
Asian intensive care research and education
Progress in the clinical care of patients is dependent on both research and education to translate research findings into changes in clinical practice. While some findings may be generalizable across different populations and settings, recent data suggest that even basic aspects of resuscitation of patients may not be appropriate across all settings. Recently, Andrews et al demonstrated that use of adapted Surviving Sepsis guidelines in a low resource setting resulted in increased rather than decreased mortality (1), suggesting that simple extrapolation of these guidelines from one setting to another may not be reasonable. This is concerning because the research on which international guidelines are based may not be appropriate to Asian settings. It is notable, for example, that of the 655 references that are quoted to support the Surviving Sepsis guidelines, only about 10% pertain to the studies in low and middle income countries (2). To be more confident that research findings are applicable to our patients it is important that research is carried out in these groups of patients and in settings similar to those that exist in Asian ICUs. In short, Asian research is required.
Asia is the world’s largest and most populous continent, being home to more than half the world’s population. It is also extremely heterogeneous in terms of economic development with both extremely high income countries and low income countries. While this provides substantial challenges to research, it also provides opportunities to study the interaction of settings and resources with treatment effects.
The last two decades have demonstrated the importance of collaborative investigator-led research in Intensive Care (3). Although lagging behind groups from Western countries and Australasia, collaborative Intensive Care research groups have been developing in Asia, with Asian (4-6), Chinese (7-9), Japanese (10) groups, amongst others, publishing important data.
The Asian Critical Care Clinical Trials Group (ACCCTG) developed, under the leadership of Professor Younsuck Koh and Dr. Jason Phua, from a collaborative group that carried out the MOSAICS study of sepsis management (11). The study demonstrated that compliance with Surviving Sepsis guidelines was lower in Asian ICUs (7.6% for resuscitation bundle, 3.5% for management bundle) than in studies carried out in North America, South America and Europe (10–31% for resuscitation bundle, 16–36% for management bundle) (12-16). Furthermore, there were substantial differences between low, middle and high income countries in compliance with the resuscitation bundle (2%, 7%, 10% respectively). Despite a disproportionately large proportion of academic centres in the study, a substantial proportion of centres did not have all the facilities required to comply with all core Surviving Sepsis guidelines, for example over 25% were unable to measure arterial lactate within 6 hours.
The ACME study, the first study undertaken by the ACCCTG, was a survey of 1,465 Intensive Care physicians designed to describe physicians’ attitudes to withholding and withdrawal of life-sustaining treatments in end-of-life care (4). In general, Asian ICU physicians’ reported behaviour suggested that they were less likely to limit therapy than their Western counterparts. However there was wide variability across Asia in attitudes and reported practice. Further analysis, by World Bank classification of income, indicated that, compared to physicians from high income Asian countries, those from low-middle income countries were less likely to limit organ support. However, family request to withdraw therapy on financial groups, were more likely to be acceded to in low-middle-income countries (6).
Arabi et al. surveyed ICUs in 20 Asian countries to describe the hospital and ICU organizational characteristics, staffing, procedures and therapies available in the ICU, protocols and policies. Overall only 3% of hospital beds were ICU beds and patients were cared for predominantly in open areas rather than single rooms. Both the ICUs (mean 21 beds) and the hospitals (mean 973 beds) were big and nurse:patient staffing levels were relatively high (1:1 to 1:2 in most ICUs). This is similar or higher than levels reported from some high income countries (17-22), but may reflect an over-representation of teaching hospitals (60%) and referral centres (81%) (5).
Ongoing studies being carried out by the group include a survey of weaning practices and a survey of stress and burnout.
The need for education in Asian intensive care is probably even greater than the need for research. Traditionally, medicine has been taught by apprenticeship. While this method may be effective for long established specialties with limited growth, it is unlikely to meet the demands of a new and rapidly growing specialty like Intensive Care where it is common for there to be an imbalance between masters and apprentices. The problem is exacerbated by the fact that many medical schools do not teach intensive care, so that doctors entering Intensive Care training have very limited skills. In Asia, the even more recent development of Intensive Care as a specialty magnifies the problem. Data from China illustrate the magnitude of the task of training sufficient healthcare workers to staff ICUs. It is estimated that there were 52,000 ICU beds in 2010 (9). Based on the assumption of a need for 20 nurses and 5 doctors for 5 beds, 200,000 ICU nurses and 10,000 ICU doctors need to be trained. However, this is likely to be an underestimate of the number of staff that need to be trained if critically ill patients are to receive adequate care. Critically ill patients are not restricted to the ICU and can be found in many areas of the hospital. Data demonstrate that these patients are poorly treated (23). Thus there is a need for training in the early recognition and initial resuscitation of critically ill patients for all clinical staff. Clearly, an apprenticeship system is unlikely to address these needs and a different approach is required.
The BASIC Collaboration, based at The Chinese University of Hong Kong, is a grouping of acute care specialists from Asia, Europe and Australasia, which has taken a collaborative approach to development of high quality educational course material (24). The collaboration has developed courses to teach both basic and more advanced aspects of acute and intensive care, for both high and low resource settings (Table 1). In the 12 years since the inception of the collaboration, the courses have been taught in over 70 countries and approximately 350 courses are taught per year. Courses are largely based on a flipped classroom approach. Candidates are expected to acquire the necessary knowledge by reading the course manual prior to attending the course. Teaching during the course is then focused on application of knowledge and acquisition of skills, with an emphasis on short case-based lectures and skill stations. Electronic learning is used to supplement some courses. This approach results in a more efficient use of the time of skilled instructors who spend less time on simple knowledge transfer and more time on high value teaching.
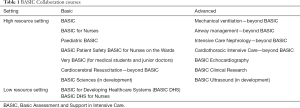
Full table
Mobile smartphone apps are currently available for Very BASIC and BASIC and are provided to all course participants to support them in their clinical practice after completing the course and to facilitate retention of knowledge. In time, apps will be available for all courses. Usage data from the Very BASIC app indicate that a substantial proportion of medical students use the app after qualification, a year after attending the course (25).
All courses are disseminated on a train the trainers basis to ensure maximal time and cost-efficiency. Course material is provided free of charge, in an electronic form, and no license fees are charged. The course content is regularly revised and updated, in response to clinical research findings and feedback from course participants and instructors. Indeed, the constant informal peer-review by the specialists from around the world that teach our courses, is a crucial part of quality improvement.
In summary, a collaborative approach to research and education is essential to improve the care of critically ill patients in Asia.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author is the chair of the Asian Critical Care Clinical Trials Group and the BASIC Collaboration.
References
- Andrews B, Semler MW, Muchemwa L. Effect of an early resuscitation protocol on in-hospital mortality among adults with sepsis and hypotension: A randomized clinical trial. JAMA 2017;318:1233-40. [Crossref] [PubMed]
- Shrestha GS, Kwizera A, Lundeg G, et al. International Surviving Sepsis Campaign guidelines 2016: the perspective from low-income and middle-income countries. Lancet Infect Dis 17:893-5.
- Marshall JC. Global Collaboration in Acute Care Clinical Research: Opportunities, Challenges, and Needs. Crit Care Med 2017;45:311-20. [Crossref] [PubMed]
- Phua J, Joynt GM, Nishimura M. Withholding and withdrawal of life-sustaining treatments in intensive care units in asia. JAMA Intern Med 2015;175:363-71. [Crossref] [PubMed]
- Arabi YM, Phua J, Koh Y, et al. Structure, Organization, and Delivery of Critical Care in Asian ICUs. Crit Care Med 2016;44:e940-8. [Crossref] [PubMed]
- Phua J, Joynt GM, Nishimura M, et al. Withholding and withdrawal of life-sustaining treatments in low-middle-income versus high-income Asian countries and regions. Intensive Care Med 2016;42:1118-27. [Crossref] [PubMed]
- Du B, An Y, Kang Y, et al. Characteristics of critically ill patients in ICUs in mainland China. Crit Care Med 2013;41:84-92. [Crossref] [PubMed]
- Zhou J, Qian C, Zhao M, et al. Epidemiology and Outcome of Severe Sepsis and Septic Shock in Intensive Care Units in Mainland China. PLoS One 2014;9:e107181. [Crossref] [PubMed]
- Du B, Xi X, Chen D, et al. Clinical review: critical care medicine in mainland China. Crit Care 2010;14:206. [Crossref] [PubMed]
- Ogura H, Gando S, Saitoh D, et al. Epidemiology of severe sepsis in Japanese intensive care units: a prospective multicenter study. J Infect Chemother 2014;20:157-62. [Crossref] [PubMed]
- Phua J, Koh Y, Du B, et al. Management of severe sepsis in patients admitted to Asian intensive care units: prospective cohort study. BMJ 2011;342:d3245. [Crossref] [PubMed]
- Ferrer R, Artigas A, Levy MM, et al. Improvement in Process of Care and Outcome After a Multicenter Severe Sepsis Educational Program in Spain. JAMA 2008;299:2294-303. [Crossref] [PubMed]
- Lefrant JY, Muller L, Raillard A, et al. Reduction of the severe sepsis or septic shock associated mortality by reinforcement of the recommendations bundle: a multicenter study. Ann Fr Anesth Reanim 2010;29:621-8. [Crossref] [PubMed]
- Cardoso T, Carneiro AH, Ribeiro O, et al. Reducing mortality in severe sepsis with the implementation of a core 6-hour bundle: results from the Portuguese community-acquired sepsis study (SACiUCI study). Crit Care 2010;14:R83. [Crossref] [PubMed]
- Daniels R, Nutbeam T, McNamara G, et al. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J 2011;28:507. [Crossref] [PubMed]
- Levy MM, Dellinger RPM, Townsend SRM, et al. The Surviving Sepsis Campaign: Results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med 2010;38:367-74. [Crossref] [PubMed]
- Graf J, Reinhold A, Brunkhorst FM, et al. Variability of structures in German intensive care units - a representative, nationwide analysis. Wien Klin Wochenschr 2010;122:572-8. [Crossref] [PubMed]
- Neuraz A, Guérin C, Payet C, et al. Patient Mortality Is Associated With Staff Resources and Workload in the ICU: A Multicenter Observational Study. Crit Care Med 2015;43:1587-94. [Crossref] [PubMed]
- Seynaeve S, Verbrugghe W, Claes B, et al. Adverse Drug Events in Intensive Care Units: A Cross-Sectional Study of Prevalence and Risk Factors. Am J Crit Care 2011;20:e131-40. [Crossref] [PubMed]
- Blatnik J, Lesnicar G. Propagation of methicillin-resistant Staphylococcus aureus due to the overloading of medical nurses in intensive care units. J Hosp Infect 2006;63:162-6. [Crossref] [PubMed]
- Kelly DM, Kutney-Lee A, McHugh MD, et al. Impact of critical care nursing on 30-day mortality of mechanically ventilated older adults. Crit Care Med 2014;42:1089-95. [Crossref] [PubMed]
- Benbenbishty J, Adam S, Endacott R. Physical restraint use in intensive care units across Europe: The PRICE study. Intensive Crit Care Nurs 2010;26:241-5. [Crossref] [PubMed]
- McQuillan P, Pilkington S, Allan A, et al. Confidential inquiry into quality of care before admission to intensive care. BMJ 1998;316:1853-8. [Crossref] [PubMed]
- Wong WT, Ling L, Gomersall CD. Making critical care education BASIC: A collaborative approach to training. ICU Manag Pract 2017;17:216-9.
- Leung C, Joynt G, Wong WT, et al. Usefulness of a mobile application in undergraduate critical care teaching. Intensive Care Med Exp 2015;3:A857. [Crossref]
Cite this article as: Gomersall CD. Asian intensive care research and education. J Emerg Crit Care Med 2018;2:28.


