
Corticosteroids for septic shock: what to do now?
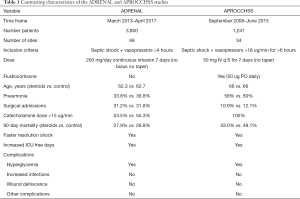
In a recent edition of the New England Journal of Medicine, two large randomized controlled trials report on the use of corticosteroids (hydrocortisone) for the treatment of septic shock (1,2). The Adjunctive Corticosteroid Treatment in Critically Ill Patients with Septic Shock (ADRENAL) trial failed to show a mortality benefit while the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial showed a significant reduction in 90-day mortality. At first glance it would appear difficult to reconcile these contrasting results; however, I believe there is a logical pathophysiological explanation for these apparent discordant findings. Table 1 outlines the major differences and similarities between the two studies. It should be noted that in both the ADRENAL and APROCCHSS studies the median time to resolution of shock and median time to discharge from the ICU were significantly shorter in the hydrocortisone group. This finding has been reported in other studies (3), and indicates that corticosteroids have a biological effect in patients with septic shock. Furthermore, both studies demonstrated that corticosteroids did not increase the risk of complications including infections, myopathy and wound dehiscence. Although hydrocortisone did not improve patient centered outcomes in the ADRENAL study, many would consider the improvement in secondary outcomes beneficial to patients and the health care system. The explanation for the mortality reduction in the APROCCHSS study and not the ADRENAL study is likely explained by the fact that patients in the APROCCHSS study had more severe septic shock (as indicated by a higher vasopressor dose and the higher mortality in the control arm), were older (increased risk of death) and included significantly fewer patients with surgical sepsis. In patients with surgical sepsis, the adequacy and timeliness of source control is likely to have a greater effect on patient outcome than adjunctive therapies. These data suggest that while corticosteroids have a beneficial effect on the pathophysiology of septic shock, these drugs only reduce mortality in the sickest subgroup of patients with septic shock. Furthermore, corticosteroids have no proven benefit in patients with severe sepsis (4). These findings support our belief that patients with severe sepsis and septic shock should be treated with corticosteroids, but not as mono-therapy (5). The addition of intravenous vitamin C and thiamine to corticosteroids enhances the biological effects of corticosteroids with no increase in adverse effects (6,7), and likely improves patient centered outcomes (8).
Full table
It should be noted that in the ADRENAL study hydrocortisone was given as a continuous infusion (200 mg/day) whereas in the APROCCHSS study hydrocortisone was given as intermittent boluses (50 mg q 6 hourly). Different dosing regimens of corticosteroids likely have distinct therapeutic effects mediated by genomic and non-genomic actions. Several studies have compared glycemic control when hydrocortisone is administered as a bolus compared to a continuous infusion (9,10). These studies have demonstrated more severe hyperglycemia with the bolus regimen. It is well known that the effect of corticosteroids on carbohydrate metabolism (glycogenolysis and glucogenesis) parallel those of the drugs anti-inflammatory effects (11). Furthermore, in the study by Loisa et al. blood pressure and vascular resistance tended to be higher in the bolus group (9). We therefore postulate that bolus administration of hydrocortisone will result in higher peak levels with greater glucocorticoid receptor binding and consequently have a greater therapeutic effect than when the drug is administered as a continuous infusion. This difference may be more marked in patients with sepsis who have intrinsic glucocorticoid resistance (12). In addition, in the ADRENAL study a loading dose of hydrocortisone was not given; considering the half-life of hydrocortisone, this implies that it would take between 6 to 12 hours to reach steady state serum concentration. It should also be recognized that in the APROCCHSS study, patients in the hydrocortisone arm were also treated oral fludrocortisone (50 ug daily). It is unclear why the authors added fludrocortisone as hydrocortisone has significant mineralocorticoid activity and the oral absorption of fludrocortisone in patients with septic shock is uncertain. Furthermore, in a previous randomized controlled trial, these authors demonstrated no benefit from the combination of hydrocortisone and fludrocortisone as compared to hydrocortisone alone (13).
In summary, although hydrocortisone positively impacts the course of septic shock this drug appears to reduce mortality only in the sickest sub-group of patients. However, we propose that when combined with intravenous vitamin C and thiamine, hydrocortisone improves outcome in all septic patients. We therefore believe that the era of corticosteroid monotherapy to treat sepsis has ended (5). Furthermore, we suggest that hydrocortisone be administered by bolus dosing rather than as a continuous infusion.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Venkatesh B, Finfer S, Cohen J, et al. Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med 2018;378:797-808. [Crossref] [PubMed]
- Annane D, Renault A, Brub-Buisson C, et al. Hydrocortisone plus fludrocortisone for adults with septic shock. N Engl J Med 2018;378:809-18. [Crossref] [PubMed]
- Sprung CL, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med 2008;358:111-24. [Crossref] [PubMed]
- Keh D, Trips E, Marx G, et al. Effect of hydrocortisone on development of shock among patients with severe sepsis. The HYPRESS Randomized Clinical Trial. JAMA 2016;316:1775-85. [Crossref] [PubMed]
- Marik PE. Glucocorticosteroids as adjunctive therapy for Acute Respiratory Distress Syndrome and Sepsis? Yes, but not as monotherapy. Crit Care Med 2017;45:910-1. [Crossref] [PubMed]
- Barabutis N, Khangoora V, Marik PE, et al. Hydrocortisone and Ascorbic Acid synergistically protect and repair lipopolysaccharide-induced pulmonary endothelial barrier dysfunction. Chest 2017;152:954-62. [Crossref] [PubMed]
- Azari O, Kheirandish R, Azizi S, et al. Protective effects of hydrocortisone, Vitamin C and E alone or in combination against renal-ischemia-reperfusion injury rat. Iran J Pathol 2015;10:272-80. [PubMed]
- Marik PE, Khangoora V, Rivera R, et al. Hydrocortisone, Vitamin C and Thiamine for the treatment of severe sepsis and septic shock: A retrospective before-after study. Chest 2017;151:1229-38. [Crossref] [PubMed]
- Loisa P, Parviainen I, Tenhunen J, et al. Effect of mode of hydrocortisone administration on glycemic control in patients with septic shock: a prospective randomized trial. Crit Care 2007;11:R21. [Crossref] [PubMed]
- Weber-Carstens S, Deja M, Bercker S, et al. Impact of bolus application of low-dose hydrocortisone on glycemic control in septic shock patients. Intensive Care Med 2007;33:730-3. [Crossref] [PubMed]
- Buttgereit F. Standardised nomenclature for glucocorticoid dosages and glucocorticoid treatment regimens: current questions and tentative answers in rheumatology. Ann Rheum Dis 2002;61:718-22. [Crossref] [PubMed]
- Marik PE, Pastores SM, Annane D, et al. Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: Consensus statements from an international task force by the American College of Critical Care Medicine. Crit Care Med 2008;36:1937-49. [Crossref] [PubMed]
- COIITSS Study Investigators, Annane D, Cariou A, et al. Corticosteroid treatment and intensive insulin therapy for septic shock in adults: A randomized controlled trial. JAMA 2010;303:341-8. [Crossref] [PubMed]
Cite this article as: Marik PE. Corticosteroids for septic shock: what to do now? J Emerg Crit Care Med 2018;2:34.


