patients (9). This study found that 2.23% [3] of COVID-19 positive patients experienced IUFD while 3.79% [31] COVID-19 negative patients experienced IUFD (9). This study also did not calculate whether or not there was a statistically significant difference in the rates of IUFD between COVID-19 positive and negative patients. Jessie et al. also attempted to determine whether or not there is a relationship between COVID-19 positivity in pregnant patients and IUFD by retrospectively testing for COVID-19 in mothers who experienced IUFD (10). A total of 55% of the 20 included patients refused to participate, and of those who did participate 88.9% of patients were COVID-19 negative at the time of IUFD (10). At this time, there is very little definitive information about the relationship between COVID-19 and IUFD, however COVID-19 is very rarely found in the newborn, suggesting that COVID-19 likely has minimal (if any) effects on the fetus (11). The third trimester presents the highest risk for vertical transmission of COVID-19, which is coincidentally when most pregnant women are admitted with severe cases of COVID-19 (12). In this case, no signs of fetal distress were observed in response to poor O2 saturation.
As highlighted in our case, this patient’s oxygensaturation dramatically improved with VV ECMO use. Early detection of IUFD was critical to protect this patient from complications such as septicemia, acute renal failure, and disseminated intravascular coagulation (DIC), which could have further complicated this patient’s recovery (13).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jeccm.amegroups.com/article/view/10.21037/jeccm-22-11/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jeccm.amegroups.com/article/view/10.21037/jeccm-22-11/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). The patient and her family were unable to be contacted after being discharged despite multiple attempts so informed consent was not obtained. All means were taken to protect the identity of this patient and all patient identifiers were removed from the report.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wastnedge EAN, Reynolds RM, van Boeckel SR, et al. Pregnancy and COVID-19. Physiol Rev 2021;101:303-18. [Crossref] [PubMed]
- Phoswa WN, Khaliq OP. Is pregnancy a risk factor of COVID-19? Eur J Obstet Gynecol Reprod Biol 2020;252:605-9. [Crossref] [PubMed]
- Jering KS, Claggett BL, Cunningham JW, et al. Clinical Characteristics and Outcomes of Hospitalized Women Giving Birth With and Without COVID-19. JAMA Intern Med 2021;181:714-7. [Crossref] [PubMed]
- Mahyuddin AP, Kanneganti A, Wong JJL, et al. Mechanisms and evidence of vertical transmission of infections in pregnancy including SARS-CoV-2s. Prenat Diagn 2020;40:1655-70. [Crossref] [PubMed]
- Li X, Guo Z, Li B, et al. Extracorporeal Membrane Oxygenation for Coronavirus Disease 2019 in Shanghai, China. ASAIO J 2020;66:475-81. [Crossref] [PubMed]
- Pacheco LD, Saade GR, Hankins GDV. Extracorporeal membrane oxygenation (ECMO) during pregnancy and postpartum. Semin Perinatol 2018;42:21-5. [Crossref] [PubMed]
- Ong J, Zhang JJY, Lorusso R, et al. Extracorporeal membrane oxygenation in pregnancy and the postpartum period: a systematic review of case reports. Int J Obstet Anesth 2020;43:106-13. [Crossref] [PubMed]
- Curi B, Sabre A, Benjamin I, et al. Coronavirus infection in a high-risk obstetrical population of the South Bronx, New York. Am J Obstet Gynecol MFM 2020;2:100203. [Crossref] [PubMed]
- Nayak AH, Kapote DS, Fonseca M, et al. Impact of the Coronavirus Infection in Pregnancy: A Preliminary Study of 141 Patients. J Obstet Gynaecol India 2020;70:256-61. [Crossref] [PubMed]
- Jessie D, Chloe D, Jade L, et al. The Correlation Between COVID 19 and IUFD: Our Experience at a Tertiary Maternity Unit in France, the CHSF. Science Journal of Clinical Medicine 2020;9:87-90. [Crossref]
- Kotlyar AM, Grechukhina O, Chen A, et al. Vertical transmission of coronavirus disease 2019: a systematic review and meta-analysis. Am J Obstet Gynecol 2021;224:35-53.e3. [Crossref] [PubMed]
- Knight M, Bunch K, Vousden N, et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ 2020;369:m2107. [Crossref] [PubMed]
- Saha D, Kurude VN, Mundhe S. A study of intrauterine fetal death in a tertiary care hospital. Int J Reprod Contracept Obstet Gynecol 2019;8:2647-52. [Crossref]
Cite this article as: LaPuma NA, Gonuguntla RK, Joseph R. Extracorporeal membrane oxygenation use in a 26-week pregnant female with a severe COVID-19 infection: case report. J Emerg Crit Care Med 2022;6:18.


