Avoiding perioperative oxygen debt
Abstract: Perioperative management of high-risk surgical patients is a complex and complicated process. Hemodynamic instability can inflict vital organ hypoperfusion that can have several serious consequences, mainly due to cellular oxygen debt. Therefore, adequate monitoring guided early interventions are inevitable to avoid serious postoperative complications. However, conventional indices, including heart rate, blood pressure, skin temperature and urine output have limited value in diagnosing compensated shock. Therefore, advanced hemodynamic monitoring may become necessary when in addition to cardiac output other measures of oxygen delivery are also taken into account during treatment. However, any alteration that aims to affect macrocirculation only makes sense if it is followed by improved microcirculatory perfusion and adequate oxygen delivery to the cells. Putting the puzzle of hemodynamic stabilization together requires a complex, holistic approach. The purpose of this review is to discuss the holistic approach of multimodal, individualized monitoring that can help to avoid perioperative oxygen debt in high risk surgical patients.
Keywords: High risk surgery; oxygen debt; oxygen delivery; oxygen consumption; hemodynamic monitoring
Received: 03 August 2019; Accepted: 16 September 2019; Published: 10 January 2020.
doi: 10.21037/jeccm.2019.09.05
Introduction
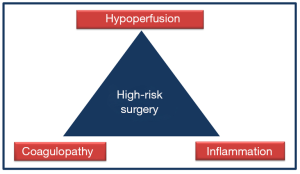
Perioperative management of high-risk surgical patients is a complex and complicated process. Hemodynamic instability can inflict hypoperfusion that can have several serious consequences, mainly due to cellular oxygen debt. Therefore, adequate monitoring guided early interventions can potentially avoid adverse outcomes. On the contrary, inadequate management of hypoperfusion and/or delayed interventions to correct or to prevent surgery induced tissue damage and its consequences may lead to postoperative multiple organ dysfunction (1). Fortunately, the “3 deadly pillars” of: hypoperfusion, coagulopathy and inflammation (Figure 1), can potentially be avoided and treated in time with the help of careful assessment of certain physiological parameters and when these parameters are put in context.
Perioperative goal-directed therapy refers to the hemodynamic optimization of fluids, vasopressors, and/or inotropes to predefined physiological targets in order to maintain or restore sufficient oxygen delivery to tissues (2).
However, conventional indices including heart rate, blood pressure, skin temperature and urine output have limited value in diagnosing compensated shock (3). Therefore, advanced hemodynamic monitoring may become necessary when in addition to cardiac output other measures of oxygen delivery are also taken into account during treatment. It is also important to note that apart from optimizing certain parameters of global oxygen delivery, monitoring oxygen consumption and/or tissue perfusion may also be necessary in order to test the efficacy of treatment (4). This requires a holistic approach that is termed the “multimodal, individualized concept”, which requires some kind of a paradigm shift from protocolized care, in which target parameters are often inappropriate and targets defined in an arbitrary manner.
The purpose of the current review is to describe the concept of multimodal, individualized hemodynamic management that can be used to detect and treat oxygen debt in high-risk surgical patients.
Pathophysiological background
The most important role of the cardio-respiratory system is to deliver adequate amount of oxygen to the cells to match their metabolic demand. Adequate tissue oxygenation depends on the balance between oxygen delivery (DO2) and consumption (VO2) (Figure 2) (5,6).
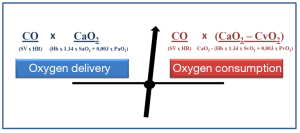
During major surgical procedures three factors have pivotal importance: (I) patient related factors, such as decreased myocardial contractility; (II) surgery-induced conditions: bleeding, hypovolemia, and (III) anesthesia related complications such as hypoxia, vasoplegia caused relative hypovolemia, inadequate depth of anesthesia, etc. These can impair oxygen delivery—both cardiac output and/or arterial oxygen content—to the tissues. There are several compensatory mechanisms to improve DO2 in order to maintain adequate tissue oxygenation and to keep VO2 constant. However, unless the cause and the consequences of this imbalance are treated the organism’s reserves become exhausted, hence without intervention further decrease in DO2 will inevitably cause insufficient VO2 and oxygen uptake by the cells. The latter will then initiate anaerobic cellular metabolism, which can be detected by high lactate levels and metabolic acidosis (7). The main goal of resuscitation while regaining balance of DO2/VO2, is to reestablish aerobic metabolism and avoid or treat oxygen debt.
Oxygen delivery targeted hemodynamic therapy
One can improve DO2 via several measures, from fluid resuscitation (CO) to oxygen therapy or blood transfusion (CaO2) just to name a few. However, each of the potential therapeutic measures can have adverse effects, hence should be considered as a double edge sword. Therefore, to avoid complications adequate resuscitation end points should be applied.
Targeting cardiac output and/or stroke volume
Several studies applied CO or SV “optimization” strategies when testing the efficacy of goal directed therapy (8,9). However, these are not identical parameters and from these studies it is unclear which the better target to follow?
Therefore, in two bleeding-resuscitation porcine animal experiment models we compared the efficacy of CO vs. SV guided resuscitation (10,11). After recording baseline physiological data, bleeding was started and continued until SV index (SVI) showed a 50% reduction. After a short period of stabilization resuscitation was guided by cardiac index (CI) or SVI and continued to reach baseline values. Animals in the CI-group remained under-resuscitated as indicated by lower central venous oxygen saturation (ScvO2), elevated SV variation (SVV) and increased central venous-to-arterial pCO2 difference (dCO2), meanwhile in the SV-group these parameters normalized. The “normalization” of CI in the CI-group occurred due to the persistent tachycardia, inflicted by the effects of bleeding on the autonomic nervous system, and not as the result of fluid resuscitation. We concluded that an SVI-based treatment algorithm may be more beneficial and is closer to physiology then a CI-based model. Nevertheless, a comparison of this kind in the clinical setting is yet to be done.
SVV or pulse pressure variation (PPV) as indicators of fluid responsiveness
In addition to fixed values, the so-called dynamic tests of fluid responsiveness, such as SVV or PPV can be used to determine fluid responsiveness (12,13). To discuss it in further details is beyond the task of the current article, but these parameters serve as very important tools in the individualized multimodal approach, hence mentioning them is very important.
Venous-to-arterial CO2 gap as a measure of global blood flow
A fundamental problem with any goal directed resuscitation is that we should adapt the target values to the patients’ individual needs—one size does not fit all. One of the useful alternatives to help this process is the assessment of the difference of central venous-to-arterial pCO2 gap (dCO2), which can be easily calculated from simultaneously sampled arterial and central venous blood gas analysis. Increased dCO2 was first reported 30 years ago in patients undergoing cardio-pulmonary resuscitation (14,15). There are several reports confirming the phenomenon of increased dCO2 in pathologies when there is low CO (16,17). The detailed physiological explanation is beyond the scope of the current article, but briefly during the hydrolysis of ATP to ADP lactic acid is produced that is buffered by bicarbonate and this will increase CO2 production (18). Therefore, based on the Fick principle decreased CO and stagnation of blood flow in the microcirculation, will result in increased dCO2 (19). It has also been shown to predict patient outcomes. High dCO2 before surgery was accompanied by increased mortality (36%) as compared to patients whose dCO2 values were in the normal range (4.5%) (20). The same holds true for patients who, after surgery are admitted to the ICU with elevated dCO2 (36 mmHg) and they also had more postoperative complications (21).
Optimizing DO2
Perioperative goal directed management to optimize oxygen delivery is not a new concept. Schultz in 1985 and later Shoemaker in his ground breaking trial used pulmonary artery catheter to monitor cardiac index and to guide interventions and targeted supra-normal values during surgery (22,23). Since then several trials have been conducted on different patient populations and various outcome parameters including mortality, morbidity, length of stay, specific postoperative complications were examined. Most of the studies applied an approach to affect oxygen delivery by targeting MAP, CI or PPV. The most important finding of these trials was that the number of postoperative complications and also the number of patients with complications were reduced by almost 50% in high-risk surgical patients (24,25). Salzwedel et al., has shown that patients undergoing abdominal, mainly bowel surgery benefited the most from this approach (25). Another important observation was, that more than 40% of patients needed dobutamine administration to improve CO, while no patients were given positive inotropic agents in the control group. These data are in accord with the results of another DO2-optimization trial in which preoperative DO2 was targeted and 40% of patients were administered dobutamine as compared to none in the control group (26). The authors also point out that in addition to the observed benefits of reduced postoperative morbidity, dobutamine may inflict parasympathetic dysfunction that should closely be observed (26). One meta-analysis showed that perioperative GDT was effective in reducing postoperative complications also in cardiac surgical patients, but failed to show the same benefit in vascular surgery (27). Cecconi et al., reported in a systematic review that early GDT in high-risk surgical patients, where the predicted mortality was higher than 20%, had significant benefit in reducing rates of complications and mortality, but could not prove it in lower risk population (28). In a meta-analysis, which assessed goal-directed therapy (GDT) based on dynamic parameters found that it was associated with a significant decrease in postoperative morbidity (29,30). On the contrary, Zhang and colleagues examined the effect of goal directed fluid management on postoperative ileus; were not able to prove significant reduction of length of stay, 30-day complication rate and mortality (31). Furthermore, in a very recent review, where authors investigated goal directed therapy, were unable to conduct a meta-analysis due to the vast amount of clinical heterogeneity (32).
In conclusion, there is no universally accepted hemodynamic target that could serve as a single parameter to be treated at present. Regarding the values that are considered as ‘normal’ should also be dealt with caution as they may vary from patient to patient and from situation to situation. One solution could be that parameters of DO2 and VO2 are put together and analyzed in context.
DO2-targeted and VO2-verified hemodynamic management: putting the puzzle in context
Solving this very complex hemodynamic puzzle is not easy and for adequate evaluation it is inevitable to put most of the measurable elements of DO2, VO2, tissue perfusion together (33).
Mixed or ScvO2 as parameters of global oxygen extraction
Mixed venous oxygen saturation (SvO2) and its surrogate, ScvO2 are frequently used methods to evaluate global relationship between VO2/DO2. ScvO2 is an easily obtained blood gas parameter taken from an already in situ central venous catheter, which is most often standard procedure in most high-risk surgical patients. Although the absolute values of ScvO2 are higher than SvO2 but they are able to track changes in a similar manner (34). The use of pulmonary artery catheters has dramatically declined in the everyday practice over the last decades, which explains in part why ScvO2 is used more frequently at the bedside (35-37). Venous oxygen saturations are mainly affected by hemoglobin, SaO2, CO and VO2. Therefore, changes in ScvO2 can potentially indicate clinically significant anemia, hypovolemia, impaired myocardial contractility, but can also be affected by sedation, fever or pain or any other factors that influence VO2/DO2 (38). A very important consideration when interpreting venous saturations is that both high and low values can indicate alarming signals and can contribute to worse outcomes. Patients admitted with sepsis to the emergency department were found to have an almost equally high mortality rate of around 40% when their ScvO2 was less than 70% or higher than 90%. In the first case it was likely due to inadequate oxygen delivery in the latter instance it could be the result of impaired oxygen uptake (39). Therefore, high ScvO2 values should be interpreted as insufficient oxygen extraction due to microcirculatory shunting that is frequently seen in sepsis (40).
Therefore, ScvO2 is a very useful and important physiological parameter, but for the appropriate interpretation additional measures are necessary, such as lactate, dCO2, and putting it in the context with advanced invasive hemodynamic monitoring derived indices.
Lactate as a measure of tissue hypoxia
Elevated lactate levels often indicate metabolic acidosis, which is an important signal of anaerobic metabolism and considered as a serious sign of deterioration and cellular oxygen debt. The importance of hyperlactatemia has been confirmed by several studies showing its good prognostic value in several clinical scenarios including the high-risk surgical patient (41,42). Elevated lactate levels on admission to the ICU corresponded to higher mortality, while low levels or better lactate clearance resulted in better outcome (43). Lactate production changes rapidly in accord with the changes in metabolism. During one of a recent bleeding-resuscitation experiment we observed that significant changes occurred within a timeframe of 20 minutes, suggesting that frequent blood gas analysis, which includes the determination of lactate, may be beneficial in monitoring progression and evaluate the efficacy of the interventions. Of note, it is important to bear in mind that fluid resuscitation on its own can have a diluting effect on lactate levels hence it may give a false positive signal of improvement in this scenario.
The multimodal, individualized approach
We can conclude at this point that each of the discussed parameters has its merit but on their own they give little if any definite answer for questions like “what is the problem?” and “what to do?” Therefore, putting them into context is inevitable and this approach is supported by strong physiological rationale. Any alteration that aims to affect macrocirculation only makes sense if it is followed by improved microcirculatory perfusion and adequate oxygen delivery to the cells. The appropriate connection between macro- and microcirculation is termed as “hemodynamic coherence” (44). Achieving this is the goal of the “multimodal, individualized” approach (45). During hemodynamic monitoring looking at any given parameter one can only comment on whether these are normal or not in relation to the overall average population. To determine whether these parameters are adequate or not in the individual patient at a given moment in time, requires thorough evaluation of the full clinical picture.
The holistic approach
In principle any parameter that looks abnormal can serve as an alarming signal that something is going wrong or at least needs attention in the patient. On the other hand, when improvement is observed could indicate the effectiveness of our treatment hence can be a comforting sign of successful stabilization. As everything is linked with each other in a way that each variable can be a cause or an effect, putting this puzzle into context is mandatory but could be challenging.
In a very recent prospective randomized clinical trial comparing the effects of colloids and crystalloids during free-flap surgery, the above mentioned “multimodal approach” was applied in both groups (46). A very interesting additional finding in the trial was that detailed hemodynamic evaluation revealed that some patients required a bolus fluid of only 500 mL but some needed almost 5 L, although the length of surgery (6 hours on average) and blood loss did not differ significantly between patients. These patients also needed positive inotropic support in 40% as reported previously (25,28,46). These results underline the huge individual variability in fluid, vasopressor and inotrope requirements and emphasize the need for advanced hemodynamic monitoring guided management in selected cases.
Conclusions
Adverse postoperative outcomes are still common and related mainly to inadequate oxygen delivery to the tissues for whatever reason. Avoiding intraoperative oxygen debt plays a crucial role in improving outcomes of high-risk surgical patients. For that purpose, there are several alternatives from simple, non-invasive continuous monitoring to advanced, invasive hemodynamic assessment. Putting all parameters in context is a very intriguing idea, but the drawback is that it can be cumbersome, costly and requires well trained personnel. Therefore, the challenge of the future is to provide clinician’s tools via which they can select the high-risk patient and choose the appropriate level of monitoring. At the moment we don’t have clear, universally accepted evidence that this approach improves outcomes. However, the strong pathophysiological rationale and the increasing number of papers with positive outcomes may encourage the readers to test this approach in their everyday practice in high risk patients undergoing major surgery.
Acknowledgments
None.
Footnote
Conflicts of Interest: Dr. Molnar receives regular honoraria for being in the Medical Advisory Board of PULSION Maquet, for lectures from Biotest, ThermoFisher Scientific and CytoSorbents. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Shoemaker WC, Appel PL, Kram HB. Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest 1992;102:208-15. [Crossref] [PubMed]
- Cove ME, Pinsky MR. Perioperative hemodynamic monitoring. Best Pract Res Clin Anaesthesiol 2012;26:453-62. [Crossref] [PubMed]
- Goodrich C. Endpoints of resuscitation: what should we be monitoring? AACN Adv Crit Care 2006;17:306-16. [PubMed]
- Benes J, Pradl R, Chyrta I. Perioperative hemodynamic optimization: a way to individual goals. In: Vincent JL, editor. Annual update in intensive care and emergency medicine 2012. New York: Springer, 2012:357-67.
- Vallet B, Tavernier B, Lund N. Assessment of tissue oxygenation in the critically ill. Eur J Anaesthesiol 2000;17:221-9. [Crossref] [PubMed]
- Tánczos K, Németh M, Molnár Z. The multimodal concept of hemodynamic stabilization. Front Public Health 2014;2:34. [Crossref] [PubMed]
- Vincent JL. The relationship between oxygen demand, oxygen uptake, and oxygen supply. Intensive Care Med 1990;16 Suppl 2:S145-8. [Crossref] [PubMed]
- Pearse RM, Harrison DA, MacDonald N, et al. Effect of a perioperative, cardiac output-guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery: a randomized clinical trial and systematic review. JAMA 2014;311:2181-90. [Crossref] [PubMed]
- Zheng H, Guo H, Ye J, et al. Goal-directed fluid therapy in gastrointestinal surgery in older coronary heart disease patients: randomized trial. World J Surg 2013;37:2820-9. [Crossref] [PubMed]
- Németh M, Tánczos K, Demeter G, et al. Central venous oxygen saturation and carbon dioxide gap as resuscitation targets in a hemorrhagic shock. Acta Anaesth Scand 2014;58:611-9. [Crossref] [PubMed]
- Tánczos K, Németh M, Trásy D, et al. Goal-directed resuscitation aiming cardiac index masks residual hypovolemia: an animal experiment. Biomed Res Int 2015;2015:160979. [Crossref] [PubMed]
- Michard F, Teboul JL. Using heart-lung interactions to assess fluid responsiveness during mechanical ventilation. Crit Care 2000;4:282-9. [Crossref] [PubMed]
- Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update. Ann Intensive Care 2016;6:111-22. [Crossref] [PubMed]
- Grundler W, Weil MH, Rackow EC. Arteriovenous carbon dioxide and pH gradients during cardiac arrest. Circulation 1986;74:1071-4. [Crossref] [PubMed]
- Weil MH, Rackow EC, Trevino R, et al. Difference in acid-base state between venous and arterial blood during cardiopulmonary resuscitation. N Engl J Med 1986;315:1616-8. [Crossref] [PubMed]
- Bakker J, Vincent JL, Gris P, et al. Veno-arterial carbon dioxide gradient in human septic shock. Chest 1992;101:509-15. [Crossref] [PubMed]
- Cuschieri J, Rivers EP, Donnino MW, et al. Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med 2005;31:818-22. [Crossref] [PubMed]
- Vallet B, Teboul JL, Cain S, et al. Venoarterial CO2 difference during regional ischemic or hypoxic hypoxia. J Appl Physiol 2000;89:1317-21. [Crossref] [PubMed]
- Lamia B, Monnet X, Teboul JL. Meaning of arterio-venous PCO2 difference in circulatory shock. Minerva Anestesiol 2006;72:597-604. [PubMed]
- Silva JM Jr, Oliveira AM, Segura JL, et al. A large venous-arterial PCO2 is associated with poor outcomes in surgical patients. Anesthesiol Res Pract 2011;2011:759792. [Crossref] [PubMed]
- Robin E, Futier E, Pires O, et al. Central venous-to-arterial carbon dioxide difference as a prognostic tool in high-risk surgical patients. Crit Care 2015;19:227. [Crossref] [PubMed]
- Schultz RJ, Whitfield GF, LaMura JJ, et al. The role of physiologic monitoring in patients with fractures of the hip. J Trauma 1985;25:309-16. [Crossref] [PubMed]
- Shoemaker WC, Appel PL, Kram HB, et al. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94:1176-86. [Crossref] [PubMed]
- Benes J, Chytra I, Altmann P, et al. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study. Crit Care 2010;14:R118. [Crossref] [PubMed]
- Salzwedel C, Puig J, Carstens A, et al. Perioperative goal-directed hemodynamic therapy based on radial arterial pulse pressure variation and continuous cardiac index trending reduces postoperative complications after major abdominal surgery: a multicenter, prospective, randomized study. Crit Care 2013;17:R191. [Crossref] [PubMed]
- Ackland GL, Iqbal S, Paredes LG, et al. Individualised oxygen delivery targeted haemodynamic therapy in high-risk surgical patients: a multicentre, randomised, double-blind, controlled, mechanistic trial. Lancet Respir Med 2015;3:33-41. [Crossref] [PubMed]
- Giglio M, Dalfino L, Puntillo F, et al. Haemodynamic goal-directed therapy in cardiac and vascular surgery. A systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2012;15:878-87. [Crossref] [PubMed]
- Cecconi M, Corredor C, Arulkumaran N, et al. Clinical review: goal directed therapy-what is the evidence in surgical patients? The effect on different risk groups. Crit Care 2013;17:209. [Crossref] [PubMed]
- Benes J, Giglio M, Brienza N, et al. The effects of goal-directed fluid therapy based on dynamic parameters on post-surgical outcome: a meta-analysis of randomized controlled trials. Crit Care 2014;18:584. [Crossref] [PubMed]
- Michard F, Giglio MT, Brienza N. Perioperative goal-directed therapy with uncalibrated pulse contour methods: impact on fluid management and postoperative outcome. Br J Anaesth. 2017;119:22-30. [Crossref] [PubMed]
- Zhang X, Zheng W, Chen C, et al. Goal-directed fluid therapy does not reduce postoperative ileus in gastrointestinal surgery: A meta-analysis of randomized controlled trials. Medicine (Baltimore) 2018;97:e13097. [Crossref] [PubMed]
- Kaufmann T, Clement RP, Scheeren TWL, et al. Perioperative goal-directed therapy: A systematic review without metaanalysis. Acta Anaesthesiol Scand 2018;62:1340-55. [Crossref] [PubMed]
- Tanczos K, Nemeth M, Molnar Z. The Hemodynamic Puzzle: Solving the Impossible? In: Vincent JL (Ed.). Annual Update in Intensive Care and Emergency Medicine. New York: Springer, 2014:355-65.
- Rivers E. Mixed versus central venous oxygen saturation may be not numerically equal, but both are still clinically useful. Chest 2006;129:507-8. [Crossref] [PubMed]
- Chawla LS, Zia H, Gutierrez G, et al. Lack of equivalence between central and mixed venous oxygen saturation. Chest 2004;126:1891-6. [Crossref] [PubMed]
- Reinhart K, Kuhn HJ, Hartog C, et al. Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med 2004;30:1572-8. [Crossref] [PubMed]
- Varpula M, Karlsson S, Ruokonen E, et al. Mixed venous oxygen saturation cannot be estimated by central venous oxygen saturation in septic shock. Intensive Care Med 2006;32:1336-43. [Crossref] [PubMed]
- van Beest P, Wietasch G, Scheeren T, et al. Clinical review: use of venous oxygen saturations as a goal - a yet unfinished puzzle. Crit Care 2011;15:232. [Crossref] [PubMed]
- Pope JV, Jones AE, Gaieski DF, et al. Multicenter study of central venous oxygen saturation (ScvO(2)) as a predictor of mortality in patients with sepsis. Ann Emerg Med 2010;55:40-6.e1. [Crossref] [PubMed]
- Ince C, Sinaasappel M. Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med 1999;27:1369-77. [Crossref] [PubMed]
- Meregalli A, Oliveira RP, Friedman G. Occult hypoperfusion is associated with increased mortality in hemodynamically stable, high-risk, surgical patients. Crit Care 2004;8:R60-5. [Crossref] [PubMed]
- Régnier MA, Raux M, Le Manach Y, et al. Prognostic significance of blood lactate and lactate clearance in trauma patients. Anesthesiology 2012;117:1276-88. [Crossref] [PubMed]
- Husain FA, Martin MJ, Mullenix PS, et al. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg 2003;185:485-91. [Crossref] [PubMed]
- Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Critical Care 2015;19:S8. [Crossref] [PubMed]
- Molnar Z, Szabo Z, Nemeth M. Multimodal individualized concept of hemodynamic monitoring. Curr Opin Anaesthesiol 2017;30:171-7. [Crossref] [PubMed]
- László I, Janovszky Á, Lovas A, et al. Effects of goal-directed crystalloid vs. colloid fluid therapy on microcirculation during free flap surgery: A randomised clinical trial. Eur J Anaesthesiol 2019;36:592-604. [PubMed]
Cite this article as: Leiner T, Tánczos K, Molnar Z. Avoiding perioperative oxygen debt. J Emerg Crit Care Med 2020;4:6.