
Spontaneous hemopericardium with fatal tamponade physiology in end-stage renal disease patient on warfarin: a case report
Introduction
Cardiac tamponade (CT) is a medical emergency. Although frequently challenging, timely clinical diagnosis and efficient management are essential elements of successful treatment (1). Acuity is determined by the fluid volume accumulated within the pericardial sac, the accumulation rate and the pericardial compliance (2). In the general population, pericardial effusions of malignant, infectious, idiopathic, hypertensive, ischemic and trauma-related etiology represent the most frequent underlying causes of CT (2). However, in end-stage renal disease (ESRD) patients, uremic (3) and iatrogenic (4) effusions are rendered higher in the differential. With advancements to date, including the evolution of hemodialysis, pericardial involvement in chronic renal failure consists a rare clinical entity. We present a clinical case with dismal outcome to bring again uremic pericardial effusions to the attention of modern clinical providers and to emphasize the fact that this clinical entity should always be considered in pertinent patients.
Case presentation
An 87-year-old male, former smoker, with past medical history significant for ESRD on hemodialysis, severe coronary artery disease requiring multiple percutaneous interventions, paroxysmal atrial fibrillation on warfarin, chronic obstructive pulmonary disease on multiple inhalers, obstructive sleep apnea on continuous positive airway pressure, anemia of chronic disease on erythropoietin and gastro-esophageal reflux with prior gastrointestinal bleeding, presents with severe hypotension, shortness of breath and crushing substernal chest pain radiating to the jaw while undergoing hemodialysis.
Patient has had several admissions the past three months for similar symptomatology, compromising his hemodialysis sessions. His labile blood pressure was attributed to profound autonomic orthostatism for which he was maintained on pre-hemodialysis Midodrine. His substernal chest pain was considered chronic stable angina and Ranolazine was initiated, as a replacement to hypotension-inducing isosorbide mononitrate, whilst sublingual nitroglycerin was also used 4–5 times per week with moderate relief. Patient was known to have a bare metal stent placed to 2nd obtuse marginal artery four years ago as well as drug-eluding stents to left circumflex artery four years ago and two years later for new de novo lesion. Over the past three months, myocardial ischemia was ruled out by left heart catheterization, which indicated left dominant coronary circulation, non-obstructive coronary artery disease and stents patency. Transthoracic echocardiogram was significant for normal atrial and ventricular size and thickness, absence of wall motion abnormalities, left ventricular ejection fraction of 65% and moderate aortic stenosis with aortic valve area of 1.4 cm2 and trans-aortic pressure gradient of 13 mmHg. No pericardial effusion was noted. Pharmacologic stress test was also performed with normal perfusion, normal left ventricular function and zero summed stress, rest and difference scores. Atherosclerotic calcifications in aorta and coronary arteries were noted.
During current presentation, patient was found tachycardic and tachypneic, with systolic blood pressure of 80 mmHg while maintaining oxygen saturation 99% on room air. Physical exam was remarkable only for irregularly irregular heart rhythm and mild bilateral crackles. Patient appeared euvolemic without pericardial knock or friction rub, gallop, murmur, jugular venous distention or peripheral edema. The electrocardiogram demonstrated irregularly irregular rhythm with heart rate 109 beats per minute but no other axis, QRS or ST segment abnormalities. Electrical alternans was completely absent (Figure 1). Chest X ray revealed unchanged cardiomegaly, left basilar pleural effusion versus atelectasis and low lung volumes without evidence of heart failure or pneumothorax (Figure 2). Troponin I was 0.034. The remaining labs were significant for mild leukocytosis of 11.6 per microliter, hemoglobin 8.6 grams per deciliter and hematocrit 26.8% and supra-therapeutic international normalized ratio (INR) of 5.14 with partial thromboplastin time (PTT) of 65.1 s. Creatinine was 5.43 mg/dL and blood urea nitrogen 34 mg/dL without other major electrolyte abnormalities. Patient was admitted to medicine and was shortly evaluated by cardiologist who recommended withholding of warfarin, as well as endocrine, infectious and malignancy work-up for unjustified supra-therapeutic INR, and right heart catheterization following INR normalization. Provided negative cardiac work-up from recent hospitalizations, new transthoracic echocardiogram or other cardiac work-up was deferred.
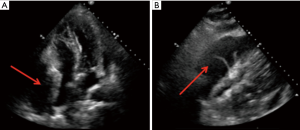
The following days, despite resolution of his chest pain, patient was complaining of persistent dizziness as well as new-onset odynophagia. He was managed with fluid boluses while Midodrine dose was increased due to intermittent hypotension. His troponin I peaked at 0.2 whereas INR and PTT continued to rise up to 5.7 and 72.9 s, respectively. Hemodialysis was deferred. On hospital day 4, patient was transferred to the intermediate medical care unit in the setting of persistent hypotension with syncope. New-onset severe abdominal pain, worsening leukocytosis to 16.6 and transaminitis (AST 1,859 and ALT 1,661 units per liter) concerning for hepatocellular ischemia were also noted. Right upper quadrant ultrasound revealed diffusely echogenic liver consistent with hepatic steatosis or chronic liver disease; hepatic, portal and splenic vasculature were found with normal directional and spectral flow. Chest X ray was significant for unchanged retrocardiac opacity. Infectious work-up proved to be negative but patient was already started on prophylactic broad-spectrum antibiotics for suspected septic shock of unidentified source. Fluid intake was liberalized. On hospital day 5, patient’s clinical status continued to deteriorate necessitating his transfer to the medical intensive care unit. Norepinephrine, and subsequently, Vasopressin infusions were started in the setting of persistent hypotension with SBP 40–60 s mmHg. Point of care echocardiogram revealed a large pericardial effusion with right atrial and ventricular collapse (Figure 3) consistent with CT. Shortly thereafter, and upon preparation for emergent pericardiocentesis, patient went to pulseless electrical activity (PEA) arrest with return of spontaneous circulation (ROSC) in 15 min. He was intubated for airway protection. Patient sustained a second PEA arrest during ultrasound-guided pericardiocentesis with ROSC in 4 min. Pericardial drain was left in place with 320 mL bloody fluid. Epinephrine infusion was started. Cardiothoracic surgery was consulted for pericardial window but family opted for non-operative management. One hour later, patient succumbed to a subsequent ventricular fibrillation arrest. Cardiopulmonary resuscitation was begun but the code was terminated at family’s request.
Limited autopsy to neck and chest was performed revealing small pericardial effusion with dusky red pericardial surface covered with abundant fibrinous exudate and small thrombi without prominent inflammatory component. No gross lesions were identified in the right and left ventricular walls. Calcified atherosclerotic plaques were noted in coronary arteries conferring 20% stenosis in right coronary and left main arteries, and 30% stenosis in left anterior descending and left circumflex arteries, respectively. Stents were found patent. Marked pulmonary parenchyma congestion with patent vasculature was also noted. Pathological diagnosis was identified as acute heart failure in the setting of CT.
Discussion and conclusions
CT physiology stems from an accumulating pericardial effusion or a compressing extra-pericardial factor that raises the intra-pericardial pressure beyond the atrial pressure, impeding venous return, adequate cardiac filling, and thus, hemodynamics (1). Clinically, CT presents as obstructive shock with predominance of Beck’s triad, consisted of hypotension, jugular vein distention and muffled heart sounds but at times, non-specific symptoms, such as abdominal pain or odynophagia, must raise suspicion in the appropriate clinical setting (3,4). As long as other causes of shock have been ruled out, CT imposes a low cardiac output state, with low mean arterial pressure, low pulse pressure (thread pulse), and a compensatory increase of the sympathetic response, with tachycardia and increased systemic peripheral resistance. Elevated cardiac filling pressures (mainly in the right side), equalization of diastolic pressure across all cardiac chambers and loss of the normal “y” descent of the jugular venous pressure waveform are typical of CT. Pericardial friction rub, pulsus paradoxus and Kussmaul sign might be also present. Electrocardiographically, diffuse ST segment elevation with reciprocal ST depression in aVR might be evident. With increasing effusions, low voltage QRS complexes (<0.5 mV in limb leads), T wave inversions and electrical alternans might evolve (5). Radiographically, an enlarged cardiac silhouette should raise concerns for the existence of large pericardial effusion. A pericardial fat stripe, left-sided pleural effusion, and an increase in transverse cardiac diameter with clear lung fields are specific but not sensitive signs. Echocardiographically, the diagnostic gold standard, CT is confirmed by the presence of a large pericardial collection combined with early diastolic collapse of the right ventricle and/or late diastolic collapse of the right atrium in the apical four-chamber or subcostal view (6). Cardiac computed tomography and magnetic resonance imaging are second-line alternatives to echocardiography, although both are considerably less cost-effective and more time-consuming (7,8).
Although frequently challenging, timely clinical diagnosis and efficient management of CT are essential elements of its successful treatment (1). Pertinent literature identifies malignant, infectious, idiopathic, hypertensive, ischemic and trauma-related pericardial effusions among the most frequent underlying causes of CT (2). However, in ESRD patients, uremic and iatrogenic effusions following an invasive medical (e.g., anticoagulation) or surgical procedure are rendered higher in the differential (9). Although we were able to reach a diagnosis for our patient (pericardial effusion with CT), the exact pathophysiology that led to his terminal pathology as well as the evolution timeline of his pericardial effusion remain ambiguous. Unfortunately, due to the emergence of our patient’s situation with recurrent codes, a pericardial fluid analysis was not sent to facilitate definitive diagnosis. Due to hemodialysis-induced hypotension and consequent hemodialysis intolerance, our patient had received inadequate dialysis over the previous 3 months. This fact, in conjunction with his presumed higher catabolic activity in the setting of his multiple comorbidities and the rough granular fibrinous pericardial surface found in autopsy, makes uremic pericardial effusion the most likely underlying cause. On the other hand, someone could advocate that the lack of chronic pertinent signs (pericardial friction rub, EKG or ECHO changes) and the relatively small amount of pericardial fluid drained, brings a more abrupt pathology higher in the differential. Provided the hemorrhagic nature of his pericardial fluid and an unexplained INR of 5.14 upon admission, a sudden hemopericardium in the setting of a supratherapeutic INR could also represent the underlying cause. Sajawal et al. (10), summarizes 11 cases of significant hemopericardium published in the literature where warfarin was deemed to be the culprit. Due to his paroxysmal atrial fibrillation, our patient had a CHA2DS2-VASc score 4 which attributes a 4.8% stroke risk per year. While this is a high risk to justify therapeutic anticoagulation in most patients, our patient’s bleeding risk was also high supporting further the aforementioned assumption (ATRIA score of 10 with 5.8% annual risk of hemorrhage, HAS-BLED score of 5 with 9.1% risk, and HEMORR2HAGES score of 6 with 12.3% risk of bleeding per 100 patient-years of warfarin). This hypothesis does not rule out though the co-existence of uremic pericardial effusion either, as there are several cases of uremic pericarditis with tamponade and hemorrhagic fluid in the absence of therapeutic anticoagulation (11). Of note, our patient did not carry a prior diagnosis of heart failure and had no evidence of fluid accumulation elsewhere. He was experiencing obstructive shock in the setting of rapid pericardial effusion with tamponade physiology.
The indolent clinical course of our patient in the setting of multiple co-morbidities as well as the modern mentality of cost-effectiveness and testing minimalism obscured a timely diagnosis. We do understand the limitation conferred by the lack of definitive microscopic or histologic diagnosis; however, the purpose of this manuscript extends beyond the demonstration of a medical diagnosis. We present this case, first and foremost, to raise awareness that early recognition of pericardial effusions can prevent life-threatening complications, spur urgent intervention, and save lives. Uremic pericardial effusion, common at one time among dialysis patients, has become a rare entity in recent years making its timely recognition by recent generations of health care providers truly challenging (12-14). With earlier dialysis initiation, better dialysis prescription, and more efficient dialyzer membranes, incidence has substantially decreased in chronic hemodialysis patients from 12.5–41% to 5–20%, and in the past decade, to <5% (15). The exact mechanism remains unknown but a uremia-induced pro-oxidant, inflammatory state has been suggested in the literature (16). Other theories implicate electrolyte and acid-base derangements, toxic metabolites and nitrogenous metabolic end products (16). Clinicians should maintain a high level of suspicion for uremic pericardial effusions, especially in patients with progressing azotemia; efforts should focus on restoring intensive hemodialysis sessions for the effusion to abate; nevertheless, in cases refractory to intensive dialysis, alternate forms of medical or surgical therapy should be sought early on (17). When signs of pericardial effusion are manifested, patients often progress rapidly to CT (18). Ultrasound- or fluoroscopy-guided pericardiocentesis, pericardial window or anterolateral pericardiectomy are potential measures in controlling pericardial effusion and preventing fatalities (19). Secondly, we aim at highlighting the fact that critical clinical situations evolve rapidly and our management does need to be tailored accordingly. Our decision-making needs to be based on current data and should not be affected by the mentality of always performing the absolutely necessary work-up for the sake of minimizing medical costs. In addition, complying with updated guidelines is highly recommended but individualized treatment plans have the priority in patients with complicated pathologies and opposing risk factors; perhaps further deliberation on the risk benefit ratio of therapeutic anticoagulation in our patient might have prevented this effusion. Extrapolating the specifics of this case to the general population, it would not be unreasonable the existence of new guidelines with stricter criteria on the initiation of therapeutic anticoagulation in ESRD patients. Last but not least, we cannot highlight enough the importance of point-of-care echocardiography for very specific clinical questions redefining the differential diagnosis at critical times and facilitating prompt directed treatment.
Acknowledgments
We would like to thank Mr. David Flynn, MS (LIS) for verifying the integrity of this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient’s health care proxy for publication of this manuscript. The consent form is held by the authors and is available for review by the Editor-in-Chief.
References
- Spodick DH. Acute cardiac tamponade. N Engl J Med 2003;349:684-90. [Crossref] [PubMed]
- Sánchez-Enrique C, Nuñez-Gil IJ, Viana-Tejedor A, et al. Cause and Long-Term Outcome of Cardiac Tamponade. Am J Cardiol 2016;117:664-9. [Crossref] [PubMed]
- Jacob S, Sebastian JC, Cherian PK, et al. Pericardial effusion impending tamponade: a look beyond Beck's triad. Am J Emerg Med 2009;27:216-9. [Crossref] [PubMed]
- Imazio M, Gaita F, LeWinter M. Evaluation and Treatment of Pericarditis: A Systematic Review. JAMA 2015;314:1498-506. [Crossref] [PubMed]
- Eisenberg MJ, de Romeral LM, Heidenreich PA, et al. The diagnosis of pericardial effusion and cardiac tamponade by 12-lead ECG. A technology assessment. Chest 1996;110:318-24. [Crossref] [PubMed]
- Kearns MJ, Walley KR. Tamponade: Hemodynamic and Echocardiographic Diagnosis. Chest 2018;153:1266-75. [Crossref] [PubMed]
- Restrepo CS, Lemos DF, Lemos JA, et al. Imaging findings in cardiac tamponade with emphasis on CT. Radiographics 2007;27:1595-610. [Crossref] [PubMed]
- Kolski BC, Kakimoto W, Levin DL, et al. Echocardiographic assessment of the accuracy of computed tomography in the diagnosis of hemodynamically significant pericardial effusions. J Am Soc Echocardiogr 2008;21:377-9. [Crossref] [PubMed]
- Sagristà-Sauleda J, Mercé J, Permanyer-Miralda G, et al. Clinical clues to the causes of large pericardial effusions. Am J Med 2000;109:95-101. [Crossref] [PubMed]
- Sajawal Ali M, Mba BI, Ciftci FD, et al. Bleeding heart: a case of spontaneous hemopericardium and tamponade in a hyperthyroid patient on warfarin. BMJ Case Rep 2016. [Crossref] [PubMed]
- Zakynthinos E, Vassilakopoulos T, Politis P, et al. Uremic pericarditis with tamponade following prolonged continuous hemofiltration. Intensive Care Med 2001;27:1958-9. [Crossref] [PubMed]
- Morin JE, Hollomby D, Gonda A, et al. Management of uremic pericarditis: a report of 11 patients with cardiac tamponade and a review of the literature. Ann Thorac Surg 1976;22:588-92. [Crossref] [PubMed]
- Sadjadi SA, Mashahdian A. Uremic pericarditis: a report of 30 cases and review of the literature. Am J Case Rep 2015;16:169-73. [PubMed]
- Alpert MA, Ravenscraft MD. Pericardial involvement in end-stage renal disease. Am J Med Sci 2003;325:228-36. [Crossref] [PubMed]
- Bentata Y, Hamdi F, Chemlal A, et al. Uremic pericarditis in patients with End Stage Renal Disease: Prevalence, symptoms and outcome in 2017. Am J Emerg Med 2018;36:464-6. [Crossref] [PubMed]
- Rehman KA, Betancor J, Xu B, et al. Uremic pericarditis, pericardial effusion, and constrictive pericarditis in end-stage renal disease: Insights and pathophysiology. Clin Cardiol 2017;40:839-46. [Crossref] [PubMed]
- De Pace NL, Nestico PF, Schwartz AB, et al. Predicting success of intensive dialysis in the treatment of uremic pericarditis. Am J Med 1984;76:38-46. [Crossref] [PubMed]
- Hager EB. Clinical observations on five patients with uremic pericardial tamponade. N Engl J Med 1965;273:304-8. [Crossref] [PubMed]
- Bataille S, Brunet P, Decourt A, et al. Pericarditis in uremic patients: serum albumin and size of pericardial effusion predict drainage necessity. J Nephrol 2015;28:97-104. [Crossref] [PubMed]
Cite this article as: Shoni M, Rodriguez G. Spontaneous hemopericardium with fatal tamponade physiology in end-stage renal disease patient on warfarin: a case report. J Emerg Crit Care Med 2020;4:3.




