
The value of Doppler assessment in transthoracic echocardiography in critically ill patients
Introduction
Due to the limited availability of advanced ultrasound machines and well-trained echo-cardiographers, focused echocardiography (echo), using simple handheld machines and a departmental specific protocol, serves as an extension of physical examination (1). Such focused echo protocols have been shown to help direct patient management, and are now widely adopted in various medical fields including emergency medicine (2), trauma service (3) and intensive care units (ICUs) (4). For example, the Focused Intensive Care Echocardiography UK protocol includes the assessment of biventricular systolic function and size, presence of pleural or pericardial effusion, and evidence of hypovolemia (Appendix 1) (1). The hemodynamics of ICU patients, however, change dramatically with time and with various vasoactive drugs or mechanical supports. A detailed echo with Doppler assessment provides important information on top of structural evaluation and eyeballing of myocardium contractility by focused echo. It takes on average 26 minutes for well-trained echo-cardiographers to perform one detailed echo assessment (5). Moreover, echo machines capable for detailed assessment are readily available in most ICU. Given these, performing detailed echo including Doppler assessment for all indicated ICU patients is feasible and we postulate that the findings would have added valves over the focused ones, which could potentially improve patients’ management plan.
This study aimed to study the added benefit of detailed echocardiography assessment, especially with the use of Doppler, on top of the commonly employed focused echo protocol in the setting of an intensive care unit.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jeccm-20-109).
Methods
Design and subjects
This study was approved by the Hospital Authority KC/KE Clinical Research Ethics Committee (reference No.: KCC/KEC-2019-0013). The need of informed consent was waived. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
This was a retrospective single-center study performed in the ICU, Queen Elizabeth Hospital, Hong Kong SAR, between August and October 2018. All patients admitted to the ICU during the period and indicated for echo assessment according to the appropriate use criteria (6) were recruited. There were 356 patients admitted. Echo was indicated in 80 of them and all were included in the study. All the echocardiography was performed by two ICU physicians with level II or III echo skills according to the European Society of Echocardiography (7). The assessment routinely included heart chamber measurement, biventricular systolic function, left ventricular diastolic function, left ventricular outflow tract (LVOT) gradient, and valvular assessment. The echo machine was scanning system cardiovascular S70 (GE Healthcare). While a patient might receive more than one echo assessment, either focused or detailed, only the first detailed echo findings were recorded. This was to avoid the potential correlation between the two echo which might bias the study findings.
Data collection and analysis
For each subject, the following data were collected: Baseline demographics included age, sex, the indications for echo, and the number of transthoracic or transesophageal echo performed.
Positive findings revealed by Doppler assessment would include valvular dysfunction of at least moderate severity, diastolic dysfunction, and dynamic LVOT obstruction.
Dynamic LVOT obstruction defined as maximum LVOT gradient being more than 30mmHg as assessed by CW Doppler.
Continuous data in baseline characteristics were expressed as mean ± standard deviation. The indications for echo and the added values of detailed echo were expressed as number of incidence, percentage.
Results
Baseline demographics
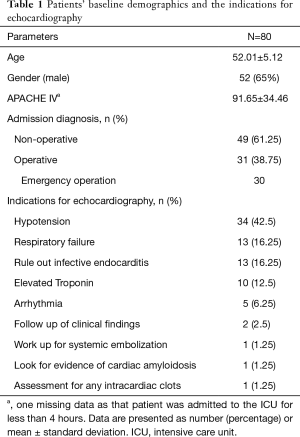
We included 80 subjects for data analysis (mean age 52.0±5.1 years, 65% male). The mean APACHE IV score was 91.7±34.5. Sixty one percent of the cases came from the medical specialties. Among 31 patients who had operations before ICU admission, only 1 of them was elective.
Indications for echo
The commonest indication was hypotension (n=34, 42.5%). Other common indications included respiratory failure (n=13, 16.3%), working up for infective endocarditis (n=13, 16.3%) and working up for elevated serum troponin level (n=10, 12.5%).
The baseline demographics and the indications for echo were summarized in Table 1.
Full table
Positive Doppler findings and clinical relevance
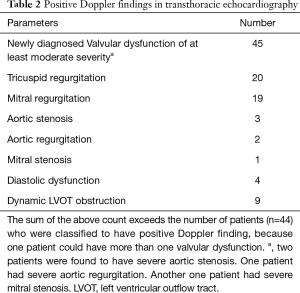
Forty-fourth patients were found to have significant positive Doppler findings (Table 2). Twenty-one had their management plans altered as a result of the Doppler findings obtained in detailed echo (Table 3). The most common alternations were related to haemodynamic management due to the presence of a LVOT gradient of more than 30 mmHg, and the prescriptions of intravenous fluid were stepped up in 8 patients.
Full table

Full table
Four patients were assessed to have diastolic dysfunction, with one of grade 1 and three of grade 2. All of them had their blood pressure lowered because of the diastolic dysfunction.
Forty-five patients were found to have new valvular problems of at least of moderate severity. The most common valvular problems were tricuspid regurgitation (25%), and mitral regurgitation (23.8%). In-patient consultations to cardiothoracic surgeons were needed in 4 patients for potential urgent operations after our detailed echo assessment. There were two cases of severe aortic stenosis. One of them had critical aortic stenosis presented with heart failure and cardiogenic shock and underwent urgent aortic valve replacement during the ICU stay. The other patient with aortic stenosis was arranged to have early operation. There was also one case of severe mitral stenosis requiring early valvular operation, and a case of severe aortic regurgitation who did not have operation during the ICU stay but required frequent follow up. For the remaining 41 patients with moderate valvular problems, follow up echo by cardiologists were arranged on discharge from ICU to monitor the progress.
Discussion
This study has demonstrated the significance of Doppler assessment by transthoracic echocardiography in critically-ill patients. While a lot of studies reported the beneficial effect of focused echo in managing the critically-ill (3,4,8-10), seldom did they report the benefit of full detailed echo assessment including Doppler assessment. Hall et al. was one of the first few groups to present the additional information provided by full echo study on top of focused study alone (11). They reported 28% (n=17) additional diagnostic information obtained following full echo study (11). In our series focusing on Doppler assessment, 26.3% of patients had alternation of treatment direction. While fluid management in the setting of focused echo could only be guided by the collapsibility of the inferior vena cava and the left ventricular systolic function, Doppler assessment offered the important information on the LVOT gradient. Eight patients (10%) had a raised LVOT gradient and thus had their intravenous fluid stepped up. High LVOT gradient was not uncommonly seen in the critically-ill, let alone whether the patient had underlying structural heart problems like hypertrophic obstructive cardiomyopathy or sigmoid-shaped septum. LVOT gradient could be significant even in a patient with structurally normal heart but severely hypovolemic, vasodilated or in left-heart hypercontractile state, but that could not be picked up by focused echo. Inadequate volume resuscitation or further escalation of inotropic agents could otherwise do harm by further aggravating the outflow gradient and exacerbating the cardiogenic shock.
In cases of diastolic dysfunction, if the blood pressure and heart rate were not tightly controlled, they could suffer persistent cardiogenic pulmonary edema due to elevated left ventricular end diastolic pressure and therefore prolonged mechanical ventilation.
For the 45 cases with moderate to severe valvular lesions, 4 urgent cardiothoracic and cardiac consultations were initiated for severe valvular abnormalities. For the remaining 42 subjects with moderate valvular diseases, although the immediate treatment directions were not altered, their valvular disease could progress in severity in few years if they were otherwise not detected and not closely monitored subsequently.
Echocardiography assessment was once a specific technique performed in the field of cardiology. Now thanks to the promulgation by different echo societies and focused echo work-groups in the last 10 years, clinicians of various specialties have acquired more advanced echo skills and knowledge. A lot of times clinicians had already developed their own system of assessment and would perform more detailed assessment on top of the originally-designed focus echo protocols, especially when an abnormality was detected during their initial assessment. Moreover, with advances in echo imaging technology, we had much more refined echo images even with our handy portable echo machines. On top of that, in this era where the application of telecommunication was so widespread (12), echo assessment could be guided by experienced clinicians off-site and detailed echo could be much more easily achievable even for the novice echo-cardiographers. Therefore, with good machines, advanced techniques and telecommunication, the pendulum of echo assessment, at least in certain clinical areas like ICU, should be shifting towards more detailed assessment and to include Doppler assessment. Meanwhile, one must understand the limitation and assumptions behind all those Doppler theories and the pitfalls of Doppler measurement. If not, a high gradient across the mitral valve in patient with tachycardia, which is due to short diastolic time, can be misdiagnosed as significant mitral stenosis. Likewise, a high LVOT gradient could be misdiagnosed if the mitral regurgitation Doppler signal is accidently included in the LVOT gradient assessment. Frequent practice and application of Doppler and detailed echo assessment are the keys to success.
The strength of this study was that the all the echocardiography was performed by accredited ICU physicians according to standard protocol. All the written echocardiography reports were verified with the video clips retrieved from the storage system. The major weakness of this study is that it was a single center retrospective cohort study that limited the generalizability of the results. Ideally the value of detailed echocardiography might be more pronouncedly shown with a randomized controlled trial comparing with focused echo, but this would be difficult to carry out and ethically challenging.
The study results added values to the current evidence that the pendulum should be gradually shifting towards detailed echocardiography to include proper Doppler assessment, at least in the field of intensive care. To facilitate that, training and accreditation of intensivists had always been important, but difficult (13). The hemodynamic alternations due to use of vasoactive medications and application of various mechanical supports mean that echocardiography in ICU is not merely comprehensive echo performed on critically-ill patients, but rather it should be regarded as a sub-branch of echocardiography (14). New technology, including afore-mentioned tele-medicine (12), new imaging techniques, simulation training (15) and artificial intelligence (16,17), could all help to steepen the learning curve and reduce human errors in echo data interpretation.
Conclusions
Doppler assessment in echocardiography remained indispensable in management of critically-ill patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jeccm-20-109
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jeccm-20-109
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-109). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Hospital Authority KC/KE Clinical Research Ethics Committee (reference No.: KCC/KEC-2019-0013) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Intensive Care Society. Focused Ultrasound for Intensive Care, website. Available online: https://www.ics.ac.uk/ICS/FUSIC/ICS/FUSIC/FUSIC_Accreditation.aspx, accessed September 08, 2020.
- Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr 2010;23:1225-30. [Crossref] [PubMed]
- Gunst M, Sperry J, Ghaemmaghami V, et al. Bedside echocardiographic assessment for trauma/critical care: the BEAT exam. J Am Coll Surg. 2008;207:e1-e3. [Crossref] [PubMed]
- Vieillard-Baron A, Slama M, Cholley B, et al. Echocardiography in the intensive care unit: from evolution to revolution?. Intensive Care Med 2008;34:243-9. [Crossref] [PubMed]
- Kimura BJ, DeMaria AN. Time requirements of the standard echocardiogram: implications regarding limited studies. J Am Soc Echocardiogr 2003;16:1015-8. [Crossref] [PubMed]
- Garbi M, Habib G, Plein S, et al. Appropriateness criteria for cardiovascular imaging use in clinical practice: a position statement of the ESC/EACVI taskforce. Eur Heart J Cardiovasc Imaging 2014;15:477-82. [Crossref] [PubMed]
- Popescu BA, Andrade MJ, Badano LP, et al. European Association of Echocardiography recommendations for training, competence, and quality improvement in echocardiography. Eur J Echocardiogr 2009;10:893-905. [Crossref] [PubMed]
- Joseph MX, Disney PJ, Da Costa R, et al. Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest 2004;126:1592-7. [Crossref] [PubMed]
- Kanji HD, McCallum J, Sirounis D, et al. Limited echocardiography-guided therapy in subacute shock is associated with change in management and improved outcomes. J Crit Care 2014;29:700-5. [Crossref] [PubMed]
- Manasia AR, Nagaraj HM, Kodali RB, et al. Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth 2005;19:155-9. [Crossref] [PubMed]
- Hall DP, Jordan H, Alam S, et al. The impact of focused echocardiography using the Focused Intensive Care Echo protocol on the management of critically ill patients, and comparison with full echocardiographic studies by BSE-accredited sonographers. J Intensive Care Soc 2017;18:206-11. [Crossref] [PubMed]
- Becker C, Fusaro M, Patel D, et al. Tele-Ultrasound to Guide Management of a Patient with Circulatory Shock. Am J Med 2017;130:e205-e206. [Crossref] [PubMed]
- Lau G, Swanevelder J. Echocardiography in intensive care--where we are heading? Anaesthesia 2011;66:649-52. [Crossref] [PubMed]
- Colebourn CL, Davies IK, Becher H. Bridging the Gap: Training Critical Care Clinician-Echocardiographers through a Collaborative Curriculum. Journal of the Intensive Care Society 2010;11:13-6. [Crossref]
- Arntfield R, Pace J, McLeod S, et al. Focused transesophageal echocardiography for emergency physicians-description and results from simulation training of a structured four-view examination. Crit Ultrasound J. 2015;7:27. [Crossref] [PubMed]
- Alsharqi M, Woodward WJ, Mumith JA, et al. Artificial intelligence and echocardiography. Echo Res Pract 2018;5:R115-R125. [Crossref] [PubMed]
- Gandhi S, Mosleh W, Shen J, et al. Automation, machine learning, and artificial intelligence in echocardiography: A brave new world. Echocardiography 2018;35:1402-18. [Crossref] [PubMed]
Cite this article as: Man Fong K, Au SY, Yung SK, Wu HLH, Ng GWY. The value of Doppler assessment in transthoracic echocardiography in critically ill patients. J Emerg Crit Care Med 2021;5:3.


