
Management of fever in critically ill patients with infection
Introduction
Body temperature is one of important vital signs to evaluate the whole-body condition (1). Body temperature is also used for the diagnosis of a ventilator-associated condition associated with infection (2) and for the calculation of APACHE II score (3). Indeed, it is common that new examinations or treatments was triggered by hypothermia or fever in critically ill patients (4). In this review, we described the accuracy of body temperature measurement, the pathophysiology of fever, physiological effect of fever, and current evidence regarding the effects of antipyretics in critically ill patients, especially those with infection. We then, provide an opinion-based recommendation for use of antipyretics in patients with infection.
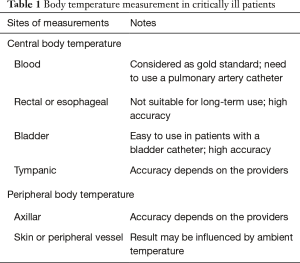
Measurement of body temperature in critically ill patients
The accuracy of body temperature measurement varies depending on the measurement site and the method used for measurement (Table 1). Therefore, physicians should use a measurement site and methods with high reliability as much as possible. Temperatures of major organs such as the brain, lung, heart, liver, and kidney are important for biological activity, and central body temperature measurement is therefore recommended (4). At present, the gold standard for central body temperature is measurement of blood temperature. However, the measurement requires insertion of a pulmonary artery catheter. Blood temperature therefore cannot be measured in a daily care setting. In the guidelines of the American College of Critical Care Medicine (ACCM) and the Infectious Diseases Society of America (IDSA), measurements of blood temperature, bladder temperature, esophageal temperature and rectal temperature are recommended because they would more accurately reflect deep temperature (4).
Full table
Fever in critically ill patients
Fever is thought to be induced through the production of prostaglandin E2 and cyclooxygenase 2, stimulated by endogenous interleukin (IL)-1 and tumor necrosis factor (TNF)-α that are produced in response to extrinsic stimuli (5). Thus, fever is an important indicator that suggests the presence of infection. In a multicenter observational study (FACE study), about 63% of the patients who had a body temperature of 38.5 °C or higher were diagnosed as having sepsis (6). However, fever is also a physiological response to non-infective pathology (7-11), including surgery, blood transfusion, drug administration, acute rejection, acute myocardial infarction, cerebral infarction, cerebral hemorrhage, acute pancreatitis, malignant tumor and other conditions (Table 2). Additionally, it should be noted that fever in seriously ill patients sometimes has multiple causes.

Full table
Physiological effect of fever
Fever may have detrimental effects such as causing discomfort, increasing minute ventilation and oxygen consumption, and worsening the neurological outcomes (12-14). In post-hoc analysis to assess the independent association of fever with ventilator-free days in critically ill patients who required mechanical ventilation, a significant association was found between fever and mechanical ventilator-free days in all of the enrolled subjects (15).
Laupland et al. conducted a large epidemiological study in critically ill patients and showed that increased intensive care unit (ICU) mortality was not associated with the presence of fever (≥38.3 °C) but, was associated with high fever (≥39.5 °C) (P<0.001) (16). However, the FACE study showed that body temperature ≥39.5 °C was associated with increased risk of 28-day mortality in non-septic patients (P=0.01) but not in septic patients (adjusted odds ratio: 0.47, P=0.11) compared with body temperature of 36.5–37.4 °C (6). Some studies have shown such an inverse association between fever and mortality in patients with infection (17,18).
Types of antipyretics
Antipyretic treatments are usually performed in critically ill patients. The FACE study showed that antipyretic therapy was performed in more than half of septic patients with a body temperature of >39.5 °C and in approximately one-third of septic patients with a body temperature of 38.5–39.4 °C (6). It is unfortunate that the benefits and harmful effects of antipyretics in critically ill patients, especially those in a septic condition, have not been clarified. Indeed, current guidelines do not provide any recommendations for the use of antipyretics in septic patients who have developed fever (4,19).
There are two methods for treating patients with fever: administration of an antipyretic drug and physical cooling. Non-steroidal anti-inflammatory drug (NSAIDs) or acetaminophen are used as antipyretics drugs. Such antipyretic drugs may lower body temperature by decreasing the threshold of body temperature control in hypothalamus through the inhibitation of prostaglandin E production. Therefore, a decrease in body temperature can be expected by administration of antipyretics drugs both in patients taking sedatives and those not taking sedatives.
Physical cooling is used to cool the body surface in order to lower body temperature. Sedation should suppress cold reactions (shivering and vasoconstriction), and sedation combined with physical cooling would therefore be effective for body temperature reduction (20,21). However, if the patient is not under sedation, the patient’s set point of regulation in body temperature does not change, and physical cooling may therefore cause a cold reaction. In that case, it would be difficult to lowering body temperature, and oxygen consumption and minute ventilation may increase.
Gozzoli and colleagues reported that physical cooling in critically ill patients without sedatives may result in a decrease in body temperature of only 0.5 degree and a 10% increase of oxygen consumption (22). Lenhardt and colleagues also reported that physical cooling in non-sedative volunteers after administration of IL-2 did not decrease body temperature but significantly increased the incidence of shivering and oxygen consumption compared with the use of a blanket (23). These studies suggest that physical cooling may promote shivering and increase oxygen consumption in patients without sedatives. If the purpose of antipyretic therapy is to make patients comfortable and to decrease oxygen consumption, it might be better to avoid physical cooling in patients who are not taking sedatives.
Conflicting evidence regarding antipyretics in critically ill patients
Since fever may result in reduced bacterial growth, promotion of the synthesis of cytokines, antibodies, and activation of neutrophils, macrophages and T cells (24-26), fever could be considered to be a protective host response against infection. In this regard, lowering body temperature by using antipyretics may be undesirable for patients with sepsis because of suppression the febrile response, which has been suggested by various animal and human studies to inhibit the activity of viruses and bacteria (24-26). Schulman et al. conducted a randomized controlled trial (RCT) in trauma patients to compare aggressive antipyretic therapy (>38.5 °C: administration of acetaminophen, >39.5 °C: physical cooling) and permissive approach (>40 °C: administration of acetaminophen with physical cooling). Mean body temperature in the aggressive group was significantly lower than that in the permissive group (36.7 vs. 37.8 °C, P=0.006). At the time of their first interim analysis, six patients in the aggressive antipyretic group had died (6/44=13.6%), whereas there was only one death in the permissive group (1/38=2.6%) (odds ratio: 7.14, P=0.06). Their study was then stopped due to safety concerns. There was no significant difference in the incidence of infection between the aggressive group (4±6/person) and the permissive group (3±2/person) (P=0.26); however, the amount of antimicrobial use was significantly decreased in the permissive group (P=0.007) (27). There have also been studies showing the possibility of harm of antipyretics (28) and suggesting not to use it in the patients with infection (29,30). Antipyretic drugs also have side effects such as gastrointestinal disorders, hepatic disorders, and kidney disorders (31). Furthermore, administration of antipyretics is not a cheap procedure. There has been a report that 10,000–30,000 dollors was spent in an 18 beds ICU for 1 year on antipyretic therapy (32).
In contrast to above-described studies, there have been several studies supporting the use of antipyretics in critically ill patients with infection. Schortgen et al. conducted a multicenter randomized trial in 200 patients with sepsis requiring vasopressor administration, mechanical ventilation and sedation to compare physical cooling for the first 48 hours after ICU admission and no physical cooling. The physical cooling in this cohort significantly decreased body temperature (36.8±0.7 vs. 38.4±1.1 °C; P<0.01), increased recovery from shock (P=0.02) and reduced 14-days mortality (19% vs. 34%, P=0.01) (33). There was no significant difference between ICU mortality (35% vs. 43%) or hospital mortality rate (43% vs. 48%) between the two groups. Since all of the patients in that study were sedated patients, the results of that study cannot be generalized to patients who are not sedated.
The HEAT study was a multicenter randomized trial in 700 intensive care patients suspected to be infected that was carried out to compare the effects of acetaminophen administration with a placebo in patients with a body temperature >38 °C (34). Acetaminophen or the placebo was administered for a median of eight or nine times per patient. The mean body temperature decreased by 0.28 °C in the acetaminophen group (37.0 vs. 37.3 °C, P<0.001). The number of ICU-free survival days at day 28 was increase in the acetaminophen group (median: 23 vs. 22 days, P=0.07), but the difference was not significant.
Recent meta-analysis to assess the impact of antipyretic therapy on mortality in critically ill septic adults
Drewry et al. recently reported the results of their updated meta-analysis to examine the impact of antipyretic therapy on mortality in critically ill septic adults (35). They searched the literature through February 2016 and included eight randomized studies on septic patients (1,507 patients). Most of the studies in that meta-analysis were not designed primarily to evaluate the clinical effect of fever treatment and some of the RCTs had a middle to high risk of bias. They reported that antipyretic therapy did not reduce 28-day/hospital mortality and did not change shock reversal or acquisition of nosocomial infections. These results are consisted with the results of another meta-analysis (36). It should be noted that the studies also varied in terms of the type of antipyretic interventions and the target body temperatures. In this regard, it is required caution to interpret the results of these meta-analysis since there have been studies suggesting that the effects of antipyretic drug and physical cooling might be differed (6,37) and that the effect of antipyretic drugs is different at different body temperatures (38).
How should we use antipyretics in septic patients?
As mentioned above, there is no definitive conclusion for antipyretic therapy in febrile critically ill patients. Until results of large-scale randomized trials examining the effect of antipyretic therapy in critically ill patients are reported, it seems that antipyretic therapy should be performed according to each patient’s condition. If patient has fever, possible causes including infection etiology and non-infection etiology should be examined, specimens should be collected from the suspected foci and a blood culture should be performed, and treatment with antibiotics should be started if necessary. If the fever itself is within the normal physiological response accompanied by compensating change of vital signs including heart rate and respiratory rate, it might be better not to treat the fever. However, if there is decompensation of vital signs including tachycardia, tachypnea or patient suffering caused by fever, antipyretics should be used to prevent derangement. In doing so, it is necessary to understand the effects of antipyretic drugs and physical cooling on physiology and to use an appropriate method. Since fever and antipyretic therapy may have merits and demerits, routine antipyretics triggered by certain body temperature might be better to be avoided.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992;101:1644-55. [Crossref] [PubMed]
- Magill SS, Klompas M, Balk R, et al. Developing a new, national approach to surveillance for ventilator-associated events. Crit Care Med 2013;41:2467-75. [Crossref] [PubMed]
- Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818-29. [Crossref] [PubMed]
- O’Grady NP, Barie PS, Bartlett JG, et al. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit Care Med 2008;36:1330-49. [Crossref] [PubMed]
- Boulant JA. Role of the preoptic-anterior hypothalamus in thermoregulation and fever. Clin Infect Dis 2000;31 Suppl 5:S157-61. [Crossref] [PubMed]
- Lee BH, Inui D, Suh GY, et al. Association of body temperature and antipyretic treatments with mortality of critically ill patients with and without sepsis: multi-centered prospective observational study. Crit Care 2012;16:R33. [Crossref] [PubMed]
- Badillo AT, Sarani B, Evans SR. Optimizing the use of blood cultures in the febrile postoperative patient. J Am Coll Surg 2002;194:477-87. [Crossref] [PubMed]
- Kennedy LD, Case LD, Hurd DD, et al. A prospective, randomized, double-blind controlled trial of acetaminophen and diphenhydramine pretransfusion medication versus placebo for the prevention of transfusion reactions. Transfusion 2008;48:2285-91. [Crossref] [PubMed]
- Roush MK, Nelson KM. Understanding drug-induced febrile reactions. Am Pharm 1993;NS33:39-42. [Crossref] [PubMed]
- Hawksworth JS, Leeser D, Jindal RM, et al. New directions for induction immunosuppression strategy in solid organ transplantation. Am J Surg 2009;197:515-24. [Crossref] [PubMed]
- Egi M, Morita K. Fever in non-neurological critically ill patients: A systematic review of observational studies. J Crit Care 2012;27:428-33. [Crossref] [PubMed]
- Manthous CA, Hall JB, Olson D, et al. Effect of cooling on oxygen consumption in febrile critically ill patients. Am J Respir Crit Care Med 1995;151:10-4. [Crossref] [PubMed]
- Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002;346:549-56. [Crossref] [PubMed]
- Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002;346:557-63. [Crossref] [PubMed]
- Park DW, Egi M, Nishimura M, et al. The Association of Fever with Total Mechanical Ventilation Time in Critically Ill Patients. J Korean Med Sci 2016;31:2033-41. [Crossref] [PubMed]
- Laupland KB, Shahpori R, Kirkpatrick AW, et al. Occurrence and outcome of fever in critically ill adults. Crit Care Med 2008;36:1531-5. [Crossref] [PubMed]
- Young PJ, Saxena M, Beasley R, et al. Early peak temperature and mortality in critically ill patients with or without infection. Intensive Care Med 2012. [Epub ahead of print]. [Crossref] [PubMed]
- Sundén-Cullberg J, Rylance R, Svefors J, et al. Fever in the Emergency Department Predicts Survival of Patients With Severe Sepsis and Septic Shock Admitted to the ICU. Crit Care Med 2017;45:591-9. [Crossref] [PubMed]
- Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008;36:296-327. [Crossref] [PubMed]
- Axelrod P. External cooling in the management of fever. Clin Infect Dis 2000;31 Suppl 5:S224-9. [Crossref] [PubMed]
- Sessler DI. Perioperative heat balance. Anesthesiology 2000;92:578-96. [Crossref] [PubMed]
- Gozzoli V, Treggiari MM, Kleger GR, et al. Randomized trial of the effect of antipyresis by metamizol, propacetamol or external cooling on metabolism, hemodynamics and inflammatory response. Intensive Care Med 2004;30:401-7. [Crossref] [PubMed]
- Lenhardt R, Negishi C, Sessler DI, et al. The effects of physical treatment on induced fever in humans. Am J Med 1999;106:550-5. [Crossref] [PubMed]
- Ryan AJ, Flanagan SW, Moseley PL, et al. Acute heat stress protects rats against endotoxin shock. J Appl Physiol 1992;73:1517-22. [Crossref] [PubMed]
- Villar J, Ribeiro SP, Mullen JB, et al. Induction of the heat shock response reduces mortality rate and organ damage in a sepsis-induced acute lung injury model. Crit Care Med 1994;22:914-21. [Crossref] [PubMed]
- Kluger MJ, Kozak W, Conn CA, et al. The adaptive value of fever. Infectious disease clinics of North America 1996;10:1-20. [Crossref] [PubMed]
- Schulman CI, Namias N, Doherty J, et al. The effect of antipyretic therapy upon outcomes in critically ill patients: a randomized, prospective study. Surg Infect (Larchmt) 2005;6:369-75. [Crossref] [PubMed]
- Makino S, Egi M. Acetaminophen for febrile patients with suspected infection: potential benefit and further directions. J Thorac Dis 2016;8:E111-4. [PubMed]
- Eyers S, Weatherall M, Shirtcliffe P, et al. The effect on mortality of antipyretics in the treatment of influenza infection: systematic review and meta-analysis. J R Soc Med 2010;103:403-11. [Crossref] [PubMed]
- Brandts CH, Ndjave M, Graninger W, et al. Effect of paracetamol on parasite clearance time in Plasmodium falciparum malaria. Lancet 1997;350:704-9. [Crossref] [PubMed]
- Plaisance KI, Mackowiak PA. Antipyretic therapy: physiologic rationale, diagnostic implications, and clinical consequences. Arch Intern Med 2000;160:449-56. [Crossref] [PubMed]
- Gozzoli V, Schottker P, Suter PM, et al. Is it worth treating fever in intensive care unit patients? Preliminary results from a randomized trial of the effect of external cooling. Arch Intern Med 2001;161:121-3. [Crossref] [PubMed]
- Schortgen F, Clabault K, Katsahian S, et al. Fever control using external cooling in septic shock: a randomized controlled trial. Am J Respir Crit Care Med 2012;185:1088-95. [Crossref] [PubMed]
- Young P, Saxena M, Beasley R, et al. Acetaminophen for Fever in Critically Ill Patients with Suspected Infection. N Engl J Med 2016;374:1292-3. [PubMed]
- Drewry AM, Ablordeppey EA, Murray ET, et al. Antipyretic Therapy in Critically Ill Septic Patients: A Systematic Review and Meta-Analysis. Crit Care Med 2017;45:806-13. [Crossref] [PubMed]
- Zhang Z. Antipyretic therapy in critically ill patients with established sepsis: a trial sequential analysis. PLoS One 2015;10:e0117279. [Crossref] [PubMed]
- Suzuki S, Eastwood GM, Bailey M, et al. Paracetamol therapy and outcome of critically ill patients: a multicenter retrospective observational study. Crit Care 2015;19:162. [Crossref] [PubMed]
- Zhang Z, Chen L, Ni H. Antipyretic therapy in critically ill patients with sepsis: an interaction with body temperature. PLoS One 2015;10:e0121919. [Crossref] [PubMed]
Cite this article as: Egi M, Makino S, Mizobuchi S. Management of fever in critically ill patients with infection. J Emerg Crit Care Med 2018;2:10.


