
Under (compartment) pressure in the intensive care unit: a case report
Introduction
Compartment syndrome by itself is an emergency, but when that is combined with acute renal failure secondary to toxin-induced rhabdomyolysis in the setting of methamphetamine overdose and exertional rhabdomyolysis, it takes on a new dimension of complexity (1). Adding to the intricacy of the case, this patient’s compartment syndrome involved the posterior deltoid. Posterior deltoid compartment syndrome has rarely been reported, and when observed, is usually post-procedural after an orthopedic surgery; either due to positioning during an operation or after intraosseous (IO) access placement. Only 20 cases of this have been reported in the literature, and the creatinine kinase (CK) in this case was the highest reported (2). We present a clinical case where a patient developed posterior deltoid compartment syndrome which led to rhabdomyolysis, uremia, and acute renal failure (ARF) requiring intubation and hemodialysis (HD) followed by emergent fasciotomy. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-163).
Case presentation
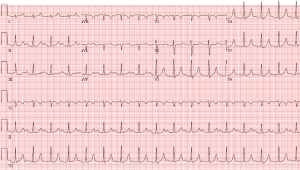
A 37-year-old male with no past medical history who presented via emergency medical services (EMS) after an illicit drug binge, was noted to have agitation, confusion, and initially was protecting his airway with a Glasgow Coma Score of 13. Per EMS reports, the patient was initially moderately responsive and complained of vague pain in his back and shoulder as well as scratching incessantly at his skin, additionally voicing that he could not hear anything. Vital signs on admission showed a temperature of 96.9 degrees Fahrenheit, blood pressure of 77/50 mmHg, heart rate of 95 beats per minute, oxygen saturation of 94% on room air, and respiratory rate of 38 breaths per minute. Initial physical exam revealed tachycardia, tachypnea, dilated pupils, diaphoresis, a tender and firm left deltoid with decreased passive range of motion, and scattered abrasions throughout. Labs were unable to be obtained prior to intubation due to agitation. He was also given multiple liters of crystalloid fluid for resuscitation but remained in hypovolemic shock requiring norepinephrine and vasopressin to maintain mean arterial pressure (MAP) above 65 mmHg. Post-intubation, labs were notable for a urine drug screen (UDS) positive for methamphetamines and amphetamines, arterial blood gas (ABG) with a pH of 7.25, pCO2 of 37.4 mmHg, and pO2 of 169 mmHg, potassium of 7.7 mmol/L, creatinine of 2.71 mg/dL, phosphorous of 19.7 mg/dL, and CK of 228,635 U/L. Troponin I was also elevated at 2.099 ng/mL and after trending this value, continued to rise for the first 36 hours peaking at 8.932 ng/mL—consistent with a non-ST segment elevation myocardial infarction (NSTEMI). Initial electrocardiogram (EKG) (Figure 1) showed peaked T waves, consistent with his hyperkalemia, but no evidence of ST segment elevations. An X-ray of the left shoulder and a head computed tomography (CT) scan were unrevealing. Patient was intravenously administered 2 grams of calcium gluconate, 10 units intravenous regular insulin, an ampule of D50, and sodium zirconium cyclosilicate for his hyperkalemia. Despite these interventions, a repeat potassium showed an increase to 8.1 mmol/L so an emergent nephrology consult was obtained and an emergent Trialysis line was placed in the patient’s right internal jugular vein for temporary HD access. Labs were checked again after HD which showed that potassium had improved to 3.6 mmol/L and CK also improved. Compartment pressures of the deltoid were checked: the anterior pressure was 15 mmHg and the posterior was elevated at 40 mmHg. As the life-threatening electrolyte abnormalities had resolved, the patient was taken to the operating room (OR) for emergent fasciotomy. Intraoperatively, the humeral head was identified and two incisions were created diagonally from the humeral head to access the anterior and posterior aspects of the deltoid. The fascia was opened revealing bulging muscle especially in the posterior aspect. The middle portion of the deltoid still felt tight, so a third incision was made overlying this area. The muscle belly in the posterior aspect was dusky in appearance, but not frankly necrotic. A standard volar upper extremity fasciotomy was then performed with the incision starting in the axilla and traversing the crease of the biceps, coming across the acromioclavicular fossa and extending onto the hand to release the carpal tunnel. After surgery, the patient remained in the ICU and underwent a total of two sessions of HD with normalization of his CK, but unfortunately remained anuric so was transitioned to continuous renal replacement therapy (CRRT) which he required for four days until his creatinine recovered enough and his urine output (UOP) was adequate. Due to ongoing vasopressor requirements, a transthoracic echocardiogram (TTE) was performed which showed a thickened mitral valve, ejection fraction of 40%, cardiomyopathy, and grade 1 diastolic dysfunction, which had not previously been documented. After 6 days, due to the marked edema, the patient returned to the OR for delayed primary closure with a continuous external tissue expander and wound vacuum assisted closure (VAC) placement. The patient was successfully extubated after twelve days of mechanical ventilation and was able to be transferred out of the ICU to a general medical floor. In the setting of cardiomyopathy with a reduced ejection fraction and elevated troponin I, a nuclear medicine stress test was performed which showed an ejection fraction of 79% with no evidence of reversible ischemia. With the assistance of occupational therapy (OT), the patient began to regain some of the strength in his left upper extremity. Per the last available outpatient OT note, the patient had not yet regained his pre-surgical strength but had made major strides towards it, with the main deficit being his ability to dress himself. It remains unclear what degree of disability will be permanent. The patient and his family were highly satisfied with the care he received. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
Neither ARF or rhabdomyolysis are particularly uncommon occurrences, but when combined in the setting of posterior deltoid compartment syndrome due to exertional and toxin-induced rhabdomyolysis, the case becomes more intriguing. Rhabdomyolysis, the dissolution or breakdown of striated muscles, is caused by leakage of the sarcoplasmic proteins such as CK into the circulation (3). The clinical triad of myalgia, weakness, and myoglobinuria is seen in less than 10% of rhabdomyolysis cases. While there is no clearly defined level of CK that constitutes rhabdomyolysis, CK levels are a more sensitive marker for muscle breakdown compared to myoglobin. This is because CK has a longer half-life than myoglobin (36 hours versus 2–4 hours, respectively), leading to frequent false positives when myoglobin alone is checked (4). Methamphetamine intoxication is commonly seen in the emergency department (ED) and is associated with a higher average level of CK (5). Rhabdomyolysis leads to ARF with a more rapid increase in creatinine compared to many other causes of ARF. Had a fractional excretion of sodium (FENa) been checked in this case, it likely would have been <1 indicating a prerenal cause, presumably due to the preglomerular vasoconstriction, not acute tubular necrosis (6).
The mainstay of the treatment of rhabdomyolysis is intravenous fluid resuscitation. Fluids are essential given the presence of massive hypovolemia, with some fluid pathologically accumulating in muscle compartments instead of being in the intravascular space, as seen in this case (7). Crystalloids are typically given at a rate of 1.5 liter per hour until goal UOP is reached. Goal UOP is 3 mL/kg/h and urinary pH of 6.5 with a serum pH of 7.5. Urinary alkalinization with sodium bicarbonate or diuresis with mannitol is not recommended (7). In the article by Bosch et al., they present a comparison of studies regarding preventative and therapeutic regimens in rhabdomyolysis and results of these studies indicate that there is no difference in resuscitative fluid; whether it be normal saline (NS) alone or NS plus bicarbonate and mannitol. There is no effect on peak CK or recovery time in patients with pH <6.5 who receive NS versus lactated Ringer’s (LR) versus bicarbonate. Multiple studies summarized in the article show that early intervention with intravenous fluid resuscitation have better outcomes than late intervention (3).
The most life-threatening parts of rhabdomyolysis and ARF are the electrolyte derangements, specifically the hyperkalemia. Hyperkalemia management includes an EKG which may start to show peaked T waves when potassium is greater than 6.0 mmol/L. If potassium is greater than 6.0 mmol/L and there are EKG changes, in order to stabilize the myocardium and decrease the threshold potential, intravenous calcium gluconate should be administered. Intravenous regular insulin should be administered next in order to begin to shift the potassium intracellularly. Concomitantly with the insulin, dextrose should be given to counteract hypoglycemia. Nebulized albuterol, a beta 2 agonist, can also be used (8). Hypocalcemia can be seen but should not be treated unless the patient is symptomatic as the added calcium could increase the precipitation of intramuscular calcium phosphate (3).
In the critical care or surgical setting, there are a number of drugs that should be avoided in these patients including the depolarizing agent succinylcholine, benzodiazepines, propofol, and ketamine (4). Succinylcholine has been associated with increased hyperkalemia and life-threatening arrhythmias, but these have generally been found to be in patients who had concomitant malignant hyperthermia or a previously undiagnosed muscular dystrophy. Propofol has been associated with propofol infusion syndrome (PRIS) which has been observed in patients on long-term propofol infusions or on short-term high doses of propofol. PRIS is clinically characterized by metabolic acidosis and cardiac dysfunction, along with rhabdomyolysis, hypertriglyceridemia, or ARF in patients on propofol. Ketamine administration can produce agitation and prolonged muscle activity leading to worsening rhabdomyolysis. (9). Bearing in mind these considerations, rocuronium was used as a paralytic for the endotracheal intubation and propofol initially was avoided, but due to the uncontrolled agitation and delirium, was ultimately required along with a midazolam infusion.
From the surgical perspective, posterior deltoid compartment syndrome is extremely rare due to the increased compliance of the fascial layers as well as the communication of the shoulder compartments (10). Elevated compartment pressure can be confirmed with an intra-compartmental pressure monitor with normal pressure between 0–10 mmHg. Once pressure is noted to be elevated, the patient must be taken for an emergent fasciotomy when stable. Surgical exploration releases the edema and pressure, and is necessary to determine if there is any necrotic tissue so that debridement can be done down to the level of healthy tissue (11). The surgical approach involves incisions over the anterolateral and posterolateral aspects of the shoulder in order to expose the anterior, middle, and posterior compartments as seen in Figure 2. Preferably, wound closure can be achieved by delayed primary closure (11).

Predominantly in patients who are encephalopathic, great attention must be paid to the physical exam in combination with the lab values. Vigilance is important when diagnosing compartment syndrome, especially with multiple other comorbidities. Even when an emergency like compartment syndrome is diagnosed, there can potentially be other, more life-threatening problems that must be addressed prior to fasciotomy. Clinicians should be aware of this, but continue to monitor the compartment pressure and patient for clinical changes.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-163
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-163). The authors have no conflicts of interest to declare
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Thorpe SW, Tarkin IS. Deltoid compartment syndrome is a surgical emergency. J Shoulder Elbow Surg 2010;19:e11-3. [Crossref] [PubMed]
- Kooner S, Crocker D, Matthewson G, et al. Ipsilateral Deltoid and Hand Compartment Syndrome: A Case Report and Review of the Literature. JBJS Case Connect 2020;10:e0289 [Crossref] [PubMed]
- Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med 2009;361:62-72. Erratum in: N Engl J Med 2011 May 19;364(20):1982. [Crossref] [PubMed]
- Torres PA, Helmstetter JA, Kaye AM, et al. Rhabdomyolysis: pathogenesis, diagnosis, and treatment. Ochsner J 2015;15:58-69. [PubMed]
- Richards JR, Johnson EB, Stark RW, et al. Methamphetamine abuse and rhabdomyolysis in the ED: a 5-year study. Am J Emerg Med 1999;17:681-5. [Crossref] [PubMed]
- Corwin HL, Schreiber MJ, Fang LS. Low fractional excretion of sodium. Occurrence with hemoglobinuric- and myoglobinuric-induced acute renal failure. Arch Intern Med 1984;144:981-2. [Crossref] [PubMed]
- Better OS, Stein JH. Early management of shock and prophylaxis of acute renal failure in traumatic rhabdomyolysis. N Engl J Med 1990;322:825-9. [Crossref] [PubMed]
- Hollander-Rodriguez JC, Calvert JF Jr. Hyperkalemia. Am Fam Physician 2006;73:283-90. [PubMed]
- Segura LG, Lorenz JD, Weingarten TN, et al. Anesthesia and Duchenne or Becker muscular dystrophy: review of 117 anesthetic exposures. Paediatr Anaesth 2013;23:855-64. [Crossref] [PubMed]
- Wijesuriya JD, Cowling PD, Izod C, et al. Deltoid compartment syndrome as a complication of lateral decubitus positioning for contralateral elbow surgery in an anabolic steroid abuser. Shoulder Elbow 2014;6:200-3. [Crossref] [PubMed]
- Thadikonda KM, Egro FM, Ma I, et al. Deltoid Compartment Syndrome: A Rare Complication after Humeral Intraosseous Access. Plast Reconstr Surg Glob Open 2017;5:e1208 [Crossref] [PubMed]
Cite this article as: Pietrangelo M, Hess J. Under (compartment) pressure in the intensive care unit: a case report. J Emerg Crit Care Med 2021;5:20.


