Echocardiographic assessment of left ventricular function
Critical care echocardiography is one of the most useful monitors for critically ill patients (1-4). Cardiac function and hemodynamic could be assessed non-invasively using this technique at the bedside and provide information which help clinicians to have a better management of intensive care unit (ICU) patients with hemodynamical compromise. 2D echocardiography, pulsed and continuous wave Doppler, colour Doppler, tissue Doppler imaging (TDI), speckle tracking and 3D imaging are the main techniques which improve the assessment of the cardiac function. Both transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) routes are used in ICU patients. TTE is sometimes limits due to the poor echogenicity of patients with chronic obstructive pulmonary disease (COPD), obesity or with high positive end-expiratory pressure (PEEP). As well presence of tapes on the chest after cardiac surgery may prevent to obtain good images to solve the clinical problem. Then TEE could be performed to overcome these limitations. But, many improvements as harmonic imaging, digital acquisition improved the performance of TTE. Then, TTE should be considered first in patient with unexplained shock or with respiratory failure. TTE is very useful when clinical signs are not enough to solve the clinical problem and then goal-directed echocardiography should be done. In ICU patients TTE is particularly useful because clinical situations are complexes and for instance septic shock could be associated with acute respiratory distress syndrome (ARDS) and then a comprehensive echocardiography should be done. More, TTE should be considered not only as an imaging technique but as a monitor which may help the clinician to follow hemodynamic changes and to decide either to give fluid or to start dobutamine or to increase noradrenalin infusion in patients which shock.
Assessment of systolic function and cardiac outputOther Section
- Assessment of systolic function and cardiac output
- Assessment of diastolic function and pulmonary arterial occlusive pressure (37-40)
- Clinical situations
- Conclusions
- Acknowledgments
- Footnote
- References
Left ventricular (LV) systolic function is a critical point to analyse in ICU patients with hemodynamic compromise to well analyse the pathophysiology of patient in shock or in respiratory failure. Echocardiography is considered as the first tool to assess this function. LV systolic function depends on preload, afterload, contractility and heart rate. Mainly, this systolic evaluation is done in ICU patients by assessing myocardial global and segmental contraction. Global assessment of LV includes determination of ejection fraction (EF) and cardiac output (5,6).
EF
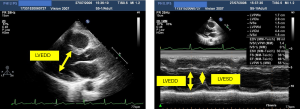
LV performance may be quantified by assessing EF (Figure 1). Shortening fraction is a surrogate parameter of EF and is obtained by using M-mode echocardiography from a parasternal long-axis view measuring left ventricular systolic dysfunction (LVSD) and left ventricular end-diastolic diameter (LVEDD) (Figure 1). Shortening fraction (SF) can be calculated as follow: SF (%) = (LVEDD − LVESD) × 100/LVEDD (normal rage 25–45%) (5). This measurement reflects EF only in case of homogeneous contraction of the LV (Figure 1).
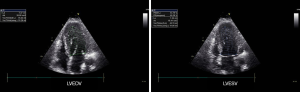
Using TEE or TTE systolic LV function can also be quantitatively assessed by fractional area change (FAC) as follow at the level of papillary muscles in a short axis view of the LV: FAC (%) = (LVEDA − LVSA) × 100/LVEDA with LVEDA end diastolic area and LVSA end systolic area of LV (normal value 36–64%) (7,8).
LV stroke volume (LVSV) and LV end-diastolic volume (LVEDV) may be assessed using Simpson method using either apical 4-chamber view alone or combining this view with apical 2-chamber view (Figure 2) and EF can be calculated as following EF = LVEDV − LVSV/LVEDV (normal value 55–75%) (7). Global systolic function can also be estimated visually especially when endocardial definition is insufficient for to Simpson method. With 2D echocardiography a reasonable correlation with measured quantitatively by echocardiography EF (Simpson) is demonstrated particularly when LVEF is visually estimated using intervals of 5% to 10% (9). Three dimensional (3D) reconstructions that use data from multiple tomographic images but do not seems accurate in ICU patients.
All these measurements need an adequate endocardial definition and accurate identification of the endocardial borders. Unfortunately, in the critical care setting, endocardial border definition may potentially be suboptimal because of technically limited TTE and poor imaging quality (1,10,11). Harmonic technique improved the visualisation of the endocardium and is widely used (12-14) and in difficult cases TEE can be useful (1,10,11).
EF depends on both preload and afterload. The EF may look normal in septic shock patients before starting noradrenalin infusion. Later the infusion of noradrenalin will increase LV afterload and may unmask a LV systolic dysfunction. Then afterload should be interpreted together with the LV afterload (15).
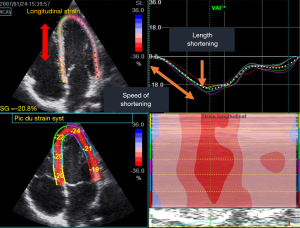
Longitudinal strain and speckle tracking
It was demonstrated that cardiac dysfunction starts with an impairment of longitudinal strain despite the EF remains normal for a long period of time. Then it became usual to assess longitudinal strain using the speckle tracking technique (Figure 3). This technique permits to follow the distance between two speckles during systole. The initial distance is called Lo and the final L and then strain is calculated as follow (L-Lo)/Lo. During the systole the normal value is negative −21.1±2.4% (16). This technique is not available on all echocargiograph. Only the most recent and performant echocargiograph will provide the possibility to measure online the strain and speckle tracking.
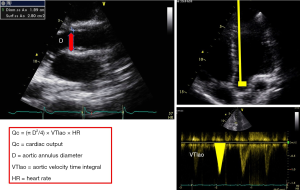
Cardiac output (Qc)
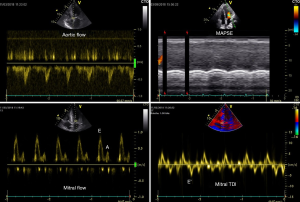
Qc is calculated as follow Qc = SV × HR where SV = CSAao × VTIao (SV is stroke volume, HR heart rate, CSAao left ventricular outflow tract (LVOT) cross sectional area, VTIao velocity time integral of LVOT) (Figure 4) (17). CSA is derived from the LVOT diameter measured from parasternal long axis view and VTIao measured on aortic blood flow recorded from apical 5-chambre view using pulsed Doppler. TTE and TEE approach could be used but small errors in diameter measurement become large errors in cross sectional area calculations because of the quadratic relationship between these variables [CSAao = (2 × 3.14 × LVOT2)/4]. Diameter and VTI measurements be made at the same anatomic site, with an average of 3 measurements. Because LVOT size do not change any change of SV could be tracked by VTIao change. pulmonary or aortic orifice, using TTE or TEE (17-19). This method was extensively validated against thermodilution in cardiologic field and in ICUs (17,20,21). Stroke volume may also be calculated as the difference of LV volume in diastole minus LV volume in systole (using the Simpson method) but this approach seems to be less accurate that previous one (22).
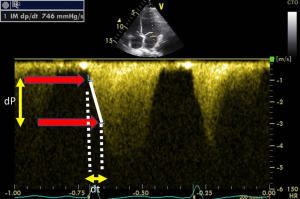
dP/dt on mitral regurgitation
We demonstrated that all volunteers, in whom we performed TTE, a small mitral regurgitation was present (23). Because mitral regurgitation velocity changes during systole is related to the change of intra ventricular pressure, dP/dt could be easily assessed this flow recorded using continuous wave Doppler (Figure 5). By measuring the duration time (dt) between the velocity of 1 m/s and the velocity of 3 m/s (dP of 32 mmHg) on the mitral regurgitation envelop it becomes easy to diagnose any LV systolic dysfunction (normal ranges 800–1,200. This approach was well validated (24,25).
Mitral annular plane systolic excursion (MAPSE) and longitudinal wall fractional shortening (LWFS)
Systolic LV function can also be assessed by MAPSE measurement (26-29). MAPSE should be measured using M-mode echocardiography with the M-mode cursor aligned parallel to the LV walls. It corresponds to mitral annular displacement distance towards the apex and a reduced MAPSE thereby reflects impairment of the longitudinal LV contraction. The normal value of MAPSE ranges between 12 and 15 mm. A value <8 mm is associated with LV EF dysfunction (<50%) with a 98% sensitivity and 82% specificity (26). It is important to keep in mind that the correlation between MAPSE and EF is accurate in case of normal or dilated LV and should be interpreted with caution in case of hypertrophic LV. Interestingly, MAPSE can be easily recorded even in patients with a poor acoustic window and for untrained echocardiographer. Bergenzaun et al. have recently described the value of MAPSE in ICU patients and showed that it reflects LV systolic and diastolic function and reduced MAPSE was independently associated with 28-day mortality (27). More recently, in a retrospective study, LWFS an M-mode index based on MAPSE, demonstrated a very good correlation with left ventricular longitudinal strain (LVLS) and therefore LV function, in intensive care patients. Interestingly, LWFS requires a simple M-mode measurement, available in all machines and reachable after minimal training. Its reproducibility and its accuracy make it a potential useful index in clinical use (28).
TDI
TDI is used to assess global systolic LV function. Sample volume is placed at the level of mitral annulus recording velocities during systole and diastole. Systolic myocardial velocity (Sm) is considered normal above 9 cm/s. Nagueh et al. reported that Sm had a good correlation with LV EF (30). Others demonstrated a good correlation with peak positive dP/dt (31).
Ventricular maximal elastance
The slope of the end-systolic pressure-volume relation, measured during progressively altered cardiac loading conditions, is still considered as the golden standard method for the assessment of LV contractility, independent of preload and afterload (32). This method could not be used easily at the bedside and should be considered only during clinical or experimental research.
Assessment of asynchrony (33-36)
Contraction asynchrony could be assessed using speckle tracking and could be useful in patients with cardiac dysfunction. This is not used in daily cardiac evaluation in ICU patients at the bedside. assessed during an echocardiographic examination with limited potential application.
Assessment of diastolic function and pulmonary arterial occlusive pressure (37-40)Other Section
- Assessment of systolic function and cardiac output
- Assessment of diastolic function and pulmonary arterial occlusive pressure (37-40)
- Clinical situations
- Conclusions
- Acknowledgments
- Footnote
- References
Diastolic function is hard to assess in ICU patients because all parameters used to assess diastolic function could be impaired by hemodynamical dysfunction independently to the diastolic dysfunction. Mitral flow recorded using pulsed Doppler with the measurement of early (E) and late (A) velocities and the E/A ratio, together with mitral annulus early diastolic velocity E’ and the E/E’ ratio, size of left atrium and maximal velocity of tricuspid regurgitation were proposed in an algorithm to assess diastolic function and LV filling pressure (37). This algorithm was never validated in ICU patients. Ratio of E’ to propagation velocity (Vp) recorded using M-mode colour was proposed to assess LV filling pressure but this parameter is hard to assess in ICU patients and is not used.
Clinical situationsOther Section
- Assessment of systolic function and cardiac output
- Assessment of diastolic function and pulmonary arterial occlusive pressure (37-40)
- Clinical situations
- Conclusions
- Acknowledgments
- Footnote
- References
LV function should be assessed in all patients with hemodynamic compromise as shock and respiratory failure.
Septic shock
In septic shock LV dysfunction was demonstrated to be presented as high as 65% of cases but is not associated with increased mortality (41). Despite this meta-analysis recent cluster analysis of 300 patients with septic shock has shown that the cluster including patients with LV systolic dysfunction had higher mortality (33%) than another cluster (42). This systolic dysfunction could occur very early during the septic shock as well as after 48 or 72 hours (43). This dysfunction associates decreased EF and low cardiac output. Usually LV filling pressures are normal and the size of the left ventricle is normal. Actually, few studies demonstrated that left ventricle could be slightly dilated (but remains in the normal ranges) and this is usually associated with better prognosis than patients in which LV size was normal or ever reduced. This dysfunction is transient and disappears after few days and systolic function return to normal (43). Dobutamin infusion is usually started when tissue hypoxemia is associated with LV systolic dysfunction and a positive effect seems to be associated with a better prognosis than no effect (44). Diastolic dysfunction could be associated with LV systolic dysfunction or could be present without systolic dysfunction (45). Diastolic dysfunction is associated with poor prognosis (45). LV strain is impaired in many patients with normal systolic function in septic shock patients and is as well associated with poor prognosis (46).
Cardiogenic shock
Echocardiography is the main tool to diagnose the cause and to manage patients with cardiogenic shock. LV function is highly useful as well as the evaluation of LV filling pressures (Figure 6). With clinical signs, echocardiography analyses the hemodynamic consequences of the administration of catecholamines (including vasoconstrictive and/or inotropic drugs) on LVEF and CO. Also, echocardiography will help to decide to start hemodynamic mechanical assistance (ECMO) and when to wean this mechanical assistance.
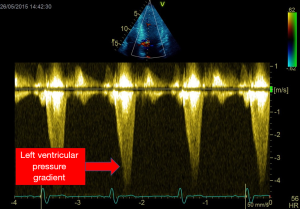
LV obstruction and shock
In 22% of patients with septic shock Chauvet et al. demonstrated LV obstruction (47). This obstruction was due mainly to hypovolemia and vasoplegia which induced a decreased size of LV and hyperkinesia which are the precipiting factors. This obstruction was reversed by either stopping Dobutamine infusion or correcting hypovolemia and sometime starting beta blockers (Figure 7) (47). This obstruction could occur when precipiting factors are or not associated with anatomic substratum as LV hypertrophy (48).
Pulmonary oedema and ARDS
Echocardiography seems to be the most useful tool in case of pulmonary oedema to distinguish cardiogenic pulmonary oedema and acute lung injury or ARDS. PAOP could be assessed as previously stated in this article and in case of pulmonary oedema echocardiography may diagnose the cause (49).
ConclusionsOther Section
- Assessment of systolic function and cardiac output
- Assessment of diastolic function and pulmonary arterial occlusive pressure (37-40)
- Clinical situations
- Conclusions
- Acknowledgments
- Footnote
- References
Echocardiography should be the first line used method in ICU patients with hemodynamic compromise. LV function together with RV function and fluid responsiveness permits to assess the pathophysiology of shock or respiratory failure, to diagnose the cause and to monitor the patient over the time.
AcknowledgmentsOther Section
- Assessment of systolic function and cardiac output
- Assessment of diastolic function and pulmonary arterial occlusive pressure (37-40)
- Clinical situations
- Conclusions
- Acknowledgments
- Footnote
- References
None.
FootnoteOther Section
- Assessment of systolic function and cardiac output
- Assessment of diastolic function and pulmonary arterial occlusive pressure (37-40)
- Clinical situations
- Conclusions
- Acknowledgments
- Footnote
- References
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ReferencesOther Section
- Assessment of systolic function and cardiac output
- Assessment of diastolic function and pulmonary arterial occlusive pressure (37-40)
- Clinical situations
- Conclusions
- Acknowledgments
- Footnote
- References
- Slama MA, Novara A, Van de Putte P, et al. Diagnostic and therapeutic implications of transesophageal echocardiography in medical ICU patients with unexplained shock, hypoxemia, or suspected endocarditis. Intensive Care Med 1996;22:916-22. [Crossref] [PubMed]
- Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU: part 1. Chest 2005;128:881-95. [Crossref] [PubMed]
- Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU: part 2. Chest 2005;128:1766-81. [Crossref] [PubMed]
- Hüttemann E, Schelenz C, Kara F, et al. The use and safety of transoesophageal echocardiography in the general ICU -- a minireview. Acta Anaesthesiol Scand 2004;48:827-36. [Crossref] [PubMed]
- Otto CM. Left and right ventricular systolic function. In: Otto CM textbook of clinical echocardiography. Pennsylvania: Elsevier Saunders Philadelphia, 2004:131-95.
- Poelaert JI, Schupfer G. Hemodynamic monitoring utilizing transesophageal echocardiography: the relationships among pressure, flow, and function. Chest 2005;127:379-90. [Crossref] [PubMed]
- Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989;2:358-67. [Crossref] [PubMed]
- Corsi C, Lang RM, Veronesi F, et al. Volumetric quantification of global and regional left ventricular function from real-time three-dimensional echocardiographic images. Circulation 2005;112:1161-70. [Crossref] [PubMed]
- McGowan JH, Cleland JG. Reliability of reporting left ventricular systolic function by echocardiography: a systematic review of 3 methods. Am Heart J 2003;146:388-97. [Crossref] [PubMed]
- Hwang JJ, Shyu KG, Chen JJ, et al. Usefulness of transesophageal echocardiography in the treatment of critically ill patients. Chest 1993;104:861-6. [Crossref] [PubMed]
- Vignon P, Mentec H, Terre S, et al. Diagnostic accuracy and therapeutic impact of transthoracic and transesophageal echocardiography in mechanically ventilated patients in the ICU. Chest 1994;106:1829-34. [Crossref] [PubMed]
- Cosyns B, El Haddad P, Lignian H, et al. Contrast harmonic imaging improves the evaluation of left ventricular function in ventilated patients: comparison with transesophageal echocardiography. Eur J Echocardiogr 2004;5:118-22. [Crossref] [PubMed]
- Kornbluth M, Liang DH, Brown P, et al. Contrast echocardiography is superior to tissue harmonics for assessment of left ventricular function in mechanically ventilated patients. Am Heart J 2000;140:291-6. [Crossref] [PubMed]
- Declerck C, Hillel Z, Shih H, et al. A comparison of left ventricular performance indices measured by transesophageal echocardiography with automated border detection. Anesthesiology 1998;89:341-9. [Crossref] [PubMed]
- Slama M, Maizel J. Echocardiographic measurement of ventricular function. Curr Opin Crit Care 2006;12:241-8. [Crossref] [PubMed]
- Menting ME, McGhie JS, Koopman LP, et al. Normal myocardial strain values using 2D speckle tracking echocardiography in healthy adults aged 20 to 72 years. Echocardiography 2016;33:1665-75. [Crossref] [PubMed]
- Mercado P, Maizel J, Beyls C, et al. Transthoracic echocardiography: an accurate and precise method for estimating cardiac output in the critically ill patient. Crit Care 2017;21:136-40. [Crossref] [PubMed]
- Tribouilloy C, Slama MA, Choquet D, et al. Determination of transmitral blood flow by pulsed echodoppler. Correlation with aortic blood flow in 30 patients. Arch Mal Coeur Vaiss 1991;84:957-65. [PubMed]
- Lewis JF, Kuo LC, Nelson JG, et al. Pulsed Doppler echocardiographic determination of stroke volume and cardiac output: clinical validation of two new methods using the apical window. Circulation 1984;70:425-31. [Crossref] [PubMed]
- Darmon PL, Hillel Z, Mogtader A, et al. Cardiac output by transesophageal echocardiography using continuous-wave Doppler across the aortic valve. Anesthesiology 1994;80:796-805. [Crossref] [PubMed]
- Estagnasié P, Djedaini K, Mier L, et al. Measurement of cardiac output by transesophageal echocardiography in mechanically ventilated patients. Comparison with thermodilution. Intensive Care Med 1997;23:753-9. [Crossref] [PubMed]
- Axler O, Megarbane B, Lentschener C, et al. Comparison of cardiac output measured with echocardiographic volumes and aortic Doppler methods during mechanical ventilation. Intensive Care Med 2003;29:208-17. [Crossref] [PubMed]
- Jobic Y, Slama M, Tribouilloy C. Et alDoppler echocardiographic evaluation of valve regurgitation in healthy volunteers. Br Heart J 1993;69:109-13. [Crossref] [PubMed]
- Bargiggia GS, Bertucci C, Recusani F, et al. A new method for estimating left ventricular dP/dt by continuous wave Doppler-echocardiography. Validation studies at cardiac catheterization. Circulation 1989;80:1287-92. [Crossref] [PubMed]
- Chen C, Rodriguez L, Guerrero JL, et al. Noninvasive estimation of the instantaneous first derivative of left ventricular pressure using continuous-wave Doppler echocardiography. Circulation 1991;83:2101-10. [Crossref] [PubMed]
- Hu K, Liu D, Herrmann S, Niemann M, et al. Clinical implication of mitral annular plane systolic excursion for patients with cardiovascular disease. Eur Heart J Cardiovasc Imaging 2013;14:205-12. [Crossref] [PubMed]
- Bergenzaun L, Ohlin H, Gudmundsson P, et al. Mitral annular plane systolic excursion (MAPSE) in shock: a valuable echocardiographic parameter in intensive care patients. Cardiovasc Ultrasound 2013;11:16. [Crossref] [PubMed]
- Huang SJ, Ting I, Huang AM, et al. Longitudinal wall fractional shortening: an M-mode index based on mitral annular plane systolic excursion (MAPSE) that correlates and predicts left ventricular longitudinal strain (LVLS) in intensive care patients. Crit Care 2017;21:292. [Crossref] [PubMed]
- Støylen A, Mølmen HE, Dalen H. Relation between Mitral Annular Plane Systolic Excursion and Global longitudinal strain in normal subjects: The HUNT study. Echocardiography 2018;35:603-10. [Crossref] [PubMed]
- Nagueh SF, Middleton KJ, Kopelen HA, et al. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 1997;30:1527-33. [Crossref] [PubMed]
- Mishiro Y, Oki T, Yamada H, et al. Evaluation of left ventricular contraction abnormalities in patients with dilated cardiomyopathy with the use of pulsed tissue Doppler imaging. J Am Soc Echocardiogr 1999;12:913-20. [Crossref] [PubMed]
- Suga H, Sagawa K. Instantaneous pressure-volume relationships and their ratio in the excised, supported canine left ventricle. Circ Res 1974;35:117-26. [Crossref] [PubMed]
- Pinsky MR. Quantifying left ventricular ejection effectiveness. In Vincent JL 2003 Year Book of intensive care and emergency medicine. Berlin: Springler-Verlag, 2003:436-46.
- Gorcsan J 3rd, Strum DP, Mandarino WA, et al. Quantitative assessment of alterations in regional left ventricular contractility with color-coded tissue Doppler echocardiography. Comparison with sonomicrometry and pressure-volume relations. Circulation 1997;95:2423-33. [Crossref] [PubMed]
- Mor-Avi V, Vignon P, Koch R, et al. Segmental analysis of color kinesis images: new method for quantification of the magnitude and timing of endocardial motion during left ventricular systole and diastole. Circulation 1997;95:2082-97. [Crossref] [PubMed]
- Kapetanakis S, Kearney MT. Siva Aet al. Real-time three-dimensional echocardiography: a novel technique to quantify global left ventricular mechanical dyssynchrony. Circulation 2005;112:992-1000. [Crossref] [PubMed]
- Slama M, Susic D, Varagic J, et al. Diastolic dysfunction in hypertension. Curr Opin Cardiol 2002;17:368-73. [Crossref] [PubMed]
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2016;17:1321-60. [Crossref] [PubMed]
- Combes A, Arnoult F, Trouillet JL. Tissue Doppler imaging estimation of pulmonary artery occlusion pressure in ICU patients. Intensive Care Med 2004;30:75-81. [Crossref] [PubMed]
- Bouhemad B, Nicolas-Robin A, Benois A, et al. Echocardiographic Doppler assessment of pulmonary capillary wedge pressure in surgical patients with postoperative circulatory shock and acute lung injury. Anesthesiology 2003;98:1091-100. [Crossref] [PubMed]
- Huang SJ, Nalos M, McLean AS. Is early ventricular dysfunction or dilatation associated with lower mortality rate in adult severe sepsis and septic shock? A meta-analysis. Crit Care 2013;17:R96-100. [Crossref] [PubMed]
- Geri G, Vignon P, Aubry A, et al. Cardiovascular clusters in septic shock combining clinical and echocardiographic parameters: a post hoc analysis. Intensive Care Med 2019;45:657-67. [Crossref] [PubMed]
- Vieillard Baron A, Schmitt JM, Beauchet A, et al. Early preload adaptation in septic shock? A transesophageal echocardiographic study. Anesthesiology 2001;94:400-6. [Crossref] [PubMed]
- Kumar A, Schupp E, Bunnell E, et al. Cardiovascular response to dobutamine stress predicts outcome in severe sepsis and septic shock. Crit Care 2008;12:R35-40. [Crossref] [PubMed]
- Sanfilippo F, Corredor C, Arcadipane A, et al. Tissue Doppler assessment of diastolic function and relationship with mortality in critically ill septic patients: a systematic review and meta-analysis. Br J Anaesth 2017;119:583-94. [Crossref] [PubMed]
- Boissier F, Razazi K, Seemann A, et al. Left ventricular systolic dysfunction during septic shock: the role of loading conditions. Intensive Care Med 2017;43:633-42. [Crossref] [PubMed]
- Chauvet JL, El-Dash S, Delastre O, et al. Early dynamic left intraventricular obstruction is associated with hypovolemia and high mortality in septic shock patients. Crit Care 2015;19:262-6. [Crossref] [PubMed]
- Slama M, Tribouilloy C, Maizel J. Left ventricular outflow tract obstruction in ICU patients. Curr Opin Crit Care 2016;22:260-6. [Crossref] [PubMed]
- Feissel M, Maizel J, Robles G, et al. Clinical relevance of echocardiography in acute severe dyspnea. J Am Soc Echocardiogr 2009;22:1159-64. [Crossref] [PubMed]
Cite this article as: Zerbib Y, Maizel J, Slama M. Echocardiographic assessment of left ventricular function. J Emerg Crit Care Med 2019;3:33.