
Bacteraemia caused by two different phenotypes of Klebsiella pneumoniae
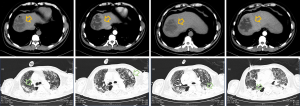
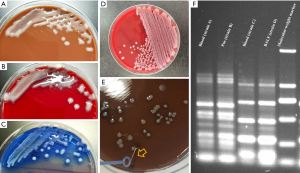
A 74-year-old male was admitted to our intensive care unit (ICU) with high fever and shock. His medical history included poorly controlled blood sugar which led to the long-term complications of diabetes, including liver abscess for one year (Figure 1A,B,C,D). Chest computerized tomography (CT) scan, bronchoalveolar lavage (BAL), CT-guided percutaneous catheter drainage (CTPCD) and blood sample culture were performed to detect the pathogenic microorganisms. Pulmonary fibrosis with infection was recognized in the chest CT (Figure 1E,F,G,H) and the morphology of the colony was mucous (Figure 2A,B,C) while two different colony forms in the agar plate were found (Figure 2D), one of which revealed the phenomenon of “Wire drawing” (Figure 2E). Finally, 4 strains of Klebsiella pneumoniae with different antimicrobial susceptibility were isolated from the blood, pus and bronchoalveolar lavage fluid (BALF) samples. Two of them were identified as carbapenem-resistant Klebsiella pneumoniae (CRKP) and the other two were carbapenem susceptible Klebsiella pneumoniae (CSKP) (Table S1). Pulsed-field gel electrophoresis (PFGE) was performed on the four isolates and sequence homology was found between the strains isolated from blood and BALF (ST-11, CRKP) while the other sequence homology was also detected between the strains isolated from blood and pus (ST-23, CSKP) (Figure 2F). Meropenem (intravenous medication, 2,000 mg q8h, and the trough concentration could maintain between 3.5 and 5.0 ug/mL) and ceftazidime-avibatan (intravenous medication, 2,500 mg q8h) were initiated. The results of blood cultures turned to negative after 5 days treatment and the patients were full recovered.
Bacteraemia is the most serious complications of pneumonia and liver abscess and the infectious agents are often identified as hypervirulent and multiple drug resistance. Two different phenotypes of Klebsiella pneumoniae from diverse sources in one blood sample is extremely rare which remains a great challenge of proper antibiotic therapy. Definitive pathogen identification and antimicrobial drug combination therapy are the key factors to improve the prognosis.
Acknowledgments
Funding: This work was supported by the Scientific Research Project of Shanghai Municipal Health Bureau (No. 201840006).
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-21-15). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained for the use of information and images. The patient’s identity has been kept confidential.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Cite this article as: Zhu C, Yu Y. Bacteraemia caused by two different phenotypes of Klebsiella pneumoniae. J Emerg Crit Care Med 2021;5:29.


