
Pediatric solid organ injury management: the role of initial hematocrit in lean times
Introduction
Injury is the leading cause of death and disability in children and young adults from ages 1–24 (1). Blunt trauma accounts for over 90% of traumatic mechanisms of injury in children. with blunt abdominal trauma accounting for approximately 10–15% of all blunt mechanisms (2-4). Several anatomic features of the pediatric abdomen make it particularly vulnerable to injury including: proportionately larger solid organs; relatively higher, less ossified rib cage; and limited fat “protection” to absorb the energy of impact (4). The vascularity of the solid organs can contribute to significant hemorrhage when injured resulting in severe morbidity and death. Of the solid organs, the spleen is the most frequently injured by blunt mechanisms. The immunological functions of the spleen in childhood prioritize spleen preservation in this population.
Early guideline development
The seminal research of Douglas and Simpson in 1971 set into motion the practice of non-operative management for isolated spleen injuries (5). Over time, this practice extended non-operative management to all solid organ injuries resulting from blunt trauma. In the 2000 American Pediatric Surgery Association (APSA) guidelines, non-operative management of liver and spleen injuries became the standard of care (6,7). The ASPA guidelines utilized the Grade of Injury as the guide for management. Application of the guideline in terms of outcomes has been reviewed and analyzed in several retrospective and prospective studies with the identification of hemodynamics as a more valuable indicator for management than grade (8,9). By implementing this strategy, significant cost savings could be realized by decreasing length of stay, earlier mobilization, and less lab resource utilization. Additionally, the focus could be placed on those patients requiring resources most urgently (6). Based on this evidence, our trauma program, located in a free-standing Level 1 academic pediatric hospital, developed the following guideline (Figure 1).
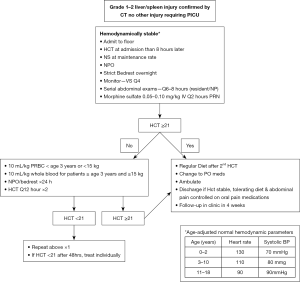
As part of the development, the new practice guideline underwent review by the Pediatric Surgery faculty and the institution’s Clinical Effectiveness Guidelines Committee prior to implementation. The final revision was placed on the institution’s website and incorporated into the Resident Orientation for Pediatric Trauma education.
The presence of a guideline alone does not insure quality care delivery. Compliance with the guideline must be monitored to identify areas of weakness and opportunities for improvement. Review of compliance is required as part of the performance improvement process (PIPS) under the most current accreditation standards presented in the American College of Surgeons Committee on Trauma (ACS-COT) Resource for the Optimal Care of the Injured Patient (10).
Lean Six Sigma definition
Performance improvement (PI) in trauma inherently implies repairing something that is broken whether it be on the patient, department, institution or system level. Equally important, however, is to view the concept of “improvement” as means to enhance value or excellence. One of the fundamental principles of an effective quality program is to continually identify ways in which to improve care delivery and patient outcomes. The lean model of management, first developed by Toyota in the automotive industry, seeks ways to improve efficiency, limit waste and provide a positive customer experience (1). Lean management strategies can be successfully adapted in the healthcare environment as a PI tool to reduce variability and enhance quality, both of which add value and excellence to care delivery (11). Three major lean strategies are particularly applicable to patient management: decrease waste, reduce “waits” and monitor outcomes continuously. By conducting a systematic review of our solid organ injury patient management guidelines, we identified opportunities to reduce variability and costs while improving patient satisfaction.
Lean Six Sigma measurement
All patients admitted in 2017 with an isolated spleen or liver injury (n=33) were reviewed for provider adherence to our guideline using the following metrics: hemoglobin/hematocrit (H/H) collection every 8 hours; diet advancement and out of bed activity orders. Cases with deviations from the guideline were further reviewed for the following metrics: unexpected transfer to the pediatric intensive care unit (PICU), complications (e.g., pleural effusion development) and hospital readmission. Patients who presented 24 hours or more after initial injury were also identified. The following issues were identified in the review:
- Variations in collection times and frequencies of H/H collection;
- Definition of “first” H/H collection;
- Definition of H/H stability in serial draws;
- Earlier diet advancement than recommended by guideline.
Lean Six Sigma analyze
Careful evaluation of patient outcomes in each case with an observed guideline variation identified the opportunity to decrease utilization by modifying the guideline in terms of frequency of phlebotomy draws and the definition of “stability” in serial H/H’s. Concurrent to these findings, additional pediatric trauma research was being conducted in which the relationship between hemodynamic stability and initial hematocrit was studied (12,13). Through several retrospective and prospective studies, an initial hematocrit of 35 was identified as the defining point for guideline direction (12,13). Our trauma program conducted a retrospective review of our institution’s isolated solid organ injury patients previously described utilizing an initial hematocrit of 35 as the criteria for guideline directives. We did not identify any fallouts from application of this parameter. As a result, the following practice guideline was developed (Figure 2).

Lean Six Sigma improve
The proposed guideline was reviewed by both the Trauma Medical Director and the Associate Trauma Medical Director. The guideline has been reviewed and approved by UPMC Children’s Hospital Clinical Effectiveness Guideline Committee. Currently it is posted on our institution’s website and incorporated into the Resident Orientation for Pediatric Trauma education. This guideline will offer both patient and institution satisfiers without compromising quality care. In terms of the former, patients will undergo less phlebotomy experiences, be advanced to a regular diet earlier and have a decreased length of stay. Also, our institution’s catchment area covers a tri-state area; a decreased length of stay allows patients and their families to return to their homes sooner reducing time away from family and work commitments. In terms of the latter, the institution will have less lab costs and overall decreased length of stay. In current healthcare dollars, these changes could result in significant savings as identified in the table below (Table 1).
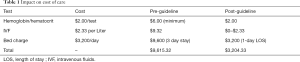
Full table
Lean Six Sigma control
The potential for improved patient satisfaction and cost reduction must not occur at the risk of patient safety and quality outcomes. As part of the lean philosophy of management scheduled monitoring of the guideline via case review will be conducted to insure compliance as well as to identify variations in practice that impact patient safety. Additionally, as part of the monitoring process, the current literature will be reviewed to insure currency with best practice. Ultimately, the goal is the development of a clinical pathway which is an evidence- and consensus-based, standardized patient care plan intended to reduce variability in practice and treatment (14).
Conclusions
The management of pediatric blunt abdominal trauma has undergone a significant evolution in the past decades. Pediatric trauma surgery set the standard for non-operative management of solid organ injuries without compromising patient outcomes. Over time, the focus has transitioned to the evaluation of hemodynamics and ultimately hematocrit trigger points to determine management. By combining evidenced based practice and lean management principles, this approach can result in improved patient and institution satisfaction without compromising quality outcomes.
Acknowledgments
We thank Barbara A. Gaines, MD (Professor, Surgery and Clinical and Translational Science; University of Pittsburgh School of Medicine; Clinical Director, Pediatric Surgery; Director, Pediatric Surgery Training Program; Director, Trauma and Injury Prevention; UPMC Children’s Hospital of Pittsburgh).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Centers for Disease Control and Prevention. National Center for Health Statistics. Leading causes of death and numbers of deaths, by age: United States, 1980 and 2016. Available online: https://www.cdc.gov/nchs
- Leeper CM, Nasr I, Koff A, et al. Implementation of clinical effectiveness guidelines for solid organ injury after trauma: 10-year experience at a level 1 pediatric trauma center. J Pediatr Surg 2018;53:775-9. [Crossref] [PubMed]
- Gaines BA. Intra-abdominal solid organ injury in children: diagnosis and treatment. J Trauma 2009;67:S135-9. [Crossref] [PubMed]
- Streck CJ Jr, Jewett BM, Wahlquist AH, et al. Evaluation for intra-abdominal injury in children after blunt torso trauma: can we reduce unnecessary abdominal computed tomography by utilizing a clinical prediction model? J Trauma Acute Care Surg 2012;73:371-6; discussion 376. [Crossref] [PubMed]
- Douglas GJ, Simpson JS. The conservative management of splenic trauma. J Pediatr Surg 1971;6:565-70. [Crossref] [PubMed]
- Stylianos S. Evidence-based guidelines for resource utilization in children with isolated spleen or liver injury. The APSA Trauma Committee. J Pediatr Surg 2000;35:164-7; discussion 167-9. [Crossref] [PubMed]
- Notrica D. Pediatric blunt solid organ injury: Beyond the APSA guidelines. Curr Surg Rep 2015;3:1-6. [Crossref]
- McVay MR, Kokoska ER, Jackson RJ, et al. Throwing out the "grade" book: management of isolated spleen and liver injury based on hemodynamic status. J Pediatr Surg 2008;43:1072-6. [Crossref] [PubMed]
- Mehall JR, Ennis JS, Saltzman DA, et al. Prospective results of a standardized algorithm based on hemodynamic status for managing pediatric solid organ injury. J Am Coll Surg 2001;193:347-53. [Crossref] [PubMed]
- American College of Surgeons Committee on Trauma. Resources for the optimal care of the injured patient. Sixth ed. Chicago, Illinois, 2014.
- Lawal AK, Rotter T, Kinsman L, et al. Lean management in health care: definition, concepts, methodology and effects reported (systematic review protocol). Syst Rev 2014;3:103. [Crossref] [PubMed]
- Golden J, Dossa A, Goodhue CJ, et al. Admission hematocrit predicts the need for transfusion secondary to hemorrhage in pediatric blunt trauma patients. J Trauma Acute Care Surg 2015;79:555-62. [Crossref] [PubMed]
- Golden J, Mitchell I, Kuzniewski S, et al. Reducing scheduled phlebotomy in stable pediatric patients with blunt liver or spleen injury. J Pediatr Surg 2014;49:759-62. [Crossref] [PubMed]
- UPMC Children’s Hospital of Pittsburgh Infonet. Pediatric and Young Adult Clinical Effectiveness Guidelines and Pathways. Available online: https://infonet.upmc.com/ClinicalTools/StandardsOfCare/GuidelinesLiterature/Pages/Pediatric-Young-Adult-Clinical-Effectiveness-Guidelines-Pathways.aspx
Cite this article as: Miller M, Perlick C. Pediatric solid organ injury management: the role of initial hematocrit in lean times. J Emerg Crit Care Med 2019;3:39.


