
Obstructive shock presenting like ST-elevation myocardial infarction (STEMI): case report
Introduction
Pulmonary emboli are responsible for 60,000 to 100,000 deaths in the United States annually (1). On average, hospitalizations complicated by pulmonary emboli cost 2.5 times more than hospitalizations without this complication (2). Pulmonary emboli can sometimes have atypical presentations, mimicking conditions like myocardial infarctions or pneumothoraxes, therefore making timely diagnosis challenging. Chest X-ray, electrocardiogram, and troponins are often the initial diagnostic tests conducted for a patient presenting with shortness of breath or chest pain. In cases of massive pulmonary emboli that cause heart strain, there can be characteristic findings on an electrocardiogram: tachycardia, S1Q3T3 pattern, incomplete/complete right bundle branch block, atrial fibrillation, T wave inversion in leads V1-V4, and ST elevation in aVR (3). Being aware of how pulmonary embolism can present atypically allows physicians to recognize and treat it in a timely fashion. This results in improved patient outcomes and decreased costs to the healthcare system. In our case report, we present a 66 years old African American male who presented to the emergency department in shock and was found to have extensive bilateral pulmonary emboli despite presenting like a patient having a myocardial infarction. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-139).
Case presentation
The patient was a 66-year-old African American male who presented to Virginia Hospital Center with cardiogenic and obstructive shock secondary to extensive bilateral pulmonary emboli. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written permission was obtained from the patient to discuss his case.
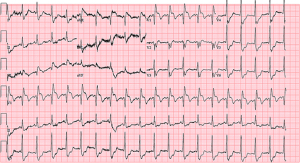
The patient had complaints of shortness of breath without accompanying chest pain. He had experienced a similar episode the previous week which had resolved with rest. Notably, the patient was active physically, including walking his dog daily and was not seeing a physician regularly. He also was a habitual cigar smoker. The patient did not have significant medical history (no malignancies and did not take medications) nor did he have any known family history of hypercoagulable conditions or extensive cardiac history; both his parents had hypertension and his father had diabetes. During the current episode, the shortness of breath did not resolve and when it worsened, EMS was called. Upon arrival at the emergency department, he was given 325 mg aspirin and was found to be diaphoretic, tachypneic, and hypotensive with blood pressure 67/48. Initial EKG showed ST segment elevations in leads V1, V2, and aVR with reciprocal ST depression in V4-V6 as well as a right bundle branch block (Figure 1). His initial troponin was positive at 0.37 ng/mL. Bedside echocardiogram showed no significant right heart strain, ejection fraction, or valvular abnormalities.
In addition to the initial Chest X-ray and electrocardiogram, additional workup was done. Comprehensive metabolic panel (CMP) showed elevated transaminases. brain natriuretic peptide (BNP) was 6,160. Lipid panel revealed high-density lipoprotein (HDL) 27, low-density lipoprotein (LDL) 70, and total cholesterol 130. Initial coagulation parameters were all within normal limits [international normalized ratio (INR): 1.14, prothrombin time (PT): 13.9 s, activated partial thromboplastin time (aPTT): 37 s). Initial lactate was 3.5 which then trended down to 0.8 on hospitalization day 2.
Within 10 minutes of arrival at the emergency room, the patient’s working of breathing increased, and he required intubation. Following intubation, the patient became bradycardic to 33 and went into pulseless electrical activity (PEA) cardiac arrest. Cardiopulmonary resuscitation (CPR) and advanced cardiac life support (ACLS) was initiated, and return of spontaneous circulation (ROSC) was achieved after 3 minutes and with 2 doses of epinephrine and atropine. A heparin drip was initiated, and he was started on vasopressor support with norepinephrine. The patient was emergently taken to the catheterization lab for coronary angiography. No significant coronary artery stenosis was found during the procedure. However, during the catheterization, he developed PEA cardiac arrest again; CPR was performed for about 1−2 minutes and ROSC achieved again. Due to lack of significant coronary artery occlusion and left ventriculogram showing an ejection fraction of 60%, there was high suspicion of extensive pulmonary emboli as the potential etiology for the patient’s positive troponins, ST elevations, shock and cardiac arrests. Alteplase 50mg was given intravenously followed by continuous heparin infusion. In addition, patient had transient atrial fibrillation; he did not have prior history of this condition. Following hemodynamic stabilization in the intensive care unit (ICU), a CT of the chest with intravenous contrast was obtained and confirmed extensive bilateral pulmonary emboli (representative section shown as Figure 2).

Patient’s perspective
Perspective was transcribed from patient at his bedside. He was very surprised to hear about his diagnosis of pulmonary emboli, as he had no personal history of blood clots nor did he have family history of it. He was also surprised to hear about going into cardiac arrest twice but was pleased that he does not have any cognitive deficits. He still felt weak but is optimistic that with adequate cardiac rehabilitation he will return to his baseline.
Conclusions
The purpose of this report is to highlight the potential varied presentations for pulmonary emboli. Typically, elevated troponins and ST elevations on electrocardiogram are associated with myocardial infarctions as opposed to pulmonary emboli. However, elevated troponins are increasingly becoming more recognized as typical in pulmonary emboli cases (4). If there are changes on electrocardiogram due to pulmonary emboli, they are typically associated with right heart strain—findings such as ST elevation in aVR, right axis deviation, and right bundle branch block. Mechanisms for this ST elevation possibly involve increased oxygen demand secondary to the right heart strain, leading to microvascular coronary spasm or epicardial vasospasm (5). Other reports have involved the possibility of paradoxical embolism due to increased right heart pressure causing a right to left shunt (6). This particular patient had no evidence of an atrial or ventricular septal defect. An alternative reported mechanism is a surge in catecholamines due to severe hypoxemia because of the pulmonary embolism. This surge in turn could then induce myocardial ischemia (7). In reality, there may be a combination of all these mechanisms that could produce the ST elevations on electrocardiogram and myocardial ischemia in cases of pulmonary emboli. It is important as clinicians to recognize that elevated troponins and ST elevations on electrocardiogram, even in anterior septal leads like in this patient, could be a sign of pulmonary emboli. Suspicion for pulmonary emboli should increase further if coronary angiography does not show clinically significant coronary artery occlusion.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/ jeccm-20-139
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-139). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Doherty S. Pulmonary embolism: An update. Aust Fam Physician 2017;46:816-20. [PubMed]
- Heit JA, Spencer FA, White RH. The epidemiology of venous thromboembolism. J Thromb Thrombolysis 2016;41:3-14. [Crossref] [PubMed]
- Shopp JD, Stewart LK, Emmett TW, et al. Findings From 12-lead Electrocardiography That Predict Circulatory Shock From Pulmonary Embolism: Systematic Review and Meta-analysis. Acad Emerg Med 2015;22:1127-37. [Crossref] [PubMed]
- Ng AC, Yong AS, Chow V, et al. Cardiac troponin-T and the prediction of acute and long-term mortality after acute pulmonary embolism. Int J Cardiol 2013;165:126-33. [Crossref] [PubMed]
- Goslar T, Podbregar M. Acute ECG ST-segment elevation mimicking myocardial infarction in a patient with pulmonary embolism. Cardiovasc Ultrasound 2010;8:50. [Crossref] [PubMed]
- Cheng TO. Mechanism of ST-elevation in precordial leads V(1)-V(4) in acute pulmonary embolism. Int J Cardiol 2009;136:251-2. [Crossref] [PubMed]
- Wilson GT, Schaller FA. Pulmonary embolism mimicking anteroseptal acute myocardial infarction. J Am Osteopath Assoc 2008;108:344-9. [PubMed]
Cite this article as: Reddy S, van Buttlar X, Casey D. Obstructive shock presenting like ST-elevation myocardial infarction (STEMI): case report. J Emerg Crit Care Med 2022;6:7.


