
Communication expectations of critically ill patients and their families
Introduction
Family-centered care is defined as “an approach to health care that is respectful of and responsive to individual families’ needs and values” (1). In the intensive care unit (ICU), current guidelines recommend open or at least flexible visiting hours, and regular family meetings that are initiated within 24–48 hours (2). However, evaluations of actual practice indicate that these benchmarks are rarely met (3-6). Perhaps the most pressing question is not how clinicians can meet family members’ needs, but instead continuing to work toward identifying what behaviors constitute as family-centered care. For example, communication is cited by both surrogates and clinicians as families’ most important need, and yet, little is known about specific preferences and expectations for interacting with clinicians (1). Some basic questions remain that this study sought to answer—which clinicians do surrogates expect to communicate with first, and how frequently do they expect to speak with them? Answering these questions have important implications for whether and to what extent clinicians’ behaviors and intentions align with surrogates’ needs and expectations.
Methods
A panel of former patients and surrogate decision makers of a 20-bed medical ICU housed within a large academic hospital in the Midwest were recruited through a patient and family engagement program. A program administrator emailed a Qualtrics survey on behalf of the study team in order to protect program members’ identities, thus response rates are not known. All program members over the age of 18 were eligible to participate. Participation was voluntary and the study was deemed exempt by the institutional review board.
As part of a larger study on surrogate-clinician communication, participants were asked to provide demographic information, and then were instructed to imagine that an adult family member or close friend has been admitted to the ICU and placed on mechanical ventilation due to fluid in their lungs; they (the participants) were to envision acting as their loved one’s surrogate. Participants indicated which clinicians they expect to have talked to within 48 hours of their loved one being admitted to the ICU (the attending physician; registered nurse; respiratory therapist; resident or fellow; social worker), and how often they would like to interact with their loved one’s care team (multiple times a day; daily; a few times a week; once a week; other). Participants also responded to the following statements: “I prefer to have the care team contact me, rather than having to contact them” and “I feel confident that I know how to reach my loved one’s care team,” both of which were measured on 5-point Likert-type scales anchored by 1 (strongly disagree), and 5 (strongly agree). These items were based on social network analysis concepts such as degree centrality and tie strength.
Results
A panel of 44 participants completed the survey. A majority of participants were married white females in their mid-50’s who had received some education (see Table 1). While relatively homogeneous, this sample corresponds with other samples of surrogates of critically ill adults (7). A single participant was omitted from the following analysis because they only filled out the first page of the survey (i.e., demographics).

Full table
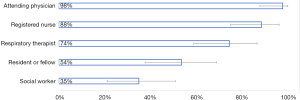
When asked about their expectations for communicating with specific clinicians, 42 participants (98%) expected to talk to the attending physician within 48 hours of their loved one being admitted to the ICU. A total of 38 participants (88%) expected to have talked to a registered nurse, and 32 (74%) to a respiratory therapist. Only approximately half (23 participants) expected to have talked to a resident or fellow, and roughly a third (15 participants) expected to talk with a social worker (see Figure 1).
Participants expected frequent communication with their loved one’s care team, with 44% expecting to be contacted multiple times a day, 51% expecting to be contacted daily, 2% expecting to be contacted a few times a week, and a single participant marked other, stating “more if health declines.” Regarding their preference for communication to be initiated by the care team, 32 participants (74%) agreed or strongly agreed. Of those remaining, 6 participants (14%) were neutral, and 5 (11%) strongly disagreed. Lastly, regarding confidence in being able to reach their loved one’s care team, 22 participants (51%) agreed or strongly agreed; 12 participants (28%) were neutral, and 9 (21%) disagreed or strongly disagreed.
Discussion
This study suggests that surrogates have different expectations for engagement with different clinicians. For example, attending physicians were expected to reach out to family members within 48 hours, and to continue to initiate contact daily if not multiple times a day. General practice is discordant with these expectations. One study found that as few as 40% of patients and families had discussions with attending physicians about prognoses or end of life care across a 2-week ICU stay, in a sample where only 20% of patients were expected to survive the next 6 months (8). The expectations for frequent communication with registered nurses are slightly more realistic in that they (the nurses) are much more accessible to families and thus have been the target of several interventions seeking to improve family communication (9,10). More work is needed to understand the expectation of frequent communication with respiratory therapists, especially considering that only approximately a third of participants had any prior experience with mechanical ventilation. Future studies might also explore underlying reasons why only half expected to interact with residents or fellows, whom often play central roles in care teams in academic hospitals.
Most participants preferred that the care team initiate contact. This could be related to the fact that only approximately half of the participants felt confident in knowing how to contact the care team. Interventions seeking to improve surrogate-clinician communication might consider targeting this knowledge gap.
This study is one of the first of its kind to describe specific expectations for clinician engagement. It is worth noting that these participants had recent experiences in the ICU; it is unclear whether families and surrogates with little to no prior experience in the ICU would hold similar expectations.
Conclusions
Expectations for surrogate-clinician communication are closer in alignment with current guidelines for family-centered care than they are with actual practice. While efforts to improve family members’ access to ICU providers should continue, it is important to consider the possible need to manage surrogates’ expectations to help ensure that they are able to capitalize on opportunities to interact with members of the care team that they may not recognize as valuable sources of information.
Acknowledgments
Funding: Dr. Ervin is receiving a grant from the National Heart, Lung, and Blood Institute (K12HL138039).
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: Participation was voluntary and the study was deemed exempt by the institutional review board. The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med 2017;45:103-28. [Crossref] [PubMed]
- Davidson JE, Powers K, Hedayat KM, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med 2007;35:605-22. [Crossref] [PubMed]
- Lilly CM, De Meo DL, Sonna LA, et al. An intensive communication intervention for the critically ill. Am J Med 2000;109:469-75. [Crossref] [PubMed]
- Curtis JR, Engelberg RA, Wenrich MD, et al. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844-9. [Crossref] [PubMed]
- Anderson WG, Cimino JW, Ernecoff NC, et al. A multicenter study of key stakeholders' perspectives on communicating with surrogates about prognosis in intensive care units. Ann Am Thorac Soc 2015;12:142-52. [Crossref] [PubMed]
- Liu V, Read JL, Scruth E, et al. Visitation policies and practices in US ICUs. Crit Care 2013;17:R71. [Crossref] [PubMed]
- Goldfarb MJ, Bibas L, Bartlett V, et al. Outcomes of patient- and family-centered care interventions in the ICU: A systematic review and meta-analysis. Crit Care Med 2017;45:1751-61. [Crossref] [PubMed]
- Teno JM, Fisher E, Hamel MB, et al. Decision-making and outcomes of prolonged ICU stays in seriously ill patients. J Am Geriatr Soc 2000;48:S70-4. [Crossref] [PubMed]
- Huffines M, Johnson KL, Smitz Naranjo LL, et al. Improving family satisfaction and participation in decision making in an intensive care unit. Crit Care Nurse 2013;33:56-69. [Crossref] [PubMed]
- White DB, Angus DC, Shields AM, et al. A randomized trial of family-support intervention in intensive care units. N Engl J Med 2018;378:2365-75. [Crossref] [PubMed]
Cite this article as: Ervin JN. Communication expectations of critically ill patients and their families. J Emerg Crit Care Med 2019;3:48.


