
Pneumocystis jiroveci pneumonia in patients with toxic epidermal necrolysis
A 63-year-old female was admitted to ICU because of toxic epidermal necrolysis (TEN) caused by sulfonamides eye drops (Figure 1A). Two weeks after ICU admission, she presented with shortness of breath and non-productive cough. Diffuse and bilateral ground glass opacification was observed in chest CT scan (Figure 1B). Aspergillus hyphae was detected in induced sputum sample by fluorescence microscope (Figure 1C), whereas the serum galactomannan (GM) test was negative. Grocott-Gomori stains were performed in bronchoalveolar lavage fluid (BALF) sample soon afterwards. Sample one contained the first 20 mL aspirated fluid in which Pneumocystis jirovecii ascospores and aspergillus hyphae were detected (Figure 1D). The first 20 mL aspirated fluid was discarded in sample two and only ascus was found (Figure 1E).
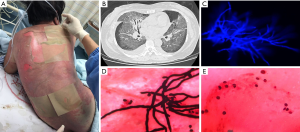
Pneumocystis jirovecii pneumonia (PJP) is rare in patients with TEN. A standardized bronchoalveolar lavage procedure is the most important method to identify the pathogen. The first 20 mL aspirated fluid in BALF, which might contain the pathogen colonized in the main airway, is entirely different from the following samples. Thus, the first sample should be discarded to avoid misinterpretation of the BALF results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Consent was obtained for the use of information and images. The patient’s identity has been kept confidential.
Cite this article as: Yu Y, Zhu C, Zhang Z. Pneumocystis jiroveci pneumonia in patients with toxic epidermal necrolysis. J Emerg Crit Care Med 2018;2:37.


