
Transient hypotension from intravenous acetaminophen in adolescent post-operative posterior spinal fusion surgery
Introduction
Intravenous (IV) acetaminophen has become an important part for non-opioid based analgesic post-surgically. The use of IV acetaminophen has been assumed to be safe without significant side effects. However, recent adult and pediatric literature has shown that IV acetaminophen may not be as benign as we once originally thought (1-3). In fact, IV acetaminophen has been shown to cause transient hypotension in the sicker intensive care pediatric patients (1,4).
The mechanism for this effect is still unknown. Some have speculated that mannitol used to stabilize IV acetaminophen fluid concentration could be the reason for this transient hypotension (5,6). Because of mannitol, there is significant increase in UOP and renal vasodilation leading to redistribution of systemic blood flow (7). Yet in Chiam et al.’s adult prospective study, these effects were only seen in the IV acetaminophen group and not in the mannitol or normal saline group (8).
If this transient hypotension effect is correct, then cardiovascularly healthy post-surgical patients who undergo larger blood loss during surgery, high inflammation leading to increase vascular permeability, and increased fluid changes post-surgical are at greater risk for hemodynamic instability. One surgery in which patients undergo prolonged substantial blood loss, inflammation, and fluid changes is posterior spinal fusion (PSF) surgery. Therefore, this study was performed to investigate a cardiovascularly healthy adolescent population receiving scheduled IV acetaminophen after PSF surgery. The primary objective of this study was to see if there were transient hemodynamic effects after giving IV acetaminophen in a cardiovascularly healthy adolescent population directly after PSF surgery. The secondary objectives of this study were to see if transient hypotension was associated with changes in urine output (UOP), and if these transient hemodynamic effects changed with subsequent IV acetaminophen dosing.
Methods
This study protocol was approved by the Naval Medical Center Portsmouth Institutional Review Board in compliance with all applicable federal regulations governing the protection of human subjects. Research data was derived from an approved IRB protocol: number NMCP.2019.0079. Written informed consent was not required by the Naval Medical Center Portsmouth IRB, as this data concerned historical de-identified patients.
Study design
This was a retrospective study of 28 cardiovascularly healthy adolescent patients (ages 10–20 years) who underwent PSF surgery for idiopathic or neuromuscular scoliosis and recovered in the PICU from 2014 to 2019. All patients involved in this study had 0-1 comorbid additional factors besides scoliosis and these patients did not have any concomitant abnormalities in their cardiac system. This population study was primarily female gender [20 (71.4%) female versus 8 (28.6%) male]. Patients involved in this study underwent PSF of 7-14 vertebral spinal bodies and had a spinal curvature of 30–82-degree Cobb angle. Estimated blood loss (EBL) and total IV fluids during surgery were recorded. Heart rates and mean arterial blood pressures (MAP), measured via arterial line monitoring, and urine output (UOP), were measured via a Foley catheter, were recorded and analyzed every hour, from right before to 4 hours after an IV acetaminophen dose was given. IV acetaminophen was dosed at 10–15 mg/kg per dose for those less than 50 kg and 1 g per dose for those greater than 50 kg. The IV acetaminophen dose was given as an infusion over 15 minutes. This dosing strategy was used in our study since it is the standard dosing by the manufacturer of Ofirmev for every 6 hours frequency (9). Directly after PSF surgery and at PICU admission, patients received scheduled IV acetaminophen every 6 hours, constant ketamine infusion (3–5 mcg/kg/min IV), and isotonic maintenance IV fluids. Absolute hypotension was defined as a patient with a MAP decreased by 15% or more from baseline MAP obtained before IV acetaminophen dose was given, and relative hypotension was defined as a patient with a MAP decreased by 10–14% from baseline MAP obtained before IV acetaminophen dose was given. Non-hypotension was defined as a patient with a MAP that did not decrease by more than 9% from baseline MAP obtained before IV acetaminophen dose was given. Patients did not receive other medications that affected hemodynamics from 1 hour before to 1 hour after an IV acetaminophen dose.
Statistics
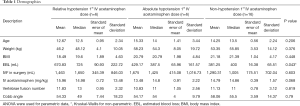
All statistics performed in this study were calculated using SPSS Statistics program (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY, USA: IBM Corp). The three groups were defined as absolute hypotension, relative hypotension, versus non-hypotension, and the descriptive factors were compared using ANOVA or Kruskal-Wallis tests, for parametric or non-parametric data respectively. These included age, weight, BMI, IV fluids given during surgery, IV acetaminophen dosage, number of vertebrae fused, vertebrae Cobb angle, and EBL (Table 1). A repeated measures mixed ANOVA were ran for HR, MAP, and UOP, in order to determine the effect of IV acetaminophen over time, as well as between groups. Mauchly’s test determined the assumption of sphericity for all two-way interactions, and adjustments were made when appropriate. All analysis was conducted at a significance level of 0.05.
Full table
Results
Twenty-eight cardiovascularly healthy adolescent patients underwent scheduled IV acetaminophen directly after PSF surgery. The first 3 scheduled doses (total of 84 doses), were used for analysis since this is an area of concern for hemodynamic instability directly post-operative. Characteristics of this patient cohort are found in Table 1. There was a significant difference in EBL during surgery between the absolute hypotension, relative hypotension, and non-hypotension groups (P=0.043, Table 1). There was no significant difference in baseline MAP between each group (P=0.155). Each IV acetaminophen dose was analyzed separately to explore if there were changes or persistent transient hypotensive effects with each subsequent IV acetaminophen dose.
Twenty-one patients (75%) experienced transient hypotension immediately after surgery. Absolute hypotension was seen in 21.4–28.6% and relative hypotension was seen in 7.1–28.6% of the population within each given IV acetaminophen dose. Two patients experienced episodes of hypotension requiring a normal saline fluid bolus to resolve (7.1%). Zero patients required vasopressor support or blood transfusions intra- or post-operatively (Table 2).
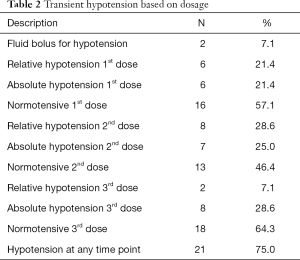
Full table
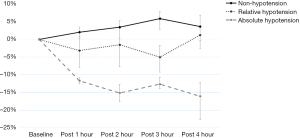
Significant hypotension changes were seen within the first hour after an IV acetaminophen dose was given. For the absolute hypotension group, all doses compared to relative hypotension and non-hypotension groups reached −15% change around 2 hours after an IV acetaminophen dose was given. The absolute hypotension group stayed hypotensive up to 4 hours after an IV acetaminophen dose was given. On average, the relative hypotension group did not experience significant hypotension and had greater variance per dose over hours after an IV acetaminophen dose was given (Figure 1).
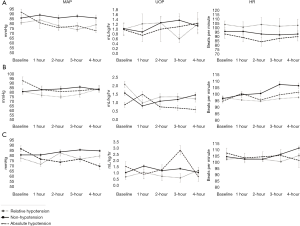
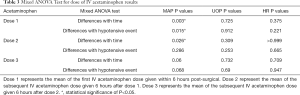
While MAP was statistically different between each hypotension group for the first dose (P=0.015), it was not statistically different for the second (P=0.286) or the third (P=0.068) IV acetaminophen doses given. UOP changes did not vary between each hypotension group (P=0.912 for dose 1, P=0.253 for dose 2, and P=0.69 for dose 3). Lastly, HR changes were not found to be significantly different between each hypotension group (Figure 2, Table 3).
Full table
Discussion
This study is the first to look at IV acetaminophen’s hemodynamic effects in a cardiovascularly healthy adolescent population immediately following PSF surgery. This is an important population since PSF is known to cause high inflammation and excessive blood loss leading to significant fluid shifts in each patient (10-14). This makes a cardiovascularly healthy population vulnerable to any hemodynamic changes.
We found that only absolute hypotension, as defined by a 15% or more MAP decrease from baseline MAP obtained prior to IV acetaminophen dose given, represented true blood pressure differences from those who remained normotensive (Figure 1). This subset of the population had significantly higher EBL during surgery (P=0.043, Table 1). It was this population that even had 7.1% of the population requiring normal saline fluid boluses to resolve their hypotension immediately after their first dose of IV acetaminophen. Thus, it can be concluded that those who experience greater EBL from surgery should not necessarily receive IV acetaminophen immediately after surgery during PICU recovery.
In IV acetaminophen concentrations, mannitol is used to stabilize the solution and can be seen up to 3.85 g per 100 mL of acetaminophen solution (9). Mannitol, even in small amounts, can cause hypotension via a significant increase in UOP and renal vasodilation (7). Therefore, our study looked at UOP differences between those who experienced relative hypotension and absolute hypotension compared to those who remained normotensive after an IV acetaminophen dose was given. No significant differences in UOP were found between each hypotension group (Table 3 and Figure 2). In addition, there was no significant increase in UOP 1 hour after IV acetaminophen dose administration. Thus, our results agree with Chiam et al.’s adult study suggesting that mannitol does not play a role in the transient hypotensive effects seen after IV acetaminophen dose administration (8).
Another novelty about this study was that we explored the effects of repeated IV acetaminophen doses in a patient within the first 24 hours after surgery. Interestingly, we saw that IV acetaminophen had significant hypotensive effects after the first dose (P=0.015, which was given in the first 6 hours post-operatively), but did not have significant blood pressure effects with subsequent every 6 hours scheduled doses 2 (P=0.286) and 3 (P=0.068) (Table 3). This hints to a possible adaptive response, therefore making the effects of excipients of IV acetaminophen (such as cysteine) more likely to be the mechanism for transient hypotension. Since surgeries such as PSF are known to cause a significant increase in pro-inflammatory cytokines immediately after surgery (14), any additional pro-inflammatory response can lead to loss of vascular tone, causing hypotension. Since IV acetaminophen leads to a rise in systemic cysteine levels, this can lead to a rise in interleukin (IL)-1β, which is known to cause hypotension via capillary leak (15). It thus makes sense that, the further away from surgery and the decreased baseline inflammation in a patient, the fewer significant transient hypotensive effects are seen (Figure 2).
Since little pediatric literature examines IV acetaminophen transient hypotensive effects (1,4), we used the Achuff et al. study as guidance to narrow the hemodynamic effects in a patient population that is also receiving potential hemodynamic altering medication. Therefore, we too choose only to analyze IV acetaminophen doses that did not have hemodynamically altering medication given 1 hour before or after IV acetaminophen dose administration. In our study’s population, this was also easier since the only potentially altering medication was the patient’s ketamine infusion (which was constant during this study’s analysis window).
When looking at the timing of IV acetaminophen’s transient hypotensive effects, it was shown that a significant change in blood pressure was seen within 1 hour after IV acetaminophen dose administration (Figure 1). This agrees with the sicker intensive care population in Achuff et al. study (1). However, we saw the peak IV acetaminophen hypotensive effects at 2 hours post IV acetaminophen dose administration (Figure 1). The reason for this 1 hour difference might be because this was a cardiovascularly healthy population that had a better ability to adapt their vascular tone. Another reason for this time difference in peak hypotensive effect, could be due to this study’s population receiving isotonic maintenance IV fluids during PICU admission. This addition can lead to increased intravascular volume leading to a delay of intravascular fluid loss and subsequently affecting peak hypotensive effects.
A limitation of this study is its population size. Due to the demand and length of time PSF surgery takes, only a few surgeries are performed per year. In order to increase the population size, this study would take over 10–15 years to generate a stronger statistically powered study. Even though this study’s population size does not generate a substantial statistical power, due to the novelty and results, this study should be used to construct further prospective studies of cardiovascularly healthy adolescents. Another limitation of our study is the frequency of blood pressure and UOP monitoring. We were only able to analyze changes every hour. However, hemodynamics are consistently changing. Thus, to make more precise hemodynamic trends post IV acetaminophen dose administration, minute by minute analysis would give even more precise trends. However, based on previous pediatric studies (1,4) the time frequency chosen was appropriate to see actual blood pressure changes due to IV acetaminophen dose administration.
Conclusions
IV acetaminophen is associated with transient hypotension in cardiovascularly healthy adolescents directly after PSF surgery. Most of the time, the hypotension experienced was transient and did not involve intervention. There was no significant trend with hypotension events and increase in UOP, making it less likely that mannitol is the underlying reason for the transient hypotension seen. Interestingly, there was a resolution of transient hypotension with subsequent IV acetaminophen doses.
Overall, based on this study’s results, it appears that IV acetaminophen is still an appropriate non-opioid based post-surgery analgesic for a cardiovascularly healthy adolescent population. However, caution must be given to withhold IV acetaminophen in high inflammatory excessive blood loss surgeries immediately after surgery.
Acknowledgments
We like to thank all Pediatric Intensivists and Pediatric Orthopedic Surgeons involved in patient care. We would also like to thank Andrea McGlynn with her help and guidance with statistics used in this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the Naval Medical Center Portsmouth Institutional Review Board in compliance with all applicable Federal regulations governing the protection of human subjects. Research data derived from an approved Naval Medical Center, Portsmouth, Virginia IRB, protocol; number NMCP.2019.0079.
Disclaimer: Dr. David Mari a military service member and Dr. Abhik Biswas is an employee of U.S. government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a United States Government work as a work prepared by a military service member or employee of the United States Government as part of that person’s official duties.
References
- Achuff BJ, Moffett BS, Acosta S, et al. Hypotensive Response to IV Acetaminophen in Pediatric Cardiac Patients. Pediatr Crit Care Med 2019;20:527-33. [Crossref] [PubMed]
- Maxwell EN, Johnson B, Cammilleri J, et al. Intravenous Acetaminophen-Induced Hypotension: A Review of the Current Literature. Ann Pharmacother 2019;53:1033-41. [Crossref] [PubMed]
- Cantais A, Schnell D, Vincent F, et al. Acetaminophen-Induced Changes in Systemic Blood Pressure in Critically Ill Patients: Results of a Multicenter Cohort Study. Crit Care Med 2016;44:2192-8. [Crossref] [PubMed]
- Allegaert K, Naulaers G. Haemodynamics of intravenous paracetamol in neonates. Eur J Clin Pharmacol 2010;66:855-8. [Crossref] [PubMed]
- Chiam E, Weinberg L, Bellomo R. Paracetamol: a review with specific focus on the haemodynamic effects of intravenous administration. Heart Lung Vessel 2015;7:121-32. [PubMed]
- de Maat MM, Tijssen TA, Brüggemann RJ, et al. Paracetamol for intravenous use in medium--and intensive care patients: pharmacokinetics and tolerance. Eur J Clin Pharmacol 2010;66:713-9. [Crossref] [PubMed]
- Bragadottir G, Redfors B, Ricksten SE. Mannitol increases renal blood flow and maintains filtration fraction and oxygenation in postoperative acute kidney injury: a prospective interventional study. Crit Care 2012;16:R159. [Crossref] [PubMed]
- Chiam E, Weinberg L, Bailey M, et al. The haemodynamic effects of intravenous paracetamol (acetaminophen) in healthy volunteers: a double-blind, randomized, triple crossover trial. Br J Clin Pharmacol 2016;81:605-12. [Crossref] [PubMed]
- The First and Only- OFIRMEV: Mallinckrodt Pharmaceuticals, 2018. Available online: http://www.ofirmev.com/downloads/pdf/OFIRMEVPharmacyFactSheet.pdf
- Lykissas MG, Crawford AH, Chan G, et al. The effect of tranexamic acid in blood loss and transfusion volume in adolescent idiopathic scoliosis surgery: a single-surgeon experience. J Child Orthop 2013;7:245-9. [Crossref] [PubMed]
- Liu JM, Fu BQ, Chen WZ, et al. Cell Salvage Used in Scoliosis Surgery: Is It Really Effective? World Neurosurg 2017;101:568-76. [Crossref] [PubMed]
- Oliveira JAA, Façanha Filho FAM, Fernandes FV, et al. Is cell salvage cost-effective in posterior arthrodesis for adolescent idiopathic scoliosis in the public health system? J Spine Surg 2017;3:2-8. [Crossref] [PubMed]
- Rumalla K, Yarbrough CK, Pugely AJ, et al. Spinal fusion for pediatric neuromuscular scoliosis: national trends, complications, and in-hospital outcomes. J Neurosurg Spine 2016;25:500-8. [Crossref] [PubMed]
- Alazawi W, Pirmadjid N, Lahiri R, et al. Inflammatory and Immune Responses to Surgery and Their Clinical Impact. Ann Surg 2016;264:73-80. [Crossref] [PubMed]
- Iyer SS, Accardi CJ, Ziegler TR, et al. Cysteine redox potential determines pro-inflammatory IL-1beta levels. PLoS One 2009;4:e5017. [Crossref] [PubMed]
Cite this article as: Mari D, Biswas A. Transient hypotension from intravenous acetaminophen in adolescent post-operative posterior spinal fusion surgery. J Emerg Crit Care Med 2020;4:15.


