An unexpected case of diphtheria—the need for vigilance
Introduction
Diphtheria is an infection that has not been encountered in Singapore for the past 25 years. We present a case of a young foreign national from an endemic region in Asia who developed airway obstruction and acute respiratory distress syndrome (ARDS) from diphtheria. It highlights the need to be vigilant for rare infectious diseases, especially in the acute care setting, and the rapidly progressive and often lethal nature of diphtheria. Observing good precautionary measures at the outset and having in place a robust follow-up programme for affected health care workers (HCW) are important.
Case report
First presentation
A 21-year-old Bangladeshi construction worker, previously well, presented to Emergency Department (ED) with worsening neck pain and severe odynophagia associated with fever for the past 2 days. This information was gathered from his colleagues as he was unable to speak and was found to have saliva pooling in his oral cavity. His neck was swollen and extremely tender on palpation. He could open his mouth as there was no trismus, but his soft palate looked edematous, obscuring further view. There was no stridor.
Vital signs showed tachycardia with a heart rate of 140 beats per minute and hypertension with non-invasive blood pressure reading of 170/80 mmHg. His saturation was 90–95% on 5 L/min oxygen face mask. He was alert and able to obey commands with Glasgow Coma Scale of E4V1M6.
Otolaryngology was consulted and urgent endoscopy was performed. As it was difficult to obtain a view through the nares, endoscopy was performed through the oral cavity, which showed generalized pharyngeal wall swelling that was circumferentially oedematous and touching the lateral portions of the epiglottis. The epiglottis also appeared swollen. The aryepiglottic folds and vocal cords were edematous as well with a posterior glottis gap of 2 to 3 mm. The vocal cords remained mobile though.
Lateral neck X-ray was quickly obtained which showed enlargement of the tonsillar soft tissue shadows and thickening of the prevertebral soft tissue. The epiglottis also appeared thickened. No radiopaque foreign body was seen.
Securing the airway
As there was impending airway collapse, the patient was immediately sent to the Operating Theatre (OT) for his airway to be secured. Awake fibreoptic bronchoscopy was attempted by the anaesthetists. Secretions were cleared but as there was poor visualization of the vocal cords, tracheostomy was eventually performed under local anaesthesia by the otolaryngology surgeons.
A Shiley size 6 non-fenestrated cuffed tracheostomy tube was inserted. A false passage was realized almost instantly as high airway resistance was encountered when the anaesthetist manually ventilated the patient using the reservoir bag of the anaesthetic machine. The tracheostomy tube was subsequently removed and the wound examined. The exact site of the tracheostoma was re-identified and the tracheostomy tube was then re-inserted without difficulty.
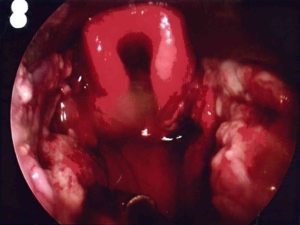
Intraoperative findings showed purulent secretions and swelling obscuring visualization of airway, central trachea with overlying edematous tissue, and purulent secretions and pseudomembranous appearance of mucosa over bilateral tonsils, base of tongue and larynx (Figure 1).
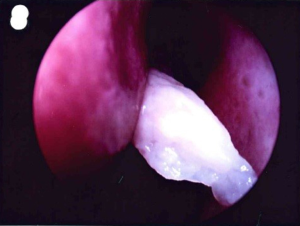
Bilateral tonsils appeared necrotic, uvula was central but there was generalised edema of bilateral anterior tonsillar pillars and soft palate noted. Epiglottis was very edematous, false cords, true cords and subglottis were also edematous and the airway obstructed. Similar pseudomembranous material (Figure 2) was found within glottis and subglottis.
Rigid oesophagoscopy was performed to 25 cm post tracheostomy. No abnormality was detected. There was purulent nasal discharge in bilateral anterior nasal space with sloughy pseudomembranous material extending into post-nasal space. Flexible bronchoscopy was performed via tracheostomy down to the carina, which showed similar pseudomembranous material along tracheal walls though less extensive.
Post operatively, he was transferred for computed tomography of the neck, which showed diffuse inflammatory soft tissue edema causing severe/near complete narrowing of the upper aero digestive tract. Bilateral cervical lymphadenopathy was noted. There was mild to moderate pneumomediastinum.
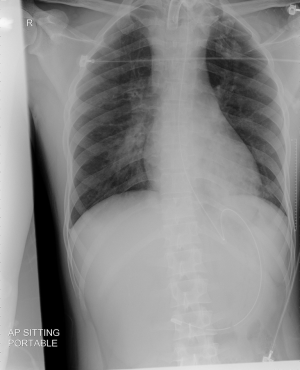
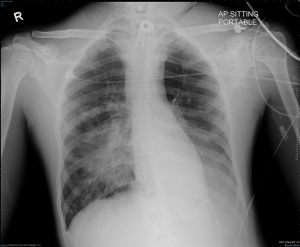
He was admitted to Surgical Intensive Care Unit (ICU) at 1 a.m. after the tracheostomy was performed. Initial chest X-ray in the ICU did not show obvious consolidative changes (Figure 3). After admission to ICU, he was ventilated with volume control mode, fraction of inspired oxygen (FiO2) of 80%, tidal volume (VT) of 470 mL, respiratory rate of 18 breaths per minute and positive end expiratory pressure (PEEP) of 6 cmH2O as he was stabilised. This was continued till 10 a.m. the next day when he was changed to pressure support mode, with FiO2 of 60%, pressure support of 8 cmH2O and PEEP remaining unchanged. Arterial blood gas after the change to pressure support mode showed pH 7.360, PaCO2 39.7 mmHg, PaO2 135.0 mmHg, base excess −3.2, bicarbonate 21.7 mmol/L.
Treatment of diphtheria
He was started on intravenous (IV) piperacillin-tazocin empirically. High clinical suspicion of diphtheria infection was present, given the pan-endoscopy findings. The patient was given a dose of diphtheria anti-toxin and covered with IV erythromycin, and amoxicillin-clavulanate acid after review by Infectious Diseases. When preliminary tonsillar tissue culture confirmed positive for Corynebacterium diphtheriae, notification was made to the Ministry of Health, Singapore.
Deterioration and demise
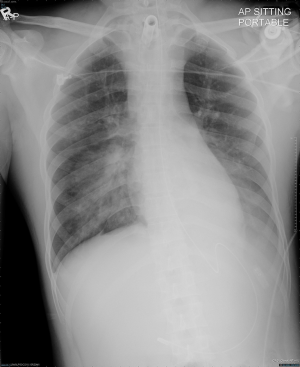
The patient was kept intubated in an Isolation Room. Inotropic support and ventilatory requirements were markedly increased the following day from 3 a.m. onwards as the patient developed ARDS, likely from sepsis caused by the diphtheria infection. His chest X-ray showed bilateral consolidation (Figure 4). In view of his worsening condition, antibiotics were escalated to IV meropenem and vancomycin, in addition to erythromycin. Ventilatory settings were changed from pressure support mode back to volume control mode and FiO2 was increased from 60% to 100% over a course of 8 hours, PEEP was also increased to 20 cmH2O. VT was increased to 550 mL. Despite that, his arterial blood gas showed pH 7.207, PaCO2 56.8 mmHg, PaO2 59.8 mmHg, base excess −6.7, bicarbonate 18.8 mmol/L. Mean airway pressure had increased from 10 to 25 cmH2O, likely indicative of worsening lung compliance. Subsequently, employing lung protective ventilation strategies, the VT was reduced to 450 mL and the respiratory rate increased to 24 breaths per minute. IV plasmalyte and 5% albumin solutions were given in boluses for fluid resuscitation when he became hypotensive. At the same time, IV noradrenaline was also started.
The patient was reviewed by Cardiology and Respiratory Medicine for additional inputs in view of the high risk for myocarditis and the escalating ventilatory requirements. Their impressions were also that of severe ARDS. Transthoracic echocardiogram showed normal chamber sizes, normal ejection fraction, no regional wall motion abnormalities, small left ventricular cavity secondary to tachycardia and under filling. There were no features of myocarditis. Consequently, more IV plasmalyte and 5% albumin solutions were given, to a combined cumulative total of 2.5 litres.
The patient continued to deteriorate and chest X-ray showed worsening of bilateral consolidation (Figure 5). He was commenced on prone ventilation with lung protective strategies to maintain SpO2 88–92%. Oxygenation improved from PaO2 64.1 mmHg to PaO2 76.8 mmHg transiently for 2 hours before decreasing again. Paralysis with atracurium was started at 30 mg per hour and continued. IV vasopressin and IV adrenaline were subsequently started. He was referred for extra-corporeal membrane oxygenation support, which was not available in our hospital. Chest X-ray repeated showed dense consolidation, which was much worse (Figure 6). Six hours later, arterial blood gas showed pH 7.092, PaCO2 64.7 mmHg, PaO2 65.8 mmHg, base excess −11.8 and bicarbonate 15.3 mmol/L. Airway pressure release ventilation was attempted. After 2 hours, the patient became severely hypotensive with blood pressure of 64/53 mmHg despite being on triple inotropic support with noradrenaline 1 µg/kg/min, adrenaline 1 µg/kg/min and vasopressin 2.4 U/hour. Prognosis was extremely poor.
Eventually, he developed pulseless electrical activity from hypoxia and severe metabolic acidosis. He was turned supine and cardiopulmonary resuscitation was performed. Arterial blood gas showed pH 6.805, PaCO2 77.4 mmHg, PaO2 47.6 mmHg, base excess −23.9, bicarbonate 7.5 mmol/L. The tracheostomy tube was disconnected from the ventilator and suction performed, indicating that the tracheostomy tube was patent. Large amounts of blood-stained frothy secretions were suctioned out. The patient did not respond to the resuscitation and demised.
Contact tracing and prevention
After notification to the Ministry of Health, a total of 48 contacts, who had worked or lived with the patient, was identified for further assessment (1). Among the 48 contacts identified, two close contacts had developed sore throat and were being isolated. All 48 contacts had been given prophylactic antibiotics and a booster diphtheria vaccine, and their respiratory samples had been taken for testing.
In addition, all HCW who had contact with this patient were given a booster diphtheria vaccine and antibiotic prophylaxis with either erythromycin or benzathine penicillin.
Discussion
The disease
Diphtheria is an infection caused by the Corynebacterium diphtheriae bacterium, a Gram-positive bacillus. It multiplies on or near the surface of the mucous membranes of the throat. It is spread via respiratory droplets, from an infected person’s cough or sneeze, contaminated personal items or by contact with an infected wound or sore.
Onset of respiratory symptoms usually follows an incubation period of 2 to 5 days, toxin production leads to the production of pseudomembranes, dense, gray debris layer composed of a mixture of dead cells, fibrin, red blood cells, white blood cells and organisms. These can cause airway obstruction which can cause suffocation. Our patient developed this but his airway was secured in time with a surgical tracheostomy.
Other manifestations of diphtheria include myocarditis, conduction defects and cranial and sensorimotor peripheral neuropathy. In our patient, he developed acute respiratory distress syndrome, eventually demised from hypoxia and severe metabolic acidosis. Other manifestations of diphtheria include chronic, indolent, non-healing skin ulcers.
Worldwide, in 2016, according to figures from the World Health Organization, there were 7,097 reported cases of diphtheria, mainly from India and Madagascar (2). There is a higher fatality rate in young children.
Diphtheria is preventable through vaccination. In Singapore, vaccination against diphtheria is compulsory by law for children, as part of the National Childhood Immunization Programme since 1962. The vaccination coverage in children aged two is high, at 96 to 98 per cent. As such, the risk of diphtheria spreading in Singapore is low. The last local case of diphtheria was reported in 1992 and the last imported case was in 1996 (2).
From the literature, we have noted that diphtheria vaccinations do not provide lifelong immunity and regular booster shots are needed. Regular booster vaccines should be given every 10 years for continued protection and are especially recommended for those traveling to endemic areas (3,4).
Diphtheria anti-toxin reduces mortality from patient and early treatment is critical, with the degree of protection from diphtheria anti-toxin inversely related to the duration of clinical illness prior to its administration. This is because the anti-toxin only acts on the unbound toxin and once the toxin acts on the cells, administering the anti-toxin will not have any therapeutic effect. An infected patient usually becomes non-infectious within 48 hours after the antibiotics have been started.
The need for vigilance
In the acute care setting, such as ED, OT for emergency cases and ICU, where patients with infectious diseases can present, it is important to have a high index of suspicion and carry out precautions to protect HCW against infections. We are living in an increasingly globalised world and our patients may be coming from any part of the world.
There should be easily and readily available N95 masks, powered air-purifying respirators for HCW. Mask fitting is compulsory for all new staff to ensure that they have adequately fitted masks when required. In addition, isolation facilities should be available for patients at risk of infectious cases, especially those with airborne spread.
Especially for HCW managing the airway such as intubation, performing a tracheostomy or suctioning respiratory secretions, adequate protection from possible airborne diseases should be observed (5). In our institution, we have made it a point for HCW managing an airway with an unknown infectivity status to don N95 masks for personal protection.
Continued education and training of HCW for infection control must be carried out.
In addition, our hospital has an infection control team, to carry out contact tracing of staff and to ensure adequate post-exposure prophylaxis is given. For this case, there was a total of 66 HCW involved from the ED, OT and ICU. There were a total of 32 nursing staff, 24 medical staff and ten allied health and support staff exposed. All involved HCW were advised post-exposure prophylaxis, which consisted of either oral erythromycin 500 mg every 6 hours for 7 days or one dose of intra-muscular benzathine penicillin 1.2 mU, as well as, a booster diphtheria vaccine, if the last dose of vaccine was given more than 5 years ago. Oral erythromycin dose was later revised to 500 mg twice a day or 250 mg every 6 hours, which was still adequate for prophylaxis, as many HCW developed gastrointestinal side effects. The situation was also further monitored for 2 weeks to ensure that all contact tracing and infection control measures were in place and carried out. Adequate information was given to affected HCW and a calm atmosphere was maintained.
For diphtheria, it took 25 years for the infection to cause a fatality. We cannot anticipate the resurgence of the next rare infection but we can be vigilant and do our best to protect ourselves.
Acknowledgements
The authors would like to thank Dr. Purnima Parthasarathy from Infectious Diseases, Dr. Lim John Wah from Occupational Medicine for their contributions to the article, as well as, Dr. Lilleen Huang Minyi and team from Otolaryngology for the photographs.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: This article is published without consent from the patient. This is because we feel that this report is raising awareness of a rare disease in Singapore and is important to public health and health of our healthcare workers. As the patient is a foreigner, consent from his next-of-kin is very difficult to obtain. Also, a reasonable individual would be unlikely to object to publication of this article which is an anonymous descriptive account of an important infectious disease.
References
- Ministry of Health. Singapore Confirmed case of Diphtheria in Singapore (5 Aug 2017) Available online: https://www.moh.gov.sg/content/moh_web/home/pressRoom/pressRoomItemRelease/2017/confirmed-case-of-diphtheria-in-singapore.html
- World Health Organization. Diphtheria (8 Aug 2017) Available online: http://www.who.int/immunization/monitoring_surveillance/burden/diphtheria/en/
- Grasse M, Meryk A, Schirmer M, et al. Booster vaccination against tetanus and diphtheria: insufficient protection against diphtheria in young and elderly adults. Immun Ageing 2016;13:26. [Crossref] [PubMed]
- Weinberger B. Adult vaccination against tetanus and diphtheria: the European perspective. Clin Exp Immunol 2017;187:93-9. [Crossref] [PubMed]
- Liang SY, Theodoro DL, Schuur JD, et al. Infection prevention in the emergency department. Ann Emerg Med 2014;64:299-313. [Crossref] [PubMed]
Cite this article as: Yeo LS, Quindipan ML, Liew CW, Murukuti P, Chia NC. An unexpected case of diphtheria—the need for vigilance. J Emerg Crit Care Med 2018;2:15.