
How to prevent and treat gastrointestinal bleeding in the critically ill patient: a pathophysiological approach
Introduction
Critical care physicians are involved in the treatment of patients with gastrointestinal bleeding in several ways. First, patients outside the ICU suffering from gastro-intestinal tract bleeding with hypovolemic shock may need ICU treatment. Second, patients can develop gastrointestinal bleeding as a complication during their treatment in the intensive care. In all cases, patients who are in a state of hypovolemic shock need appropriate shock treatment with fluids, blood- and plasma transfusions and if needed, vasopressors. In addition, specific causes such as oesophageal varices, gastric- or duodenal ulceration may need local treatment. This local treatment with e.g., endoscopic interventions, Sengstaken-Blakemore tube or coiling may be needed for some patients and at appropriate timing. Several scoring systems rate the severity of illness and their prognostication of patients who present with bleeding outside the ICU (1). A recent study showed that the AIMS65 and Glasgow-Blatchford scores performed better than the pre-endoscopic Rockall score and pre-endoscopic Baylor score (1). The in-hospital mortality appeared to be around 10% (1).
The approach to patients who develop gastrointestinal bleeding during ICU treatment is different from the approach to patients who develop bleeding outside the ICU and is in a way more complex. This narrative review provides an overview of pathophysiology, prevention and treatment for patients who develop gastrointestinal bleeding during their ICU stay.
Aetiology
The normal gastric mucosa is designed and highly matched to resist the acidic fluids in the gastric lumen. The integrity of the gastric mucosa is normally formed by the mucus layer, a phospholipid barrier, the tight junctions between epithelial cells, the regeneration capacity of the mucosa, prostaglandin production and the mucosa blood flow (2). Loss of one or more of these barriers leads to a diminished integrity of the gastric mucosa. In critically ill patients, the inflammatory state and altered circulation of the splanchnic region can easily result in a reduction in one or more of these defence mechanisms. When disturbances in the integrity of the gastric mucosa occur, gastric acid is permitted to reach the deeper layers of the mucosa, which can lead to the formation of a gastric ulcer. Mucosal damage occurs in 75–100% of patients admitted to the ICU in shock (3,4). Also, the extreme physical stress with sympathetic drive and vasoconstriction in burn or neurosurgical patients lead to a high incidence of gastric ulcer in this group of patients (5). Probably the main reason for a disruption of the mucosal barrier function in any critically ill patient is a reduced mucosal circulation (2,6). A normally perfused mucosa recovers from injury within hours but an impaired splanchnic perfusion during an inflammatory state hampers recovery. Disturbed microcirculation and vasoconstriction in the splanchnic region occurs due to endotoxemia and hypovolemia in the acute phase of severe disease. This process enforces itself due to the increased translocation of endotoxins through the ischemic mucosa and subsequent endotoxic vasoconstriction (7). The reduced perfusion with ischemic mucosa leads to a loss of tight junctions. The concept of reduced integrity and increased permeability in critically ill patients was proven in at least two studies by measuring an increased absorption of sucrose (8,9). The damaged mucosa leads to acid back diffusion and consecutive ulcer formation occurs. In 1970 Skillman published the results of his studies to the gastric mucosal barrier function and back-diffusion of acid (10). He concluded: “These studies strongly suggest that disruption of the barrier function of the stomach, especially in the presence of poor vascular perfusion may be an important clue to the pathogenesis of the vexing and highly fatal problem of acute stress ulceration of the human stomach.” However, many clinicians today still hold gastric acid responsible for stress ulceration in the stomach and choose their treatment according to that view instead of focussing on the improvement of splanchnic perfusion.
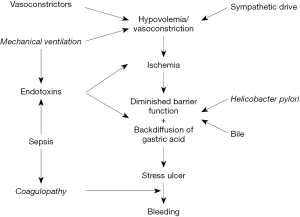
Above reasoning leads to a conceptual framework (Figure 1) that increases our insight in the pathophysiology of stress ulcer formation and prevention (11). Additional factors that add to the diminished gastric mucosa integrity are the presence of H. pylori and reflux of bile from the duodenum towards the stomach (4,12). Mechanical ventilation and coagulopathy were identified as independent risk factors and fit in the conceptual framework as shown (Figure 1) (13).
Definition
The most frequent location of gastrointestinal bleeding is the stomach although all sites within the gastrointestinal tract may bleed. Bleeding may be occult or overt. Occult bleeding may happen unknown as many critically ill patients experience a decrease in haemoglobin level and many receive a transfusion at some point in their ICU stay. Occult bleeding can stop or develop into overt bleeding. Overt bleeding is usually defined according to Cook and co-workers as hematemesis, gross blood or “coffee grounds” material in a nasogastric aspirate, hematochezia, or melena (13). Not every overt bleeding is severe enough to lead to clinical consequences such as shock. Cook used a detailed and complex definition of clinical important bleeding as overt bleeding complicated by a decrease in systolic blood pressure (20 mmHg), increase in heart rate (20 bpm), or a decrease in haemoglobin level within 24 hours after the onset of bleeding, in the absence of other causes (13). This definition is difficult to use at the bedside. In short, this definition describes that a clinically important bleeding is associated with hypotension and/or transfusion.
The location of the bleeding can be upper or lower gastrointestinal tract. The upper gastrointestinal tract is oesophagus, stomach and small bowel. Occasionally the bleeding originates from other locations such as the biliary tract (14). Often the location is initially unknown and bleeding from the upper gastrointestinal tract is then referred to as upper gastrointestinal bleeding (UGIB). It is important to realize that the source of the bleeding can be a reflux esophagitis, which has a completely different cause and treatment than stress ulcerations. In one study two or three out of 16 bleeds (12–18%) appeared to be caused by esophagitis (15). Bleeding that results from stress ulcerations is called stress ulcer related bleeding (SURB). This implies that an UGIB can only be called SURB after endoscopic investigation or, in retrospect, during autopsy. As a consequence, UGIB incidence is higher than the true SURB incidence (1.9% vs. 1.0% in one study) (15). This distinction is important when the literature on this subject is reviewed concerning incidence, prevention and treatment. The incidence of UGIB is variable in the literature as was shown in recent studies. Incidences of 1.96% (16) and as high as 6.1% were reported recently (17). However, a low incidence of 0.6% has been published before (18).
Presentation
The clinical signs of gastrointestinal bleeding vary. Most patients with nasogastric tubes present with blood or coffee grounding in the gastric residual aspirations. Usually this is combined with signs of hypotension or a drop in haemoglobin and as such this may fit within the definition of clinically important bleeding (13). In case of esophagitis, in a minority of patients retrosternal pain is expressed. Usually both esophagitis and stress ulceration are without signs of pain or discomfort, although in burn patients epigastric pain is associated with ulcer formation (5). Stress ulcerations are most often detected in the stomach but may be present throughout the complete gastrointestinal tract, from stomach to rectum. Bleeding in the upper gastrointestinal tract will usually lead to black, sticky and smelling faeces, melena. Bleeding from the lower gastrointestinal tract will appear as bloody stools, hematochezia. In that case, endoscopic studies are useful too as haemorrhoids will ask for a different approach than stress ulceration. Ulceration in the colon may be related to ischemia as ischemic colitis. The differentiation between ischemic colitis and stress ulceration in the colon is more or less semantic as both can be seen as a result of inadequate perfusion. A diffuse ischemia present in small or large bowel without obstruction in the arteries is called non-occlusive mesenteric ischemia (NOMI). In contrast, when occlusion is present, occlusive mesenteric ischemia is the case. It is important to differentiate between these two situations, as occlusive ischemia needs opening of the vessels were NOMI needs improvement of the (micro)circulation. The clinical presentation of NOMI is usually not bleeding but abdominal pain, distension of the bowel and inflammatory response (19). However, the clinical and laboratory signs are quite variable (19,20). It has become clear that no single or combined biochemical marker is precise and accurate enough to exclude or diagnose NOMI (20).
Prevention
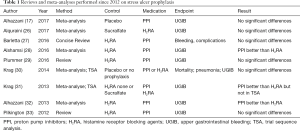
Clinically important bleeding adds to ICU mortality with a relative risk of 4 in a regression model, 1.0 in an adjusted regression model and 1.8 or 2.9 in matched cohort models (21). Another recent observational trial in patients with clinically important gastrointestinal bleeding, the adjusted odds ratio for 90-day mortality was not significantly higher (OR 1.7; 95% CI: 0.7–4.3) (22). One of these studies showed a significant longer length of stay of 4–8 days for patients with bleeding (21). Taken together, it is worthwhile to prevent stress ulceration and subsequent bleeding. Probably, over the years an improved treatment of the circulation, respiratory failure, optimization of feeding and early sepsis recognition and treatment has had its effect, leading to a lower incidence than in the 1970’s. In those early years, many intensive care patients needed a laparotomy for gastric ulceration with bleeding and sometimes perforation. Most critically ill patients have stress ulcerations, although not many suffer from bleeding (3,4). In a setting with a combined strategy that focuses on most of the etiological factors, as reviewed in Figure 1, the incidence of UGIB appeared to be as low as 0.6% (18). In that study a combination of several approaches was used: early goal directed therapy, vasodilators to reduce vasoconstriction, selective decontamination of the digestive tract to reduce endotoxemia, H. pylori carriership and secondary sepsis, steroids to reduce inflammation, early use of prokinetics to reduce bile to regurgitate and protective mechanically ventilation strategies (18). Histamine receptor blocking agents (H2RA) and proton pump inhibitors (PPI) were not used at all. In contrast, acid reducing strategies are frequently used as a preventive strategy although acid is not the main cause of stress ulceration and bleeding (23). Moreover, acid suppression was for long a standard treatment for most intensive care patients according to guidelines that recommend its use routinely but the most recent guidelines restrict the use to patients at risk for SURB (24). In a survey of 97 ICUs, it was shown that all but one ICU routinely provided acid suppressive agents (23). The exact practice, however, varied considerably and PPI was most the frequently used agent (23). In another study it was shown that the adherence to the guideline concerning stress ulcer prophylaxis is low with both over- and underutilization (25). The available clinical research on the prevention of stress ulceration and associated bleeding also focuses on acid reducing interventions and is summarized in Table 1.
Full table
H2RA or PPI versus placebo
Two meta-analyses reviewed the studies that compared acid suppressive agents, H2RA and PPI, with placebo. Both did not show any improvement in the incidence of UGIB and neither in mortality (Table 1). Alhazzani and co-workers found in around 600 patients that the odds ratio for clinically important UGIB was 0.96 (95% CI: 0.24–3.82) (17). Krag and co-workers found in 15 studies with the endpoint mortality a RR 1.00, 95% CI 0.84–1.20. Neither PPI nor H2RA was associated with a mortality benefit when studied separately (30). For the outcome UGIB, in the included two studies using PPIs the RR was 1.04 with 95% CI 0.07–16.3. H2RA were associated with lesser UGIB in 20 studies with a RR 0.44, 95% CI 0.28–0.68. However, heterogeneity was large with 48%. The authors debated this finding themselves as a trial sequence analysis (TSA) showed that only 22% of the calculated number of needed patients were included in all studies together. As such, the evidence is in their conclusion not convincing yet (30). The same results were found in another earlier review by the same authors (31).
In addition, a new RCT that is not yet included in the meta-analyses yet, PPI compared to placebo suggest that primary prevention with PPIs is not per se needed for all intensive care patients (34). Moreover, the use of PPIs may even bear some risks in itself by increasing infection, hypomagnesaemia and mortality (35).
H2RA versus PPI
In five reviews and meta-analyses comparisons between H2RA and PPI have been reported (Table 1).
Compared to H2RA, PPIs lower the risk for bleeding in three of the reviews/meta-analysis. This was shown in the reviews from Alhazzani and Alshamsi and Krag (28,31,32). Although Krag found a RR of 0.44 (95% CI: 0.22–0.88 for PPI vs. H2RA), the trial sequence analysis was not significant (31). The reviews from Barletta, that from Plummer and an older review from Pilkington could not confirm the superior effect of PPI compared to H2RA (27,29,33). When this knowledge is regarded in relation to the absence of effect of H2RA or PPI compared to placebo, it is unlikely that PPI can have a significant effect compared to H2RA.
Other studies
The use of sucralfate as a gastric mucosa-protecting agent was not more effective in preventing UGIB than H2RA but was associated with fewer ventilators associated pneumonia (VAP) (26).
For subgroups, neurocritical care patients were studied in a review of eight RCTs and over 800 patients. A significant effect was found for stress ulcer prophylaxis (H2RA or PPI combined) on both UGIB and mortality (36). As neurosurgical patients are subject to extreme sympathetic drive, which is probably associated with vasoconstriction and ulcer formation, acid reduction may have an effect in these patients.
The prophylactic use of acid suppressive agents has some potential drawbacks. It may be related to Clostridium colonization and consecutive infection (35). PPIs and H2RA interact with the local immune system and the neurological system, the enteric minibrain, in the gut (37,38). Also, PPIs are often continued after ICU discharge, even at hospital discharge and without clear indication (39). The prescription of acid suppressive medication in the ICU is inherently related to costs. In that respect, H2RA may be more cost efficient than PPI (40). Acid reducing medications have been studied for their effect on ventilator associated pneumonia incidence. A systematic review did not show any effect of PPI or H2RA on the incidence of VAP (30). A RCT compared sucralfate with PPI (pantoprazole) and found a significant lower incidence of VAP (41). The drawback of this study is that this study is relatively small and the incidence in the PPI group is remarkably high (36%).
Treatment
The cornerstone in the treatment of UGIB outside the ICU setting is acid suppression (42). Acid suppression provides an environment for the gastric mucosa to recover. Whether acid suppression in intensive care patients with UGIB leads to faster recovery has not been studied as such. Acid suppression therapy in critically ill patients can be questioned, as it is not evident that critically ill patients produce acid at all in a state of shock. Moreover, Skillman showed in 1970 that a 72% reduction of acid secretion occurred in hemorrhagic shock (10). When acid production is limited, then acid suppression will not have any effect on stress ulcer prevention or treatment. Based on the pathophysiological concept as explained previously, it is more logical to restore mucosal perfusion (11). Shock reversal using fluids, inotropes and vasopressors may all be useful in this respect. However, trials on vasodilator therapy for the splanchnic region have not been performed yet.
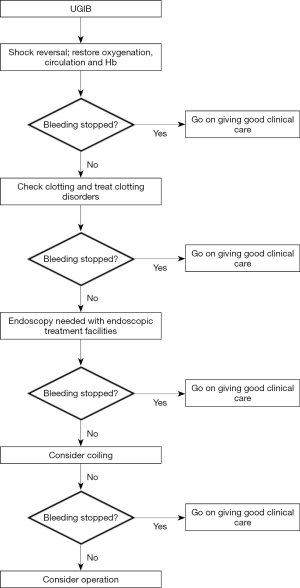
The cornerstone of the treatment of UGIB in intensive care patients is good clinical care: restore circulation, oxygenation and haemoglobin level. In addition, clotting disorders should be treated to enhance clot formation and haemostasis. Usually, these measures are sufficient to stop bleeding. When bleeding proceeds, the next step is to obtain an endoscopic examination with or without endoscopic treatment. Several options are available for local treatment, a discussion of which is outside the scope of this review. When bleeding persists, a coiling of the appropriate vessel is the next step to perform (22). With this sequential and step-up approach a surgical treatment is seldom needed (Figure 2).
Conclusions
Stress ulceration and consecutive bleeding has a complex aetiology and ditto approach. We present a pathophysiological approach and propose a multifactorial preventive strategy that can reduce the incidence to less than 1%. Preventive treatment with acid reducing medications has not convincingly been proven effective and has potential side effects such as Clostridium infection. However, it may be effective in selected patients at high risk for UGIB such as neurosurgical and burn patients. Critically ill patients with clinically important bleeding need appropriate shock treatment and additional local treatment in a stepwise approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Tang Y, Shen J, Zhang F, et al. Comparison of four scoring systems used to predict mortality in patients with acute upper gastrointestinal bleeding in the emergency room. Am J Emerg Med 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Yandrapu H, Sarosiek J. Protective Factors of the Gastric and Duodenal Mucosa:An Overview. Curr Gastroenterol Rep 2015;17:24. [Crossref] [PubMed]
- Bardou M, Quenot JP, Barkun A. Stress-related mucosal disease in the critically ill patient. Nat Rev Gastroenterol Hepatol 2015;12:98-107. [Crossref] [PubMed]
- van der Voort PH, van der Hulst RW, Zandstra DF, et al. Prevalence of Helicobacter pylori infection in stress induced gastric mucosal injury. Intensive Care Med 2001;27:68-73. [Crossref] [PubMed]
- Choi YH, Lee JH, Shin JJ, et al. A revised risk analysis of stress ulcers in burn patients receiving ulcer prophylaxis. Clin Exp Emerg Med 2015;2:250-5. [Crossref] [PubMed]
- Tarnawski AS, Ahluwalia A, Jones MK. The mechanisms of gastric mucosal injury:focus on microvascular endothelium as a key target. Curr Med Chem 2012;19:4-15. [Crossref] [PubMed]
- Deitch EA. Gut-origin sepsis: evolution of a concept. Surgeon 2012;10:350-6. [Crossref] [PubMed]
- Burgstad CM, Besanko LK, Deane AM, et al. Sucrose malabsorption and impaired mucosal integrity in enterally fed critically ill patients: a prospective cohort observational study. Crit Care Med 2013;41:1221-8. [Crossref] [PubMed]
- van der Voort PH. H. pylori in the critically ill. Chapter 9, Thesis, University of Amsterdam 1999. Available online: , accessed on October 8th 2017.https://pure.uva.nl/ws/files/3360533/5766_UBA003000168_012.pdf
- Skillman JJ, Gould SA, Chung RS, et al. Clinical and experimental studies in critically ill and normal ma, and in the rabbit. Ann Surg 1970;172:564-84. [Crossref] [PubMed]
- van der Voort PH, Zandstra DF, Tytgat GN. Helicobacter pylori in intensive care. Intensive Care Med 2004;30:1245-6. [Crossref] [PubMed]
- Ritchie WP. Role of bile acid reflux in acute hemorrhagic gastritis. World J Surg 1981;5:189-98. [Crossref] [PubMed]
- Cook DJ, Fuller HD, Guyatt GH, et al. Risk factors for gastrointestinal bleeding in critically ill patients. N Engl J Med 1994;330:377-81. [Crossref] [PubMed]
- Tjwa ET, Holster IL, Kuipers EJ. Endoscopic management of nonvariceal, nonulcer upper gastrointestinal bleeding. Gastroenterol Clin North Am 2014;43:707-19. [Crossref] [PubMed]
- van der Voort PH, van der Hulst RW, Zandstra DF, et al. Gastrointestinal endoscopy in the intensive care unit:a prospective one year study. Chapter 2, Thesis, University of Amsterdam 1999. Available online: , accessed on October 8th 2017.https://pure.uva.nl/ws/files/3360519/5759_UBA003000168_005.pdf
- El-Kersh K, Jalil B, McClave SA, et al. Enteral nutrition as stress ulcer prophylaxis in critically ill patients: A randomized controlled exploratory study. J Crit Care 2017;43:108-13. [Crossref] [PubMed]
- Alhazzani W, Guyatt G, Alshahrani M, et al. Withholding Pantoprazole for Stress Ulcer Prophylaxis in Critically Ill Patients: A Pilot Randomized Clinical Trial and Meta-Analysis. Crit Care Med 2017;45:1121-9. [Crossref] [PubMed]
- Zandstra DF, Stoutenbeek CP. The virtual absence of stress-ulceration related bleeding in ICU patients receiving prolonged mechanical ventilation without any prophylaxis. A prospective cohort study. Intensive Care Med 1994;20:335-40. [Crossref] [PubMed]
- Howard TJ, Plaskon LA, Wiebke EA, et al. Nonocclusive mesenteric ischemia remains a diagnostic dilemma. Am J Surg 1996;171:405-8. [Crossref] [PubMed]
- van der Voort PH, Westra B, Wester JP, et al. Can serum L-lactate, D-lactate, creatine kinase and I-FABP be used as diagnostic markers in critically ill patients suspected for bowel ischemia. BMC Anesthesiology 2014;14:111. [Crossref] [PubMed]
- Cook DJ, Griffith LE, Walter SD, et al. The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients. Critical Care 2001;5:368-75. [Crossref] [PubMed]
- Krag M, Perner A, Wetterslev J, et al. Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med 2015;41:833-45. [Crossref] [PubMed]
- Krag M, Perner A, Wetterslev J, et al. Stress ulcer prophylaxis in the intensive care unit: an international survey of 97 units in 11 countries. Acta Anaesthesiol Scand 2015;59:576-85. [Crossref] [PubMed]
- Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign:International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med 2017;43:304-77. [Crossref] [PubMed]
- Rafinazari N, Abbasi S, Farsaei S, et al. Adherence to stress-related mucosal damage prophylaxis guideline in patients admitted to the Intensive Care Unit. J Res Pharm Pract 2016;5:186-92. [Crossref] [PubMed]
- Alquraini M, Alshamsi F, Møller MH, et al. Sucralfate versus histamine 2 receptor antagonists for stress ulcer prophylaxis in adult critically ill patients: A meta-analysis and trial sequential analysis of randomized trials. J Crit Care 2017;40:21-30. [Crossref] [PubMed]
- Barletta JF, Bruno JJ, Buckley MS, et al. Stress Ulcer Prophylaxis. Crit Care Med 2016;44:1395-405. [Crossref] [PubMed]
- Alshamsi F, Belley-Cote E, Cook D, et al. Efficacy and safety of proton pump inhibitors for stress ulcer prophylaxis in critically ill patients: a systematic review and meta-analysis of randomized trials. Crit Care 2016;20:120. [Crossref] [PubMed]
- Plummer MP, Blaser AR, Deane AM. Stress ulceration: prevalence, pathology and association with adverse outcomes. Crit Care 2014;18:213. [Crossref] [PubMed]
- Krag M, Perner A, Wetterslev J, et al. Stress ulcer prophylaxis versus placebo or no prophylaxis in critically ill patients. A systematic review of randomised clinical trials with meta-analysis and trial sequential analysis. Intensive Care Med 2014;40:11-22. [Crossref] [PubMed]
- Krag M, Perner A, Wetterslev J, et al. Stress ulcer prophylaxis in the intensive care unit: is it indicated? A topical systematic review. Acta Anaesthesiol Scand 2013;57:835-47. [Crossref] [PubMed]
- Alhazzani W, Alenezi F, Jaeschke RZ, et al. Proton pump inhibitors versus histamine 2 receptor antagonists for stress ulcer prophylaxis in critically ill patients:a systematic review and meta-analysis. Crit Care Med 2013;41:693-705. [Crossref] [PubMed]
- Pilkington KB, Wagstaff MJ, Greenwood JE. Prevention of gastrointestinal bleeding due to stress ulceration: a review of current literature. Anaesth Intensive Care 2012;40:253-9. [PubMed]
- Selvanderan SP, Summers MJ, Finnis ME, et al. Pantoprazole or Placebo for Stress Ulcer Prophylaxis (POP-UP): Randomized Double-Blind Exploratory Study. Crit Care Med 2016;44:1842-50. [Crossref] [PubMed]
- Ro Y, Eun CS, Kim HS, et al. Risk of Clostridium difficile Infection with the Use of a Proton Pump Inhibitor for Stress Ulcer Prophylaxis in Critically Ill Patients. Gut Liver 2016;10:581-6. [Crossref] [PubMed]
- Liu B, Liu S, Yin A, et al. Risks and benefits of stress ulcer prophylaxis in adult neurocritical care patients:a systematic review and meta-analysis of randomized controlled trials. Crit Care 2015;19:409. [Crossref] [PubMed]
- O’Keefe GE, Gentilello LM, Maier RV. Incidence of infectious complications associated with the use of histamine2-receptor antagonists in critically ill trauma patients. Ann Surg 1998;227:120-5. [Crossref] [PubMed]
- Wood JD. Neurotransmission at the interface of sympathetic and enteric divisions of the autonomic nervous system. Chin J Physiol 1999;42:201-10. [PubMed]
- Tan B, Norman R, Litton E, et al. Incidence and cost of stress ulcer prophylaxis after discharge from the intensive care unit:a retrospective study. Crit Care Resusc 2016;18:270-4. [PubMed]
- Hammond DA, Kathe N, Shah A, et al. Cost-Effectiveness of Histamine2 Receptor Antagonists Versus Proton Pump Inhibitors for Stress Ulcer Prophylaxis in Critically Ill Patients. Pharmacotherapy 2017;37:43-53. [Crossref] [PubMed]
- Khorvash F, Abbasi S, Meidani M, et al. The comparison between proton pump inhibitors and sucralfate in incidence of ventilator associated pneumonia in critically ill patients. Adv Biomed Res 2014;3:52. [Crossref] [PubMed]
- Scarpignato C, Gatta L, Zullo A, et al. Effective and safe proton pump inhibitor therapy in acid-related diseases - A position paper addressing benefits and potential harms of acid suppression. BMC Med 2016;14:179. [Crossref] [PubMed]
Cite this article as: van der Voort PH. How to prevent and treat gastrointestinal bleeding in the critically ill patient: a pathophysiological approach. J Emerg Crit Care Med 2017;1:35.


