
Interpreting biomarkers in infectious diseases in intensive care unit: the potential role of procalcitonin
Introduction
Sepsis is now defined as a life-threatening organ dysfunction caused by dysregulated host response to infection, which may be associated with circulatory and cellular/metabolic dysfunction resulting in high risk of mortality (1). The latter condition is referred to as ‘septic shock’. However, it is not only infection, but several other non-infectious type insults that can cause dysregulated inflammatory response resulting in organ dysfunction. Nevertheless, regarding early management of septic patients, as recommended by the Surviving Sepsis Campaign guidelines, the early recognition of infection, adequate antimicrobial therapy and fluid resuscitation may contribute to positive outcomes and survival benefit (2). Although critical illness caused organ dysfunction can be detected via objective signs of organ failure/dysfunction, in the sepsis context the fundamental question is to decide whether the critical illness is due to infection or not?
Unfortunately, diagnosing infection is not easy. ‘Sepsis syndrome’ is a term that was created in a hotel in Las Vegas in 1980, during the designing of the protocol of one of the first prospective randomized trials in sepsis, performed by a group of scientists led by the late Roger Bone (3). Although the study did not result in significant conclusions, a statement paper was later published by the same authors titled “Sepsis syndrome: a valid clinical entity” (4). Based on this paper or for other reasons, but majority of medical society still considers sepsis as a definitive disease. The consequence is that physicians expect a single test with high sensitivity and specificity to diagnose sepsis, and a specific and single ‘anti-sepsis medication’ has also been demanded. By today, it has become clear that neither of these wishes will ever come true.
It soon turned out that the features characterized as systemic inflammatory response (SIRS) based on body temperature, leukocyte count, tachycardia, hypotension, are very general terms, more-or-less true for any hospitalized patient, never mind those needed to admitted to the intensive care unit (ICU). Due to the non-specific nature of these conventional indices, biomarkers have widely been studied in order to improve diagnostic accuracy during the last decades. Procalcitonin (PCT) is one of the most studied biomarkers (5), especially in the field of adequate antibiotic therapy, but the results overall are controversial (6-10).
This confusion is due to the fact that biomarkers reflect a non-specific, individual host response to infection, therefore the results are difficult to interpret. However, inflammatory biomarkers have their own values and limitations, and to understand them, one should understand at least the basics of the immunological background of critical illness, inflammation, sepsis and septic shock.
Dysregulated host response: what does it mean?
It was Janos Selye, originally from Hungary, who in 1936 discovered, that animals exposed to different acute non-specific ‘nocuous’ agents, such as cold, surgery, etc., developed a typical syndrome, which appeared to be independent of the nature of the damaging agent (11). Later he called this condition stress. Today we know, that this non-specific response is directed by the immune system, it is also independent from the insult, let it be infectious or non-infectious in origin, and reflect the patient’s individual response to the injury—exactly the way Selye described stress response.
The immune system consists of two main components, the innate and the adaptive immunity. This complex network relies on the balance between pro-, and anti-inflammatory mechanisms. The innate immunity recognizes a broad spectrum of pathogens via ‘pathogen associated molecular patterns’ (PAMPs), and produces a pro-inflammatory response, in order to eradicate the potentially dangerous invading pathogens. The role of the anti-inflammation (guided by adaptive immunity) is to keep this war localized and/or under control. It was a surprising new aspect that mechanical damage of tissues such as trauma, burns, ischemia-reperfusion, pancreatitis, major surgery, etc., may also result in a cytokine storm. Immune response for a non-infectious insult is referred to as “damage- associated molecular patterns” (DAMPs) (12).
When we are healthy, the antagonistic forces are in balance in our body, as symbolized by yin and yang (Figure 1). In Chinese philosophy, yin and yang describes how antagonistic forces may actually be complementary, interconnected, and interdependent, and how they may give rise to each other as they interrelate to one another. This becomes clear when we concern the acid/base, pro-/anti-coagulation and oxidant/anti-oxidant balance. No-one knows it better than us, critical care physicians, how an imbalance in homeostasis (acid-base) or hemostasis (pro-, anti-coagulation) can cause life threatening situations.
It is the same regarding the inflammatory forces. Normally the balance is maintained between pro-, and anti-inflammation, and they function at a baseline level of activity to protect us from our environment during our everyday life. When we fall ill, both the pro-, and anti-inflammation increases its activity, they act in a parallel manner, the above-mentioned balance is maintained, and after 5–6 days we usually recover from injuries, or community acquired infections, and the activity of our immune system returns to its baseline (13). Why? Because we are healthy. It may sound a paradox, but we are still healthy even when we have fallen ill. This is why the SIRS concept was false, as SIRS is a physiological response, required to overcome the insult. However, in the context of sepsis, pro-inflammatory forces overwhelm anti-inflammation and the response goes out of control, becomes uncontrolled and dysregulated (14). These patients can die due to fulminant septic shock during the early course of their disease.
Diagnosing infection at the bedside—use kinetics over absolute values
As mentioned above, sepsis is not a definitive disease, thus from the patient’s treatment point of view it may be an irrelevant issue whether a given patient is septic or not. The key question is whether the critically ill condition is due to infection or not?
The way it usually works in everyday practice is the following: we recognize that the patient is critically ill via the objective signs of organ dysfunction and commence basic and organ specific resuscitation, regardless of the actual diagnosis, which is often unknown at the time. The main question in this sepsis context is, whether the symptoms are due to infection or not? If infection is highly likely then source control should be initiated as soon as possible (15). However, if infection is unlikely, then antimicrobial therapy, surgery should be withheld due to the undesired adverse effects (15).
Unfortunately, diagnosing infection is not always easy. Although clinical signs are very important but on their own may be insufficient. Classical indicators of infection, such as fever/hypothermia, leukocytosis/leukopenia, tachypnoe, tachycardia and hypotension are non-specific indicators of infection, frequently observed in every critically ill patient with or without infection. Therefore, inflammatory biomarkers have been investigated for decades in order to improve our diagnostic accuracy (5). However, despite the promising results, biomarkers have their own limitations. One of the major misconceptions regarding inflammatory biomarkers is that they are often referred to as ‘sepsis’ or ‘infectious’ biomarkers, which is a big mistake. As it was discussed earlier, both PAMPs and DAMPs can trigger inflammatory immune response in a very similar manner and this is one of the reasons why biomarkers will never have 100% sensitivity and specificity for diagnosing infection or sepsis, and they will never be able to clearly differentiate the inflammatory response for infection from host response for non-infectious insults.
There are more than 200 so called inflammatory biomarkers potentially available today, but undoubtedly PCT and C-reactive protein (CRP) are the most commonly used (5). CRP’s greatest limitation is its long half-life and slow response time. It reaches its maximum concentration around 48 hours after a certain insult, hence follows the change of the patients’ condition with a considerable delay. Moreover, CRP concentrations are elevated in most ICU patients with a huge scatter, making interpretation of the results even more difficult (16).
In contrast, PCT can be detected within 4–6 hours after the initial insult and reaches its peak concentration within 24 hours. In case of adequate treatment (for example in sepsis) or during an uncomplicated course after major surgery, the levels follow a reduction of roughly 50% per day (17). Several studies compared CRP to PCT and found that the latter differentiates bacterial infections from other etiologies with a higher sensitivity and specificity (18), also showed to have a good prognostic value regarding outcome (19). However, interpreting PCT values is not easy either.
Numerous studies report that PCT values correlate with severity of sepsis and septic shock (20). According to Clec’h et al., patients with septic shock had an almost 10 times higher median PCT levels compared to non-septic shock patients (21). If we look at their data more closely, it is important to acknowledge that although there is a statistically significant difference of 14 (0.3–767) in septic shock vs. non-septic shock: 1 (0.15–36) ng/mL, but there is also a huge overlap between the two groups due to the huge scatter of the data, indicating individual variations in the response for the insult. In a subsequent study from the same group the median PCT value in medical vs. surgical patients differed both in SIRS: 0.3 (0.1–1.0) vs. 5.7 (2.7–8.3), and in septic shock: 8.4 (3.6–76.0) vs. 34.0 (7.1–76.0) ng/mL (22). However, the same phenomenon as previously can also be observed, regarding the scatter and overlap of the data. Therefore, one rightly assume that absolute values may significantly differ between populations of patients (both severity and etiology), but regarding the individual patient, a single measurement of PCT is of limited value.
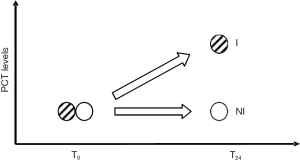
What we may use is the change of PCT over time. Tsangaris et al. evaluated PCT kinetics by measuring its levels daily in patients who had already been treated on the ICU and had a sudden onset of fever (23). A two-fold increase was found from the day before to the day when there was a sudden onset of fever in patients with later proven infection, but there was no change in PCT in patients with fever without the infection. Their results were confirmed by our observational study in which we also found that an increase in PCT from the day before (t-1) to the day when infection was suspected (t0) predicted infection, while in patients in whom infection was not proven, PCT remained unchanged (Figure 2) (24). A PCT increase of >88% from t-1 to t0 that had an area under curve (AUC) of 77% with a sensitivity of 75% (65–84%) and specificity of 79% (60–92%) to indicate infection. It is important to note that neither the absolute values nor the change of white cell count, body temperature or CRP from t-1 to t0 could predict infection and had an AUC of around 50% for all parameters.
Patients requiring prolonged ICU stay most likely to acquire immunosuppression. In these cases, PCT can also be used, but interpretation requires special attention. It has been demonstrated that in patients with secondary peritonitis with a series of recurrent infections, although PCT increased when infections occurred, but the peak values were lower and lower, insult after insult (25). Charles et al. found a similar pattern: during the first infectious insult the mean of PCT concentrations was 55 ng/mL, but despite a similar clinical picture, during the second infectious insult, the mean value was several-fold lower (6.4 ng/mL) (26).
These findings give strong evidence that PCT values are affected by several factors (individual response, etiology, time, etc.), and support the concept of interpreting PCT kinetics instead of choosing a fix cut-off value at the bedside.
PCT-assisted antibiotic therapy
Due to the relatively fast reacting features of PCT kinetics it may be used to assist antimicrobial therapy in several ways.
One of the first studies by Christ-Crain et al. found that antibiotic therapy guided by admission PCT levels resulted in a 50% (44% vs. 83%) reduction in antibiotic exposure in patients admitted to the emergency ward with acute respiratory symptoms (6). Subsequent multicentre trials adjusting antibiotic therapy as indicated by PCT-kinetics also found a 2-day decrease in antibiotic exposure, when antibiotics were stopped in case of a 80–90% decrease in PCT levels (7,27,28). Hochreiter et al. and Schroeder et al. conducted trials on high risk surgical patients with suspected infection. They found significant reduction of antibiotic therapy and shorter ICU stay where PCT-guided therapy was followed during the postoperative period (29,30).
Although, there are other studies that could not find significant benefits of this approach (3,31), but there were important methodological differences between these and the previously mentioned studies. Jensen et al. tested primarily antibiotic escalation and applied fixed values of PCT to indicate intervention (9). Shehabi et al. designed an excellent study, but they expected to detect a 4-day reduction in antibiotic exposure (10). Therefore, although they observed a 2-day benefit in the PCT-group, but the study was underpowered to show such a difference.
Nevertheless, a recent trial-based analysis of the SAPS-trial (28), indicates that the impact of a PCT-assisted antibiotic management approach, not just shortens antibiotic exposure but may also be related to lower in hospital mortality and cost effectiveness (32).
Monitoring treatment efficacy
It goes without saying that monitoring the inflammatory response of critically ill patients at the bedside on a daily basis in a reliable manner, would be of utmost importance. However, there is no such thing as ‘immunometer’ for that purpose that has been agreed upon as gold standard. There are hundreds of biomarkers on the market that could potentially be measured in the clinical routine, but they are expensive tests and data on their usefulness to monitor patient progress is limited. Therefore, each institute should take their choice of the one or two biomarkers for their daily routine they prefer and familiar with. In our institute we use PCT as our monitor to evaluate the patients’ inflammatory response and we measure it on a daily basis in almost every patient. In addition to this we specifically use PCT kinetics to indicate antibiotic appropriateness and to indicate adjunctive therapies in patients with multiple organ failure and persisting cytokine storm.
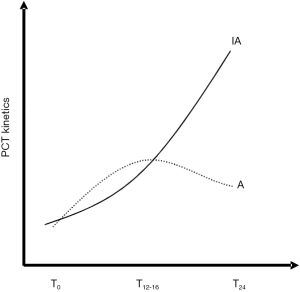
The gold standard for proving antibiotic appropriateness of antibiotic therapy is the microbiological confirmation of the bacteria and its susceptibility. However, to obtain these results may take several days. At the early stage of suspected infection, currently there is no ‘perfect’ clinical sign or laboratory parameter that helps the clinician in deciding about antimicrobial therapy. We conducted an observational study (the EProK-study) where PCT was measured when the first dose of empirical antibiotics was given (t0), and then 8 hourly (t8, t16, t24) during the first 24 hours and then daily (33). There was a significant difference in the kinetics between patients receiving appropriate as compared to those receiving inappropriate antibiotic therapy. Receiver Operating Characteristic analysis revealed that a PCT elevation ≥55% within the first 16 hours (i.e., from t0–t16) had an AUC for predicting inappropriate antibiotic treatment of 0.78 (95% CI: 0.66–0.85), P<0.001; from t0–t24 a ≥70% increase had an AUC of 0.85 (0.75–0.90), P<0.001. These data suggest that early response of PCT within the first 24 hours of commencing empirical antibiotics in critically ill patients may help the clinician to evaluate the appropriateness of therapy, a concept which certainly will have to be tested in the future. Of note, hospital mortality was 35% in the appropriate and 65% in the inappropriate group (P=0.001), which provides further evidence that choosing inappropriate antibiotic therapy may seriously affect survival.
Translating these results into the everyday practice, we recommend two possible approaches. The first is, to measure the percentage change in PCT within the first 24 hours after starting antibiotic therapy and use the EProK data to decide on antibiotic appropriateness. Second, measure PCT level at the commencement of antibiotic therapy, then one more somewhere in between 12–16 hours later and another one after 24 hours. If one observes a ‘roof top’ type kinetics (Figure 3) in contrast to a continuous increase what we found in the inappropriate group in the EProK study, may support that the patient is getting appropriate treatment.
In critically ill patients who have received appropriate resuscitation, source control, and require organ support, but still don’t want to improve, indicating some sort of adjunctive therapy is sometimes considered (34). As there is no frank evidence on the indication of these treatment alternatives, guidelines usually do not recommend these therapies (2). However, clinicians still use immunoglobulins, high volume hemofiltration, plasmapheresis and recently extracorporeal cytokine removal (CytoSorb®, Cytosorbents, Germany), all over the world.
In a recent proof of concept prospective randomized pilot trial, we tested the efficacy of early extracorporeal cytokine removal with CytoSorb in patients with septic shock, with high PCT and high vasopressor need (35). The most dramatic effects as compared to controls were the dramatic decrease in PCT and vasopressor need within the first 12–24 hours of treatment.
Our results suggest that PCT may be a useful biomarker to monitor inflammation/cytokine storm in patients and also to help the physicians to target immunomodulatory adjuvant therapy to patients who may benefit the most.
Conclusions
PCT is a well-established and thoroughly investigated biomarker, which has been shown to help individualizing antibiotic management of critically ill patients that can have several potential benefits on both patient outcomes and cost effectiveness. In addition to its role in antibiotic therapy it may also play an important part in the assessment of the inflammatory response in general, hence in several non-infectious conditions, and in combination with the clinical picture it may help in targeting adjunctive therapy to those patients who would benefit the most.
Acknowledgements
None.
Footnote
Conflicts of Interest: Z Molnar receives lecture honoria from ThermoFisher Scientific. F Hawchar has no conflicts of interest to declare.
References
- Singer M, Deutschman CS, Christopher Warren S, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315:801-10. [Crossref] [PubMed]
- Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 2017;43:304-77. [Crossref] [PubMed]
- Bone RC, Fisher CJ, Clemmer TP, et al. A controlled clinical trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. N Engl J Med 1987;317:653-8. [Crossref] [PubMed]
- Bone RC, Fisher CJ, Clemmer TP, et al. Sepsis syndrome: a valid clinical entity. Methylprednisolone Severe Sepsis Study Group. Crit Care Med 1989;17:389-93. [Crossref] [PubMed]
- Pierrakos C, Vincent J. Sepsis biomarkers: a review. Crit Care 2010;14:R15. [Crossref] [PubMed]
- Christ-Crain M, Jaccard-Stolz D, Bingisser R, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections : cluster-randomised, single-blinded intervention trial. Lancet 2004;363:600-7. [Crossref] [PubMed]
- Bouadma L, Luyt C, Tubach F, et al. Use of procalcitonin to reduce patients ’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet 2010;375:463-74. [Crossref] [PubMed]
- Layios N, Lambermont B, Canivet JL, et al. Procalcitonin usefulness for the initiation of antibiotic treatment in intensive care unit patients. Crit Care Med 2012;40:2304-9. [Crossref] [PubMed]
- Jensen JU, Lundgren B, Hein L, et al. The Procalcitonin And Survival Study (PASS) - A Randomised multi-center investigator-initiated trial to investigate whether daily improve survival in intensive care unit patients. Calculated sample size (target population): 1000 patients. BMC Infect Dis 2008;8:91. [Crossref] [PubMed]
- Shehabi Y, Sterba M, Garrett PM, et al. Procalcitonin algorithm in critically ill adults with undifferentiated infection or suspected sepsis a randomized controlled trial. Am J Respir Crit Care Med 2014;190:1102-10. [Crossref] [PubMed]
- Selye H. A Syndrome produced by Diverse Nocuous Agents. Nature 1936;138:32. [Crossref]
- Zhang Q, Raoof M, Chen Y, et al. Circulating Mitochondrial DAMPs Cause Inflammatory Responses to Injury. Nature 2010;464:104-7. [Crossref] [PubMed]
- Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: From cellular dysfunctions to immunotherapy. Nat Rev Immunol 2013;13:862-74. [Crossref] [PubMed]
- Cavaillon JM, Adib-Conquy M. Bench-to-bedside review : endotoxin tolerance as a model of leukocyte reprogramming in sepsis. Crit Care 2006;10:233. [Crossref] [PubMed]
- Marshall JC. Principles of source control in the early management of sepsis. Curr Infect Dis Rep 2010;12:345-53. [Crossref] [PubMed]
- Lelubre C, Anselin S, Boudjeltia KZ, et al. Interpretation of C-reactive protein concentrations in critically ill patients. Biomed Res Int 2013;2013:124021. [Crossref] [PubMed]
- Samsudin I, Vasikaran SD. Clinical utility and measurement of procalcitonin. Clin Biochem Rev 2017;38:59-68. [PubMed]
- Müller B, Becker KL, Schchinger H, et al. Calcitonin precursors are reliable markers of sepsis in a medical intensive care unit. Crit Care Med 2000;28:977-83. [Crossref] [PubMed]
- Jensen JU, Heslet L, Jensen TH, et al. Procalcitonin increase in early identification of critically ill patients at high risk of mortality. Crit Care Med 2006;34:2596-602. [Crossref] [PubMed]
- Pupelis G, Drozdova N, Mukans M, et al. Serum procalcitonin is a sensitive marker for septic shock and mortality in secondary peritonitis. Anaesthesiol Intensive Ther 2014;46:262-73. [Crossref] [PubMed]
- Clec’h C, Ferriere F, Karoubi P, et al. Diagnostic and prognostic value of procalcitonin in patients with septic shock. Crit Care Med 2004;32:1166-9. [Crossref] [PubMed]
- Clec’h C, Fosse J, Karoubi P, et al. Differential diagnostic value of procalcitonin in surgical and medical patients with septic shock. Crit Care Med 2006;34:102-7. [Crossref] [PubMed]
- Tsangaris I, Plachouras D, Kavatha D, et al. Diagnostic and prognostic value of procalcitonin among febrile critically ill patients with prolonged ICU stay. BMC Infect Dis 2009;9:213. [Crossref] [PubMed]
- Trásy D, Tánczos K, Németh M, et al. Delta procalcitonin is a better indicator of infection than absolute procalcitonin values in critically ill patients : a prospective observational study. J Immunol Res 2016;2016:3530752. [Crossref] [PubMed]
- Rau BM, Frigerio I, Bu MW. Evaluation of procalcitonin for predicting septic multiorgan failure and overall prognosis in secondary peritonitis. Arch Surg 2007;142:134-42. [Crossref] [PubMed]
- Charles PE, Tinel C, Barbar S, et al. Procalcitonin kinetics within the first days of sepsis : relationship with the appropriateness of antibiotic therapy and the outcome. Crit Care 2009;13:R38. [Crossref] [PubMed]
- Schuetz P. Effect of Procalcitonin-Based Guidelines vs Standard Guidelines on Antibiotic Use in Lower Respiratory Tract Infections. JAMA 2009;302:1059-66. [Crossref] [PubMed]
- de Jong E, Oers JA, Van , Beishuizen A, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis 2016;16:819-27. [Crossref] [PubMed]
- Hochreiter M, Köhler T, Schweiger AM, et al. Procalcitonin to guide duration of antibiotic therapy in intensive care patients: a randomized prospective controlled trial. Crit Care 2009;13:R83. [Crossref] [PubMed]
- Schroeder S, Hochreiter M, Koehler T. Procalcitonin (PCT)-guided algorithm reduces length of antibiotic treatment in surgical intensive care patients with severe sepsis: results of a prospective randomized study. Langenbecks Arch Surg 2009;394:221-6. [Crossref] [PubMed]
- Bone RC, Fein AM, Balk RA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992;101:1644-55. [Crossref] [PubMed]
- Kip MMA, Oers JA, Van , Shajiei A, et al. Cost-effectiveness of procalcitonin testing to guide antibiotic treatment duration in critically ill patients : results from a randomised controlled multicentre trial in the Netherlands. Crit Care 2018;22:293. [Crossref] [PubMed]
- Trásy D, Tánczos K, Németh M, et al. Early procalcitonin kinetics and appropriateness of empirical antimicrobial therapy in critically ill patients. A prospective observational study. J Crit Care 2016;34:50-5. [Crossref] [PubMed]
- Becze Z, Molnár Z, Fazakas J. Can procalcitonin levels indicate the need for adjunctive therapies in sepsis ? Int J Antimicrob Agents 2015;46:S13-8. [Crossref] [PubMed]
- Hawchar F, László I, Öveges N, et al. Extracorporeal cytokine adsorption in septic shock: A proof of concept randomized, controlled pilot study. J Crit Care 2019;49:172-8. [Crossref] [PubMed]
Cite this article as: Hawchar F, Molnar Z. Interpreting biomarkers in infectious diseases in intensive care unit: the potential role of procalcitonin. J Emerg Crit Care Med 2018;2:107.



