The perils of beta-blockade and the promise of venoarterial extracorporeal membrane oxygenation in managing low-output heart failure in thyroid storm: a case report
Introduction
Thyroid storm is a diagnostic challenge in the emergency department owing to its rare incidence and diverse clinical manifestations. Thyroid hormones affect every organ system and when dysregulated, patients present with a myriad of signs and symptoms. The emergency physician must be adept at rapidly recognizing this endocrine emergency because prompt treatment can reduce the high morbidity and mortality associated with the disease. A complication of thyroid storm is low-output heart failure which ranges from subclinical to life-threatening. These patients present a therapeutic challenge because the initiation of beta-blockers, a cornerstone of therapy in thyroid storm, can precipitate decompensation into cardiogenic shock. We present a case of a young man who presented to the emergency department in thyroid storm, was treated with diltiazem and esmolol prior to recognition of his underlying low-output heart failure, and decompensated into cardiogenic shock. He was ultimately treated with venoarterial extracorporeal membrane oxygenation (VA-ECMO) for refractory cardiogenic shock which enabled him to recover normal left ventricular systolic function.
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-133).
Case presentation
A 33-year-old otherwise healthy man presented to the emergency department with one week of persistent palpitations associated with chest tightness, shortness of breath, epigastric pain, nausea, and vomiting. He reported having intermittent palpitations over the past year but this was the first time he had sought medical attention. He endorsed fatigue and unintentional 15-pound weight loss over the past few months. He had no medical or surgical history and denied use of over-the-counter or prescription medications. His mother and grandmother had Graves’ disease. He denied recreational drug and alcohol use. He was a full-time carpenter who lived with his wife and enjoyed mountain biking.
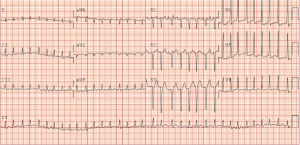
On initial assessment, he was alert, anxious, and diaphoretic with a temperature of 36.5 °C. He was tachycardic with a heart rate of 143 bpm and blood pressure of 94/79 mmHg. Physical examination was notable for jugular venous distention to the angle of the mandible, a nontender symmetrically enlarged thyroid gland, a tachycardic heart rate with an irregular rhythm, clear lung fields, epigastric abdominal tenderness, and warm nonedematous lower extremities. Electrocardiogram revealed atrial fibrillation with a rate of 209 bpm (Figure 1). Chest X-ray showed a borderline enlarged cardiac silhouette with no pulmonary edema (Figure 2). He was started on a diltiazem infusion and heparin infusion in the emergency department and admitted to the intensive care unit. Laboratory results in the emergency department and through hospitalization are shown (Table 1). He had a suppressed thyroid stimulating hormone (TSH) and elevated free thyroxine (T4). Thyrotropin receptor autoantibody level was raised at >40 IU/L consistent with Graves’ disease.
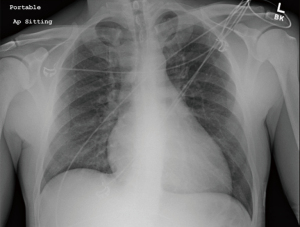
Table 1
| Laboratory test | Reference range | ED | HD 2 | HD 3 | HD 7 | HD 25 |
|---|---|---|---|---|---|---|
| Sodium | 133–145 mEq/L | 136 | 129 | 130 | 155 | 134 |
| Potassium | 3.3–5.3 mEq/L | 4.7 | 6.5 | 5.5 | 3.4 | 4.4 |
| BUN | 6–19 mg/dL | 20 | 46 | 69 | 80 | 26 |
| Creatinine | 0.50–1.30 mg/dL | 0.79 | 2.44 | 3.61 | 0.95 | 0.65 |
| ALP | 39–117 U/L | 170 | 157 | 155 | 105 | 109 |
| AST | 0–37 U/L | 129 | 5220 | 4684 | 283 | 51 |
| ALT | 0–40 U/L | 118 | 3387 | 4069 | 535 | 53 |
| Lactate | 0.5–2.0 mmol/L | – | 6.8 | 3.0 | 2.0 | – |
| Troponin T | 0.000–0.030 ng/mL | 0.037 | 0.08 | – | – | – |
| NT-ProBNP | 0–450 pg/mL | 7,364 | – | – | – | – |
| TSH | 0.270–4.200 uIU/mL | <0.014 | – | <0.005 | <0.005 | – |
| T4 | 5.3–12.3 ìg/dL | 16.6 | – | – | – | – |
| T4 free | 0.90–1.70 ng/dL | – | >5.00 | 7.77 | 2.22 | 0.74 |
| T3 | 80.0–200.0 ng/dL | – | 505.0 | 137 | 77.4 | |
| T3 free | 2.3–4.2 pg/mL | – | – | – | 4.7 | 2.0 |
| Thyrotropin receptor Ab | 0.00–1.75 IU/L | – | >40 | – | – | – |
VA-ECMO, venoarterial extracorporeal membrane oxygenation; ED, emergency department; HD, hospital day; BUN, blood urea nitrogen; ALP, alkaline phosphatase; AST, aspartate transaminase; ALT, alanine transaminase; NT-Pro-BNP, N-terminal prohormone brain natriuretic peptide; TSH, thyroid-stimulating hormone; T4, thyroxine; T3, triiodothyronine.
A clinical diagnosis of thyroid storm was made in the context of a Burch-Wartofsky score of 55. A score ≥45 is highly suggestive of a diagnosis of thyroid storm. After endocrinology consultation, he was treated with propylthiouracil, hydrocortisone, and potassium iodide. An esmolol infusion was started, replacing diltiazem for rate control. Propylthiouracil was replaced with methimazole when labs revealed severe transaminitis. Transthoracic echocardiography (TTE) revealed severe global hypokinesis with a left ventricular ejection fraction (EF) of 10% to 15%. On hospital day 2, he continued to have atrial fibrillation with rapid ventricular rate ranging from 150 to 200 bpm with poor response to increasing doses of esmolol. He became progressively more hypotensive requiring vasopressor and inotropic support. A pulmonary artery catheter was deferred due to hyperkalemia and concern of inducing a dysrhythmia. He developed acute liver failure and anuric acute renal failure with a lactate elevation to 6.8 mmol/L. By hospital day 3, he continued to clinically deteriorate with declining mentation and cool extremities. VA-ECMO was initiated for refractory thyroid storm with multisystem organ dysfunction. Medical treatment with methimazole, potassium iodide, and hydrocortisone was continued while VA-ECMO provided a bridge to recovery. With continued circulatory support, his multiorgan system dysfunction improved and he was decannulated after 7 days. His TTE on hospital day 14 demonstrated improved left ventricular function with an EF of 56%. He recovered over the remainder of his 25-day hospitalization and was discharged to an acute rehabilitation facility for 9 days before returning home. Outpatient endocrinology follow up care was arranged and he underwent complete thyroidectomy 3 months after discharge. Pathology showed diffuse multinodular hyperplastic changes. He remains on levothyroxine and guideline-directed medical therapy for heart failure with reduced ejection fraction. He has since returned to work as a carpenter and experiences fatigue only with strenuous exercise.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
Hyperthyroidism is characterized by excess circulating thyroid hormone with the most common etiology being Graves’ disease (1). The prevalence of hyperthyroidism is 1.3% of the general population and thyroid storm is a rare life-threatening manifestation (2,3). Thyroid storm is diagnostically challenging because it mimics other more common disease processes. Thyroid hormones affect every organ system and in excess cause dysfunction of the cardiovascular, gastrointestinal, hepatic, thermoregulatory, and central nervous systems. While many patients have a prior history of hyperthyroidism to guide the differential diagnosis, thyroid storm may be the first clinical presentation. Burch and Wartofsky developed a scoring system using the different signs and symptoms of thyroid storm to aid in the diagnosis (4). The diagnosis can be confirmed with a suppressed TSH and elevated free T4. Early recognition and treatment is imperative to reduce the high morbidity and mortality associated with the condition (5,6).
Thyrotoxicosis profoundly affects the cardiovascular system and the development of cardiac complications markedly impacts the prognosis. Thyroid hormones alter cardiovascular dynamics by decreasing systemic vascular resistance and increasing heart rate, cardiac contractility, and circulating blood volume (7,8). These combined effects increase preload and decrease afterload, ultimately increasing cardiac output by 50% to 300% (7). In patients with prolonged occult or untreated hyperthyroidism, sustained volume overload and increased cardiac workload may lead to heart failure. While hyperthyroidism is associated with high-output heart failure in a majority of patients, a subset of patients can develop low-output heart failure (9,10). Low-output heart failure occurs predominantly in patients with underlying heart disease in whom the increased cardiac workload and myocardial oxygen demand exacerbates subclinical coronary artery disease or compensated heart failure (10). Chronic persistent sinus tachycardia or atrial fibrillation may cause rate-induced cardiomyopathy in patients with structurally normal hearts as well (8,10).
Management of thyroid storm involves reducing the peripheral hyperadrenergic effects of thyroid hormones. T3 upregulates beta-adrenergic receptors to varying degrees in different tissues with an especially dominant effect on the heart (11). The increased density of cardiac beta-adrenergic receptors enhances the heart’s sensitivity to endogenous circulating catecholamines as well as its sensitivity to beta-blockers. Beta-blockers are a cornerstone of therapy for thyroid storm. Propranolol is preferred due to its nonselective beta-adrenergic antagonism and additional effect of reducing the peripheral conversion of inactive T4 to active T3. However, guidelines for the management of thyroid storm do not provide an algorithm for patients with low-output heart failure in whom beta-blockers should be used with extreme caution. The hyperadrenergic state plays a compensatory role in maintaining cardiac output and end organ perfusion in these patients. Beta-blockade disrupts this compensatory mechanism and can cause a significant drop in cardiac output with hemodynamic instability. Several case reports in the literature report cardiovascular collapse after administration of a beta-blocker in patients with thyroid storm (12-14). Many of these patients did not have clinical evidence of heart failure on presentation.
Patients with thyrotoxicosis-induced low-output heart failure must be identified early to tailor treatment and prevent further left ventricular dysfunction. A complete hemodynamic evaluation should be performed prior to initiating treatment and patients should continue to be hemodynamically monitored in an intensive care setting. Bedside TTE should be performed to screen for subclinical heart failure, assessing for chamber dilatation and reduced EF. Short-acting beta-blockers such as esmolol are a safer option than long-acting beta-blockers like propranolol. Esmolol has a short elimination half-life of 10 minutes enabling easier titration and immediate cessation upon evidence of circulatory collapse (13). Calcium channel blockers should be used with caution as they have a similar duration of action as standard beta-blockers and may cause severe hypotension. Digoxin may be considered in patients with heart failure and atrial fibrillation, however higher potentially toxic doses of digoxin are required to achieve a therapeutic effect in hyperthyroid patients (10). Amiodarone should not be a first line agent for cardioversion since it is an iodine-rich drug that induces thyroid derangements and can exacerbate preexisting thyrotoxicosis (5).
In patients who develop cardiogenic shock, mechanical circulatory support with VA-ECMO should be strongly considered. VA-ECMO may be used as a temporizing measure to maintain systemic delivery of oxygenated blood while cardiac function recovers and anti-thyroid medications restore a euthyroid state. A systematic review reports a 78.5% survival rate and near complete recovery of left ventricular function in patients with thyrotoxicosis-induced cardiomyopathy treated with VA-ECMO (15). Our patient had a severely decreased left ventricular EF of 10% to 15% prior to cannulation and successfully weaned off VA-ECMO after 7 days, by which time his serum free T4 levels had normalized. His TTE on postoperative day 15 demonstrated complete recovery of left ventricular function with an EF of 56%.
In conclusion, low-output heart failure is a rare and dangerous complication of thyroid storm and medications commonly used to treat thyroid storm can precipitate shock and worsen outcomes in these patients. VA-ECMO is a potential temporizing measure that has been shown to improve left ventricular function and survival. The emergency physician who can rapidly recognize thyroid storm, identify underlying low-output heart failure, and initiate appropriate medical therapy under close hemodynamic monitoring will undoubtedly provide these critically ill patients with the best chance for survival and recovery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-133
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-133). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cooper DS. Hyperthyroidism. Lancet 2003;362:459-68. [Crossref] [PubMed]
- Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99. [Crossref] [PubMed]
- Galindo RJ, Hurtado CR, Pasquel FJ, et al. National Trends in Incidence, Mortality, and Clinical Outcomes of Patients Hospitalized for Thyrotoxicosis With and Without Thyroid Storm in the United States, 2004-2013. Thyroid 2019;29:36-43. [Crossref] [PubMed]
- Burch HB, Wartofsky L. Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am 1993;22:263-77. [Crossref] [PubMed]
- Idrose AM. Acute and emergency care for thyrotoxicosis and thyroid storm. Acute Med Surg 2015;2:147-57. [Crossref] [PubMed]
- Bourcier S, Coutrot M, Kimmoun A, et al. Thyroid Storm in the ICU: A Retrospective Multicenter Study. Crit Care Med 2020;48:83-90. [Crossref] [PubMed]
- Klein I, Danzi S. Thyroid disease and the heart. Circulation 2007;116:1725-35. [Crossref] [PubMed]
- Dahl P, Danzi S, Klein I. Thyrotoxic cardiac disease. Curr Heart Fail Rep 2008;5:170-6. [Crossref] [PubMed]
- Siu CW, Yeung CY, Lau CP, et al. Incidence, clinical characteristics and outcome of congestive heart failure as the initial presentation in patients with primary hyperthyroidism. Heart 2007;93:483-87. [Crossref] [PubMed]
- Fadel BM, Ellahham S, Ringel MD, et al. Hyperthyroid heart disease. Clin Cardiol 2000;23:402-8. [Crossref] [PubMed]
- Bilezikian JP, Loeb JN. The influence of hyperthyroidism and hypothyroidism on alpha and beta adrenergic receptor systems and adrenergic responsiveness. Endocr Rev 1983;4:378-88. [Crossref] [PubMed]
- Fraser T, Green D. Weathering the storm: Beta-blockade and the potential for disaster in severe hyperthyroidism. Emerg Med (Fremantle) 2001;13:376-80. [Crossref] [PubMed]
- Dalan R, Leow M. Cardiovascular Collapse Associated with beta blockade in thyroid storm. Exp Clin Endocrinol Diabetes 2007;115:392-96. [Crossref] [PubMed]
- Abubakar H, Singh V, Arora A, et al. Propranolol-induced circulatory collapse in a patient with thyroid crisis and underlying thyrocardiac disease: A word of caution. J Investig Med High Impact Case Rep 2017;1-6. [Crossref] [PubMed]
- White A, Bozso SJ, Moon MC. Thyrotoxicosis induced cardiomyopathy requiring support with extracorporeal membrane oxygenation. J Crit Care 2018;45:140-3. [Crossref] [PubMed]
Cite this article as: Zacharia JA, May TL. The perils of beta-blockade and the promise of venoarterial extracorporeal membrane oxygenation in managing low-output heart failure in thyroid storm: a case report. J Emerg Crit Care Med 2021;5:37.