Emergency preparedness for COVID-19: experience from one district general hospital in Wuhan
As a newly infectious disease, COVID-19 was first reported at the end of December 2019 and now has become a global pandemic (1). By August 20th, a total of 22,213,869 cases were confirmed in over 200 countries, including 781,677 death cases (2), which resulted in a challenge of medical care system. During the first 2 months of 2020, the same situation existed in Wuhan, China. As an emergency response, 314 medical rescue teams with 42,000 medical staff from 19 provinces of China provided support and many hospitals were temporarily converted into COVID-19 designated hospitals (3), which played an important role in the pandemic control in Hubei province. Herein, we will share our experience in Wuhan.
Improvement of hospital facilities
Wuhan Third Hospital is a district general hospital with 680 inpatient beds in just one building. On January 25th, it was requisitioned as a designated hospital for COVID-19 by the government, and the medical building was reconstructed immediately into a structure with 600 inpatient beds (including 25 ICU beds). In order to meet the requirements of infection diseases control, the building was divided into three areas (clean areas, semi-contaminated areas and contaminated areas) with two passageways (patient access and medical access) (Figure 1). Meanwhile, the workflow was optimized and the management was refined.

A total of 300 newly confirmed COVID-19 cases were admitted on January 27th. The number of patients admitted had reached 600 in the next three days and 15% of them were critically ill who need organ support, especially the respiratory support. However, insufficient oxygen supply and lack of ventilators brought great obstacles for the rescue of these patients. An oxygen booster station was built immediately within the next three days and a 35-bed temporary ICU on the lobby of the medical building was also set up for the overflow of critical ill patients.
As a newly built designated hospital, it is important to ensure the supply of medical equipment. High-flow nasal cannula, non-invasive and invasive ventilators were deployed from all over the country. The daily consumption of personal protective equipment (PPE) in this hospital was 800 sets and only 2,000 sets were stored at the early stage. As only three days’ consumption can be guaranteed, government and community have made supplement or donations to the hospital consistently. Meanwhile, a system to optimize the rational use of medical equipment was established, especially for the use of PPE.
Medical staff coordination
The medical rescue team with 148 staff from Shanghai arrived to manage the critically ill patients on January 29th. Besides 2 staff for the nosocomial control and 10 for laboratory, a multidisciplinary team (MDT) of 43 doctors from critical care medicine, respiratory, infectious disease, traditional Chinese medicine (TCM), psychology and rehabilitation medicine with 93 registered nurses (RN) were responsible for the management of 120 critically ill patients, while the 500 medical staff of the local hospital were responsible for the other 480 patients. The doctors worked in a 6-hour shift with 6–8 persons per round in the ICU while 20 RNs were on a 4-hour shift. The special medical quality-control group was established to be responsible for protecting the patients and medical staff’s safety as well as controlling the medical quality.
Implementation of clinical practice guidance
Based on the guideline of COVID-19 issued by Surviving Sepsis Campaign (4) and combined with the clinical characteristic of patients admitted to this hospital, a local guidance of COVID-19 was worked out by our team. It was constantly updated along with the continually understanding of the pathophysiology and clinical observation. An early warning system was established to identify the high-risk patients who might be deteriorated and to intervene in time, which may decrease the incidence of critical patients effectively.
At the same time, professional training was performed twice a week to improve the compliance of our COVID-19 guidance and to standardize the timing, indication and model of life support system application, such as respiratory support, continuous renal replacement therapy (CRRT) and extracorporeal membrane oxygenation (ECMO), etc. Meanwhile, TCM was also adopted to provide individual scheme. All the critical cases were managed individually by MDT and all the death cases were audited carefully to analysis the potential drawbacks.
Psychological intervention is important to relieve the anxiety of the patients and the staff. Therefore, a psychological team provided face-to-face or tele-psychological intervention services by WeChat. Rehabilitation is also expected to implement early, which could shorten the length of stay in ICU and improve the quality of life after recovery.
Strengthen the nosocomial infection control
About 2,000 medical staff were infected at the early stages of the epidemic in Wuhan due to lacking knowledge of the contagious disease, weak capability of self-protection and the shortage of PPE (5). Thus, how to prevent cross-infection between patients and staff became the top priority. Besides the building reconstruction and workflow optimization mentioned above, we also do first to set up a special management system and infection control protocol. Second, a strictly training program was performed to enhance the protection ability of the staff by standardization the wearing and undressing of the PPE. Third, we enforced the supervision of the whole working process and every staff behavior and compliance to the preventive protocol, including hand hygiene, etc. (6). Fourth, we put up the preventive protocol and warning signs in the key sites of each potentially contaminated area. Fifth, we demand our staff do not gathering out of contaminated area. Sixth, the personnel health status was monitored daily to ensure the early find of the suspicious infection. Lastly, the tele-medicine equipment was used to reduce unnecessary exposure to the contaminated areas of the staff, such as remote monitor of vital signs and communicating with patients by WeChat. We achieved the aim of our staff zero incidence of infection.
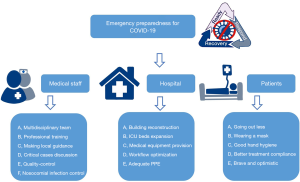
In summary, as an emergency response to the newly infectious diseases such as COVID-19, temporary designated hospitals are helpful for facing the challenge from overflowing patients. Our suggestions might be suitable for general hospitals with several separate buildings which can select one building to set up special wards as “designated hospital”. (I) Facilities must be considered to meet the demands of the large amount of patients care, especially in oxygen supply, ventilator, PPE and medicine supplement, etc.; (II) once the staff in local hospital were shortage, the support from outside medical rescue teams should be considered; (III) teamwork is the key factor to care the patients safely and the effective coordination and communication between different disciplinary medical staff were the main ways to care patients efficiency and high quality; (IV) one local clinical practical guidance should be drawn to improve the quality of patients care; and (V) the control of nosocomial infection is extremely important, and psychological intervention and rehabilitation are also indispensable (Figure 2).
The challenge of new emerging infectious diseases will never be stopped. Emergency preparedness for the disaster is very important to control the epidemic in time (7). We hope our experience in Wuhan could provide some useful reference for the control of COVID-19 pandemic.
Acknowledgments
We are grateful to all the medical staffs of our medical rescue team for fighting against COVID-19 together in the last 2 months in Wuhan.
Funding: None.
Footnote
Provenance and Peer Review: This article was a free submission to the journal and has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-97). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang C, Horby PW, Hayden FG, et al. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470-3. [Crossref] [PubMed]
- WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/
- National Health Commission of the People’s Republic of China Dashboard. Available online: http://www.nhc.gov.cn
- Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med 2020;46:854-87. [Crossref] [PubMed]
- Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available online: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- Neo JR, Sagha-Zadeh R, Vielemeyer O, et al. Evidence-based practices to increase hand hygiene compliance in health care facilities: An integrated review. Am J Infect Control 2016;44:691-704. [Crossref] [PubMed]
- Maves RC, Jamros CM, Smith AG. Intensive Care Unit Preparedness During Pandemics and Other Biological Threats. Crit Care Clin 2019;35:609-18. [Crossref] [PubMed]
Cite this article as: Yu Y, Xu C, Zhu C, Li Q, Chen E. Emergency preparedness for COVID-19: experience from one district general hospital in Wuhan. J Emerg Crit Care Med 2020;4:30.