Damage control resuscitation in patients with major trauma: prospects and challenges
Introduction
Trauma continues being a leading cause of death across the globe, especially for younger ages (1). When analyzing trauma related deaths, acute traumatic hemorrhage is one of the leading reasons—along with brain injuries—of mortality (2). Major trauma resuscitation has been through a long journey to our current standard of care which has improved the outcome of the patients. During the last 40 years there is a gradual trend to move from a universal and dogmatic approach to a more patient tailored strategy (3). In trauma care, anatomy is becoming less important and physiology has progressively taken its place under the spotlight.
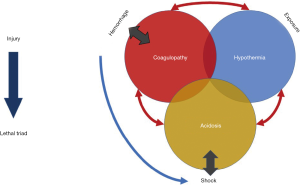
Once an actively bleeding patient has been recognized, then the modern resuscitative approach focuses on stopping the bleeding, replacing the circulating blood volume, and correcting trauma related physiological complications such as trauma induced coagulopathy. During the last few the new term of damage control resuscitation (DCR) has been introduced to describe this kind of approach, prioritizing hemostasis over maintaining a “normal” perfusing blood pressure (3). DCR encompasses different strategies aiming to reverse the physiological consequences of what is known as the lethal triad of trauma: hypothermia, coagulopathy and acidosis (4). This sinister triad creates a catastrophic physiological situation in patients who are in extremis after severe injury. Traditional strategies making use of aggressive fluid resuscitation, and surgical procedures aiming to provide definitive treatment to the injuries act as a “second hit” further derailing the patient’s physiological status decreasing the patient’s immediate survival (5). In addition, in many cases where patients survive from this physiological derailment, they may never recover and be steered towards multiple organ failure leading to late mortality after injury.
This review paper aims to provide insight in the latest developments of DCR focusing on the concept of hemostatic resuscitation of multiple trauma patients.
The lethal triad of trauma
Apart of the anatomical considerations particular to the type of injury, major trauma patients with massive blood loss present a syndrome called the lethal triad. This encompasses acidosis, hypothermia and coagulopathy that are linked both to the events causing them but also to each other, creating a vicious circle (Figure 1) (6).
Acidosis
Uncontrolled blood loss eventually causes hypovolemia with reduction of the cardiac preload and consequently reduction of the heart contractility and of the arterial blood pressure. This is recognized by the baroreceptors mainly situated at the carotid sinus which trigger a sympathetic discharge leading to arteriole and veniole constriction (7). This compensatory mechanism reduces the blood flow of the skin, skeletal muscles and the gut in favor of the brain, heart and kidneys and initially manages to preserve a perfusing blood pressure to these organs. Nevertheless, the addition of excessive blood loss, endothelial damage and tissue injury causes peripheral tissue hypoperfusion with inadequate oxygen delivery, leading to anaerobic metabolism and accumulation of lactic acid. Acidosis renders the enzymatic systems inactive and causes impairment in multiple organs. In trauma patients the severity of acidosis correlates with the dysfunction of coagulation factors and predicts mortality (8). A pH of 7.1 will severely decrease fibrin formation, by decreasing its propagation phase by 50% (9). Severe acidosis has been shown to act on the other clotting factors, reducing the activity of factor VIIa by 90% and of factors Xa/Va by 70% (8,9).
Hypothermia
Trauma patients commonly present with hypothermia on arrival due to exposure, blood loss, and administration of unwarmed fluids. Based on the patient’s core temperature hypothermia is classified as severe (<32 °C), moderate (32–33.9 °C) and mild (34–36 °C). Risk of hypothermia is not uniquely present in cold climates as data from Iraq and Afghanistan show that 9.8% of combat trauma patients present hypothermia. In these patients, severe hypothermia <32 °C was correlated with an increased injury severity score (ISS) and had almost half the survival of normothermic trauma patients (10). The effects of hypothermia are equally catastrophic in the civilian setting, and patients in severe hypothermia requiring emergency laparotomy have a mortality reaching 100% (11,12). Moderate hypothermia directly inhibits platelet aggregation and decreases coagulation factor activity by 10% for each degree of core temperature drop (13,14).
Coagulopathy
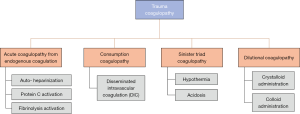
Coagulopathy is a major component of the lethal triad directly exacerbating hemorrhage. Both acidosis and hypothermia can cause coagulopathy with the mechanisms previously discussed (8,9,13,14). In addition to the coagulopathy of the lethal triad researchers recognize three other categories of coagulopathy related to trauma: acute traumatic coagulopathy from endogenous anticoagulation, consumptive coagulopathy and dilutional coagulopathy (15,16). The first one is observed in one-third of trauma patients and is characterized by a prolongation of the prothrombin time together with prolonged clotting time in viscoelastic hemostatic assays (VHAs) (17-20). The trigger for this endogenous anticoagulation is extensive endothelial damage causing in parallel auto-heparinization, protein C activation and increased fibrinolysis (21,22). Auto-heparinization occurs when microvascular trauma fragments the endothelial glycocalyx releasing molecules with heparin-like activity in the blood stream (23). Consumptive coagulopathy is believed to be caused by disseminated intravascular coagulation (DIC) from failure of the hemostatic mechanism to keep the balance between coagulation and fibrinolysis (24). Last, dilutional coagulopathy is the result of the administration of large volumes of crystalloid intravenous fluids in patients with severe bleeding, which leads to dilution of the coagulation factors; the severity of this coagulopathy is relative to the infused fluid volumes (25). The infusion of synthetic colloids such as hydroxyethyl starch interferes directly with the platelet and the factor XIIIa function, further aggravating the coagulopathy (26). Failure to address the aforementioned physiological imbalances, leads to non-salvageable situations where the trauma victim succumbs to the lethal triad in spite of the prompt resuscitation attempts.
Damage control resuscitation
DCR is a staged strategy addressing the physiological derailment of major trauma patients by prioritizing the restoration of physiological function and the reversal of the lethal triad over the definitive treatment of the injury (8). Trauma patients in extremis cannot tolerate complex and prolonged surgical procedures. As such life-saving interventions are performed in the retrieval and emergency setting in order to stabilize the patient’s physiological status. Trauma protocols prioritize now catastrophic bleeding over other life-threatening condition by implementing the C-ABCDE approach (27-29). Damage control surgery (DCS) is similarly targeting life-threatening conditions while deferring treatment of non-vital injuries to a later stage. Physiological optimization is undertaken in the ICU and definitive surgical treatment is undertaken only after normalization of the patient status (Figure 2) (12).
One of the primary goals of DCR is the reversal of the lethal triad of hypothermia, acidosis and coagulopathy. Hypothermia is addressed by limiting the patient’s exposure with passive warming using insulating blankets and active external warming with the use of air heaters. These methods usually the core temperature increases by 2 °C each hour. Use of active internal warming by administration of warm intravenous, intravesical and intragastric fluids is a more aggressive way to increase the core temperature by 4–5 °C per hour (30). There are observational data showing improved outcomes when using extracorporeal membrane oxygenation for warming patients in cardiopulmonary arrest and hypothermia (31).
There is no specific method for the reversal of acidosis in trauma patients. Administration of sodium bicarbonate will transiently increase the pH but will also cause a build-up of carbon dioxide leading to intracellular acidosis. This in turn causes depression of the myocardial contractility worsening the tissue hypoperfusion. A large randomized controlled trial (RCT) from France used sodium bicarbonate in Intensive Care Unit patients with severe acidemia (pH ≤7.2) in order to maintain a pH of >7.3 but did not show any overall survival benefit of these patients when compared with the control group (32). On the other hand, early appropriate care of trauma patients has been shown to reduce exposure to acidosis and decrease complications. In a prospective cohort study including 332 patients with major trauma, defined by an ISS ≥16, had their fractures fixated within 36 hours of admission. When compared to an historic cohort, they had fewer complications with the only independent predictors of complication rate being the ISS and the time to achieve early appropriate care (33). As such the treatment of acidosis should be focused in providing early definitive care of injuries and maintaining an adequate tissue perfusion with peripheral delivery of oxygen.
Hypotensive resuscitation
Optimization of the peripheral tissue perfusion in trauma patients is another issue that has changed in the last years. In the past the goal was to maintain a “normal” perfusing pressure and several clinical endpoints as the heart rate, peripheral pulse and blood pressure were used, but their use is unreliable (34). More than two decades ago, Bickell et al. reported that patients with penetrating torso injuries not receiving any intravenous crystalloids before arriving in the operating room had a better survival had a better survival (70% vs. 62%, P=0.04), reduced morbidity an and a shorter hospital stay when compared to those who received aggressive fluid resuscitation (35). This gave birth to the concept of permissive hypotension in trauma resuscitation; the goal is to keep the arterial blood pressure low enough to avoid clot dislodgement and exacerbation of arterial hemorrhage while maintaining an adequate perfusing pressure. In practice a systolic blood pressure of 80–90 mmHg is allowed until the patient is brought in the operating room for surgical hemostasis (36). Several studies have reported a survival benefit when using this strategy when compared with aggressive intravenous crystalloid fluids administration. A recent metanalysis pooling 1,158 patients showed that patients treated with permissive hypotension had a survival benefit (odds ratio: 0.70, 95% confidence interval: 0.53–0.92), received fewer blood products and had lesser estimated blood loss. However, most of the studies were underpowered and there was heterogeneity in the systolic blood pressures used as well as in the inclusion of patients with blunt and penetrating injuries (37). An important caveat is the application permissive hypotension in patients with head injury as in these cases hypotension is poorly tolerated. Preservation of cerebral perfusing pressure is of the utmost importance in head-injured patients, as a drop of systolic blood pressure <90 mmHg has been implicated in a two-fold increase of mortality (38).
Mechanical hemostasis
Hemorrhage control is of critical importance as the patient’s own blood is the ideal fluid to retain circulation volume. A variety of methods have been suggested and used with a great variability of outcomes. van Oostendorp et al. have published a review of more than 70 articles of the literature summarizing the available modalities and their outcome but concluded that the level of evidence was quite low (39). Most of these modalities have been created for the prehospital settings, nevertheless they have also seen application in the emergency department. Direct wound pressure remains the optimal approach for external bleeding wounds, where tourniquets and splinters have been used mainly for limp control with or without bone fractures. In particular, tourniquets have emerged as the ideal hemostatic modality for mangled extremities in the civilian setting, after extrapolation of data showing that they are lifesaving in the combat setting (40). In addition, public awareness and education programs such as “Stop the Bleed” organized by the American College of Surgeons has drastically increased the number of laypersons that are capable of applying tourniquets (41). It should be noted though that in spite of training, in an important number of cases in the prehospital setting, tourniquets can be either inappropriately placed or not placed in patients that required them by the emergency medical teams (42). Hemostatic modalities such as wound clamps, injectable hemostatic sponges, pelvic circumferential stabilizers, intra-abdominal gas insufflation, and intra-abdominal self-expanding foam have been used with a low level of evidence (39). Others such as pelvic binders are currently not supported by a high level of evidence.
Resuscitative thoracotomy (RT) in the emergency department has been used widely for proximal control of bleeding in peri arrested and unstable patients. Indications include patients with penetrating thoracic and subdiaphragmatic injuries that have signs of life at the scene and arrive at the emergency department with organized cardiac activity (43). A recent analysis of data from Europe showed that in 887 patients receiving emergency department thoracotomy, survival rates of 4.8% for blunt and 20.7% for penetrating trauma (44). However, data from a national cohort study in Japan with 1,377 critical blunt trauma patients who received cardiopulmonary resuscitation in the emergency department found out that the patients who had RT had a lower one-month survival when compared to those having closed-chest compression (1.2% vs. 6.0%, P<0.001). In addition, RT requires surgical expertise, available material and has relatively high collateral complications. That’s why the last decade other alternatives have been proposed such as the Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA), where the descending thoracic aorta is occluded by a balloon catheter inserted in the emergency department (45). Observational data from 285 patients show that when REBOA is applied in patients in extremis or near arrest without penetrating thoracic injuries, it achieves superior survival beyond the emergency department (RT: 44%, REBOA: 63%; P=0.004) and survival to discharge (RT: 2.5%, REBOA: 9.6%; P=0.023) (46). In general, trauma patients with signs of life on site arriving at the emergency room with an organized cardiac function can be candidates for RT if they have penetrating chest injuries and for REBOA if they don’t. Both techniques have their indications but require availability of material, expertise and standardization of the treatment protocols in order to improve the survival of these severely injured patients.
Hemostatic resuscitation
In the last decade, trauma resuscitation has gone far away from the dogma of aggressive intravenous crystalloid administration that dominated previously. It started being evident more than 15 years ago that the blood volume of patients with massive bleeding should be replaced with the same element lost—blood (47). Soon, more and more data emerged supporting that the administration of packed red blood cells (PRBCs), fresh frozen plasma (FFP) and platelets had a survival benefit when compared with the administration of crystalloids and colloids in trauma (48). The Prospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study analyzed 905 trauma patients requiring three or more units of blood production within 24 h of the injury. It found out that an early administration of high dose FFP and platelets in a ratio of 1:1:1 significantly reduced early mortality (49). This transfusion strategy for major hemorrhage was also validated by the Pragmatic Randomized Optimal Platelet and Plasma Ratios (PROPPR) trial which randomized 680 injured patients with major hemorrhage in receiving FFP: platelets: PRBC in a ratio of 1:1:1 compared to a ratio of 1:1:2. In the 1:1:1 group a higher percentage of patients achieved hemostasis (86% vs. 78%, P=0.006), received less transfusions after the intervention and received less frequently cryoprecipitate (22% vs. 29%, P=0.01) but had the same mortality at 24 h with the 1:1:2 group (50). The 1:1:1 strategy is implemented in the transfusion protocols of major trauma of national authorities such as the National Institute of Clinical Excellence (NICE) in the UK (51). It is useful to know the existence of scoring systems such as the Trauma Associated Severe Hemorrhage, and the Assessment of Blood Consumption which can predict the need of massive blood transfusion (>10 units in 24 h) in trauma patients (52). Interestingly, there are reports that important heterogeneity in the massive transfusion protocols exists in Europe and the USA due to national and international differences in preparation and volume of blood components and in the interpretation of the 1:1:1 rule (53,54).
Tranexamic acid (TXA) is an inexpensive anti-fibrinolytic agent that blocks lysine-binding sites on plasminogen, effectively blocking the degradation of organized fibrin clots. The Clinical Randomization of an Antifibrinolytic in Significant Hemorrhage (CRASH-2) is a large multicentric RCT reported that trauma patients with suspected significant bleeding had increased survival when receiving TXA when compared to placebo (55). These results were validated in the military setting by the MATTERs trial and in the pediatric trauma setting by the PED-TRAX trial (56,57). In surgical patients, TXA reduces the probability to receive a transfusion (risk ratio: 0.62, 95% confidence interval: 0.58–0.65; P<0.001), and decreases mortality (0.61, 0.38–0.98; P=0.04) without increasing the risk of myocardial infarction, stroke, deep vein thrombosis and pulmonary embolism (58). Interestingly there are at least 126 published RCTs assessing the effect of TXA on blood transfusion in surgery making this one of the most redundant areas of study (59). TXA must be given within 3 h of injury in an intravenous dose of 1 g followed by a further 1 g infusion over 8 h. Due to its availability and ease of administration, it has been integrated in both prehospital and in-hospital trauma protocols (60).
Ionized serum calcium plays a very important role in hemostasis as it helps the binding of coagulation proteins on cellular membranes. Citrate contained in PRBC transfusion bags act as anticoagulant by eliminating calcium through chelation (7). Almost all trauma patients receiving massive transfusion of blood products manifest hypocalcemia which can be severe in trauma patients causes hypocalcemia which can be severe (ionized calcium <0.9 mmol/L) in 70% of cases. These patients with severe hypocalcemia have been found to have received a bigger number of transfusions, to have coagulopathy and a mortality two times higher than trauma patients with higher levels of ionized calcium (61). Ionized calcium decreases even after a transfusion of a single red blood cells unit and this drop increases with the number of transfused blood products (62). A prospective study of 591 critically ill trauma patients found that more than half of them had ionized calcium <1 mmol/L on admission. They had increased mortality (15.5% vs. 8.7%, P=0.036), received more multiple transfusions (17.1% vs. 7.1%, P=0.005) and more of them had massive transfusion (8.2% vs. 2.2%, P=0.017). Multivariable logistic regression analysis identified ionized calcium <1 mmol/L as an independent predictor of the need for multiple transfusions after adjusting for age and injury severity (odds ratio: 2.294, 95% confidence interval: 1.053–4.996) (63). The same findings are seen in major trauma patients that did not receive prehospital blood transfusion which means that mechanisms apart from the effect of the citrate in transfused products are responsible (64). Hypercalcitoninemia and inappropriate calciuria have been observed in major trauma patients and it is hypothesized that the calcium regulatory mechanisms may by disrupted in these patients (65). It seems that calcium plays an equally important role to the elements of the lethal triad in trauma coagulopathy and it should be closely monitored and corrected (66).
Thromboelastography (TEG) and rotational thromboelastometry (ROTEM) are two techniques measuring and displaying changes in the viscoelastic strength of a small sample of clotting blood to which a constant rotational force is applied. The analysis of these results allows the assessment of clot formation, propagation, stabilization and dissolution, effectively providing valuable information about the platelets, coagulation factors and fibrinolysis (67). The use of these VHA has been used to manage the administration of blood products during massive transfusion protocols. Gonzalez et al. randomized 111 injured patients meeting the criteria for massive blood transfusion to be managed either by TEG or by conventional coagulation assays including international normalized ratio (INR), fibrinogen and platelet count. The TEG group had a higher 28-day survival (19.6% vs. 36.4%, P=0.049), and consumed less units of FFP and platelets (68). In addition, a systematic review of 17 RCT with 1,493 bleeding patients, TEG or ROTEM when compared to transfusion guided by any other method had reduced overall mortality, less red blood cell, FFP and platelet transfusions, but with a low quality of evidence (69). Newer protocols are being developed incorporating TEG and ROTEM with hemostatic assays in order to identify early patients with trauma induced coagulopathy and to provide data-driven optimization of DCR in trauma patients (70).
In conclusion, major bleeding and trauma coagulopathy are two of the most important factors defining trauma patient survival. Modern resuscitation protocols can apply the principles of hemostatic resuscitation starting in the prehospital and continuing to the emergency room setting (71). The main targets are: a transfusion of blood products in a ratio of ≤2:1:1 (PRBC: FFP: platelets), warming of the patient and of the administered fluids, intravenous administration of 1 g of TXA within 3 h of injury and then infusion of another 1 g for 8 hours, use of VHA to optimize the transfusion strategy, minimization of active bleeding through permissive hypotension, and early bleeding control with mechanical means with early surgical or interventional control of the hemorrhage. As more data become available, we will be able to optimize the resuscitation of major trauma patients and avoid preventable deaths from hemorrhage.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Athanasios Chalkias) for the series “Recent Advances in Critical Emergency Medicine: From Pathophysiology to Clinical Practice” published in Journal of Emergency and Critical Care Medicine. The article was sent for external peer review organized by the Guest Editor and the editorial office.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jeccm-20-24). The series “Recent Advances in Critical Emergency Medicine: From Pathophysiology to Clinical Practice” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Norton R, Kobusingye O. Injuries. N Engl J Med 2013;368:1723-30. [Crossref] [PubMed]
- Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma 2006;60:S3-11. [Crossref] [PubMed]
- Harris T, Davenport R, Mak M, et al. The evolving science of trauma resuscitation. Emerg Med Clin North Am 2018;36:85-106. [Crossref] [PubMed]
- Duke MD, Guidry C, Guice J, et al. Restrictive fluid resuscitation in combination with damage control resuscitation: Time for adaptation. J Trauma Acute Care Surg 2012;73:674-8. [Crossref] [PubMed]
- Lasanianos NG, Kanakaris NK, Dimitriou R, et al. Second hit phenomenon: existing evidence of clinical implications. Injury 2011;42:617-29. [Crossref] [PubMed]
- Giannoudi M, Harwood P. Damage control resuscitation: lessons learned. Eur J Trauma Emerg Surg 2016;42:273-82. [Crossref] [PubMed]
- Hall EJ. Guyton and hall textbook of medical physiology, 13th edition. Philadelphia: Saunders, 2016.
- Kaafarani HM, Velmahos GC. Damage control resuscitation in trauma. Scand J Surg 2014;103:81-8. [Crossref] [PubMed]
- Martini WZ. Coagulopathy by hypothermia and acidosis: mechanisms of thrombin generation and fibrinogen availability. J Trauma 2009;67:202-8. [Crossref] [PubMed]
- Fisher AD, April MD, Schauer SG. An analysis of the incidence of hypothermia in casualties presenting to emergency departments in Iraq and Afghanistan. Am J Emerg Med 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Martin RS, Kilgo PD, Miller PR, et al. Injury-associated hypothermia: an analysis of the 2004 National Trauma Data Bank. Shock 2005;24:114-8. [Crossref] [PubMed]
- Morris JA Jr, Eddy VA, Blinman TA, et al. The staged celiotomy for trauma. Issues in unpacking and reconstruction. Ann Surg 1993;217:576-84; discussion 584-6. [Crossref] [PubMed]
- Beekley AC. Damage control resuscitation: a sensible approach to the exsanguinating surgical patient. Crit Care Med 2008;36:S267-74. [Crossref] [PubMed]
- Scharbert G, Kalb ML, Essmeister R, et al. Mild and moderate hypothermia increases platelet aggregation induced by various agonists: a whole blood in vitro study. Platelets 2010;21:44-8. [Crossref] [PubMed]
- Johansson PI, Stensballe J, Oliveri R, et al. How I treat patients with massive hemorrhage. Blood 2014;124:3052-8. [Crossref] [PubMed]
- Stensballe J, Ostrowski SR, Johansson PI. Haemostatic resuscitation in trauma: the next generation. Curr Opin Crit Care 2016;22:591-7. [Crossref] [PubMed]
- MacLeod JB, Lynn M, McKenney MG, et al. Early coagulopathy predicts mortality in trauma. J Trauma 2003;55:39-44. [Crossref] [PubMed]
- Brohi K, Singh J, Heron M, et al. Acute traumatic coagulopathy. J Trauma 2003;54:1127-30. [Crossref] [PubMed]
- Cotton BA, Faz G, Hatch QM, et al. Rapid thrombelastography delivers realtime results that predict transfusion within 1 h of admission. J Trauma 2011;71:407-14; discussion 414-7. [Crossref] [PubMed]
- Davenport R, Manson J, De’Ath H, et al. Functional definition and characterization of acute traumatic coagulopathy. Crit Care Med 2011;39:2652-8. [Crossref] [PubMed]
- Johansson PI, Henriksen HH, Stensballe J, et al. Traumatic endotheliopathy: a prospective observational study of 424 severely injured patients. Ann Surg 2017;265:597-603. [Crossref] [PubMed]
- Kashuk JL, Moore EE, Sawyer M, et al. Primary fibrinolysis is integral in the pathogenesis of the acute coagulopathy of trauma. Ann Surg 2010;252:434-42. [PubMed]
- Ostrowski SR, Johansson PI. Endothelial glycocalyx degradation induces endogenous heparinization in patients with severe injury and early traumatic coagulopathy. J Trauma Acute Care Surg 2012;73:60-6. [Crossref] [PubMed]
- Gando S, Sawamura A, Hayakawa M. Trauma, shock, and disseminated intravascular coagulation: lessons from the classical literature. Ann Surg 2011;254:10-9. [Crossref] [PubMed]
- Maegele M, Lefering R, Yucel N, et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8725 patients. Injury 2007;38:298-304. [Crossref] [PubMed]
- Rasmussen KC, Johansson PI, Hojskov M, et al. Hydroxyethyl starch reduces coagulation competence and increases blood loss during major surgery: results from a randomized controlled trial. Ann Surg 2014;259:249-54. [Crossref] [PubMed]
- Duchesne JC, McSwain NE Jr, Cotton BA, et al. Damage control resuscitation: the new face of damage control. J Trauma 2010;69:976-90. [Crossref] [PubMed]
- Jansen JO, Thomas R, Loudon MA, et al. Damage control resuscitation for patients with major trauma. BMJ 2009;338:b1778. [Crossref] [PubMed]
- Hussmann B, Lendemans S. Pre-hospital and early in-hospital management of severe injuries: changes and trends. Injury 2014;45 Suppl 3:S39-42. [Crossref] [PubMed]
- Shapiro MB, Jenkins DH, Schwab WC, et al. Damage control: a collective review. J Trauma 2000;49:969-78. [Crossref] [PubMed]
- Ohbe H, Isogai S, Jo T, et al. Extracorporeal membrane oxygenation improves outcomes of accidental hypothermia without vital signs: a nationwide observational study. Resuscitation 2019;144:27-32. [Crossref] [PubMed]
- Jaber S, Paugam C, Futier E, et al. Sodium bicarbonate therapy for patients with severe metabolic acidaemia in the intensive care unit (BICAR-ICU): a multicentre, open-label, randomised controlled, phase 3 trial. Lancet 2018;392:31-40. [Crossref] [PubMed]
- Weinberg DS, Narayanan AS, Moore TA, et al. Prolonged resuscitation of metabolic acidosis after trauma is associated with more complications. J Orthop Surg Res 2015;10:153. [Crossref] [PubMed]
- Deakin CD, Low JL. Accuracy of the advanced trauma life support guidelines for predicting systolic blood pressure using carotid, femoral, and radial pulses: observational study. BMJ 2000;321:673-4. [Crossref] [PubMed]
- Bickell WH, Wall MJ Jr, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 1994;331:1105-9. [Crossref] [PubMed]
- Geeraedts LMG, Pothof LAH, Caldwell E, et al. Prehospital fluid resuscitation in hypotensive trauma patients: do we need a tailored approach? Injury 2015;46:4-9. [Crossref] [PubMed]
- Tran A, Yates J, Lau A, et al. Permissive hypotension versus conventional resuscitation strategies in adult trauma patients with hemorrhagic shock: a systematic review and meta-analysis of randomized controlled trials. J Trauma Acute Care Surg 2018;84:802-8. [Crossref] [PubMed]
- Tobin JM, Dutton RP, Pittet JF, et al. Hypotensive resuscitation in a head-injured multi-trauma patient. J Crit Care 2014;29:313.e1-5. [Crossref] [PubMed]
- van Oostendorp SE, Tan EC, Geeraedts LMG. Prehospital control of life-threatening truncal and junctional haemorrhage is the ultimate challenge in optimizing trauma care; a review of treatment options and their applicability in the civilian trauma setting. Scand J Trauma Resusc Emerg Med 2016;24:110. [Crossref] [PubMed]
- Goodwin T, Moore KN, Paley JD, et al. From the Battlefield to main street: tourniquet acceptance, use, and translation from the military to civilian setting. J Trauma Acute Care Surg 2019;87:S35-9. [Crossref] [PubMed]
- Ross EM, Redman TT, Mapp JG, et al. Stop the bleed: the effect of hemorrhage control education on layperson’s willingness to respond during a traumatic medical emergency. Prehosp Disaster Med 2018;33:127-32. [Crossref] [PubMed]
- Duignan KM, Lamb LC, DiFiori MM, et al. Tourniquet use in the prehospital setting: are they being used appropriately? Am J Disaster Med 2018;13:37-43. [Crossref] [PubMed]
- DiGiacomo JC, Angus LDG. Thoracotomy in the emergency department for resuscitation of the mortally injured. Chin J Traumatol 2017;20:141-6. [Crossref] [PubMed]
- Schulz-Drost S, Merschin D, Gümbel D, et al. Emergency department thoracotomy of severely injured patients: an analysis of the TraumaRegister DGU®. Eur J Trauma Emerg Surg 2020;46:473-85. [Crossref] [PubMed]
- Howie W, Broussard M, Batoon B. Resuscitative endovascular balloon occlusion of the aorta (REBOA) as an option for uncontrolled hemorrhagic shock: current best practices and anesthetic implications. AANA J 2019;87:19-25. [PubMed]
- Brenner M, Inaba K, Aiolfi A, et al. Resuscitative endovascular balloon occlusion of the aorta and resuscitative thoracotomy in select patients with hemorrhagic shock: early results from the American Association for the Surgery of trauma's aortic occlusion in resuscitation for trauma and acute care surgery registry. J Am Coll Surg 2018;226:730-40. [Crossref] [PubMed]
- Johansson PI, Hansen MB, Sorensen H. Transfusion practice in massively bleeding patients: time for a change? Vox Sang 2005;89:92-6. [Crossref] [PubMed]
- Johansson PI, Oliveri R, Ostrowski SR. Hemostatic resuscitation with plasma and platelets in trauma. A meta-analysis. J Emerg Trauma Shock 2012;5:120-5. [Crossref] [PubMed]
- Holcomb JB, del Junco DJ, Fox EE, et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg 2013;148:127-36. [Crossref] [PubMed]
- Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA 2015;313:471-82. [Crossref] [PubMed]
- Glen J, Constanti M, Brohi K. Assessment and initial management of major trauma: summary of NICE guidance. BMJ 2016;353:i3051. [Crossref] [PubMed]
- Foster JC, Sappenfield JW, Smith RS, et al. Initiation and termination of massive transfusion protocols: current strategies and future prospects. Anesth Analg 2017;125:2045-55. [Crossref] [PubMed]
- Rijnhout TWH, Noorman F, Bek A, et al. Massive transfusion in The Netherlands. Emerg Med J 2020;37:65-72. [Crossref] [PubMed]
- Etchill E, Sperry J, Zuckerbraun B, et al. The confusion continues: results from an American Association for the Surgery of Trauma survey on massive transfusion practices among United States trauma centers. Transfusion 2016;56:2478-86. [Crossref] [PubMed]
- CRASH-2 trial collaborators, Shakur H, Roberts I, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet 2010;376:23-32.
- Morrison JJ, Dubose JJ, Rasmussen TE, et al. Military application of tranexamic acid in trauma emergency resuscitation (MATTERs) study. Arch Surg 2012;147:113-9. [Crossref] [PubMed]
- Eckert MJ, Wertin TM, Tyner SD, et al. Tranexamic acid administration to pediatric trauma patients in a combat setting: the pediatric trauma and tranexamic acid study (PED-TRAX). J Trauma Acute Care Surg 2014;77:852-8. [Crossref] [PubMed]
- Ker K, Edwards P, Perel P, et al. Effect of tranexamic acid on surgical bleeding: systematic review and cumulative meta-analysis. BMJ 2012;344:e3054. [Crossref] [PubMed]
- Ker K, Roberts I. Exploring redundant research into the effect of tranexamic acid on surgical bleeding: further analysis of a systematic review of randomised controlled trials. BMJ Open 2015;5:e009460. [Crossref] [PubMed]
- Wafaisade A, Lefering R, Bouillon B, et al. Prehospital administration of tranexamic acid in trauma patients. Crit Care 2016;20:143. [Crossref] [PubMed]
- Giancarelli A, Birrer KL, Alban RF, et al. Hypocalcemia in trauma patients receiving massive transfusion. J Surg Res 2016;202:182-7. [Crossref] [PubMed]
- Webster S, Todd S, Redhead J, et al. Ionised calcium levels in major trauma patients who received blood in the Emergency Department. Emerg Med J 2016;33:569-72. [Crossref] [PubMed]
- Magnotti LJ, Bradburn EH, Webb DL, et al. Admission ionized calcium levels predict the need for multiple transfusions: a prospective study of 591 critically ill trauma patients. J Trauma 2011;70:391-5; discussion 395-7. [Crossref] [PubMed]
- Vasudeva M, Mathew JK, Fitzgerald MC, et al. Hypocalcaemia and traumatic coagulopathy: an observational analysis. Vox Sang 2020;115:189-95. [Crossref] [PubMed]
- Koch SM, Mehlhorn U, Baggstrom E, et al. Hypercalcitoninemia and inappropriate calciuria in the acute trauma patient. J Crit Care 1996;11:117-21. [Crossref] [PubMed]
- Ditzel RM Jr, Anderson JL, Eisenhart WJ, et al. A review of transfusion- and trauma-induced hypocalcemia: is it time to change the lethal triad to the lethal diamond? J Trauma Acute Care Surg 2020;88:434-9. [Crossref] [PubMed]
- Whiting D, DiNardo JA. TEG and ROTEM: technology and clinical applications. Am J Hematol 2014;89:228-32. [Crossref] [PubMed]
- Gonzalez E, Moore EE, Moore HB, et al. Goal-directed hemostatic resuscitation of trauma-induced coagulopathy: a pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays. Ann Surg 2016;263:1051-9. [Crossref] [PubMed]
- Wikkelsø A, Wetterslev J, Møller AM, et al. Thromboelastography (TEG) or thromboelastometry (ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding. Cochrane Database Syst Rev 2016.CD007871. [PubMed]
- Baksaas-Aasen K, Van Dieren S, Balvers K, et al. Data-driven development of ROTEM and TEG algorithms for the management of trauma hemorrhage: a prospective observational multicenter study. Ann Surg 2019;270:1178-85. [Crossref] [PubMed]
- Wijesuriya JD, Keogh S. Integrated major haemorrhage management in the retrieval setting: damage control resuscitation from referral to receiving facility. Emerg Med Australas 2017;29:470-5. [Crossref] [PubMed]
Cite this article as: Ntourakis D, Liasis L. Damage control resuscitation in patients with major trauma: prospects and challenges. J Emerg Crit Care Med 2020;4:34.