
Inter-hospital variations in resuscitation processes and outcomes of out-of-hospital cardiac arrests in Singapore
Introduction
Out-of-hospital cardiac arrests (OHCAs) are a global health concern and remain a leading cause of death (1). Various demographic, etiological and pre-hospital factors are well known to affect outcomes. Examples include age (2), cause of arrest (3), witnessed arrest (2-6), bystander cardiopulmonary resuscitation (CPR) (3-6), and first arrest rhythm (2-5,7). Recent studies comparing inter-hospital OHCA outcomes have also highlighted several hospital-based factors—percutaneous coronary intervention (PCI) capability [whether specified as 24-hour emergency PCI (6,8) or otherwise] (9), OHCA patient volume (10), and expertise and ability (9). Several other factors have also been associated with inter-regional variations in OHCA survival (11,12). These include regional differences in OHCA risk, population density, socioeconomic and racial characteristics, bystander response, emergency cardiac care and importantly, post-resuscitation care (6,13,14) Developments in post-resuscitation care, including targeted temperature management (TTM) (15-17) and early PCI (18,19), are also key elements behind recent improvements in OHCA survival in the early 2000s (1,16,20), compared to the lack of significant survival improvement several decades earlier (5,21,22).
However, although there are specific post-resuscitation guidelines from the American Heart Association (23) and European Resuscitation Council (24), and local accreditation bodies such as the National Resuscitation Council in Singapore (25), these interventions require multidisciplinary dedicated care, specialized expertise and equipment, and involve substantial healthcare costs (26). Indeed, physician surveys in the United States demonstrate low uptake rates due to a variety of reasons, including the aforementioned (27,28). Furthermore, local adoption of PCI and TTM practices has only recently occurred in 2008 (16). We postulate that these may also cause significant utilization disparities amongst hospitals within the same country, which may in turn result in dissimilarities in OHCA outcomes.
To our knowledge, a comparison of inter-hospital OHCA outcomes within Singapore has never been done. This could reveal variation in the delivery of resuscitative and post-resuscitative care, and highlight opportunities for improvement. In this study, we sought to determine the magnitude and factors associated with inter-hospital outcome variations for OHCAs in all public hospitals in Singapore.
Methods
Study design
This was a prospective, nation-wide, multi-centre cohort study of consecutive OHCA cases presenting at any of the 6 restructured hospitals in Singapore from April 2010 to December 2014. OHCA was determined by these criteria: absence of pulse, unresponsiveness, and apnea (29), regardless of aetiology and method of arrival. We excluded patients who are immediately pronounced dead and for whom resuscitation is not attempted.
In this study, all Singapore OHCA cases were extracted from the Pan-Asian Resuscitation Outcomes Study Clinical Research Network (PAROS CRN), an international prospective registry of OHCAs in the Asia-Pacific region. Relevant data collection processes for Singapore were reviewed and approved by Singhealth Centralised Institutional Review Boards (IRB) and National Healthcare Group Domain Specific Review Boards (DSRB) with waiver of informed consent. A data sharing agreement within PAROS CRN has also been put in place to protect the confidentiality of the study population. The primary outcome was survival to discharge or 30 days post-arrest, if not discharged. Secondary outcomes included survival to Emergency Department (ED) admission and survival with favourable neurological outcome, defined as a Glasgow-Pittsburgh Cerebral Performance Categories (CPC) ≤2 at hospital discharge, or 30 days post OHCA if not discharged. CPC are classified as follows: (I) good cerebral performance where patient is conscious and able to work and lead a normal life; (II) moderate cerebral disability where patient is conscious and able to work part-time in sheltered environments; (III) severe cerebral disability where patient is conscious but dependent on others for daily support; (IV) coma; (V) death by traditional criteria or certified brain dead. CPC grading was done through in-person assessments, clinical records, and via the telephone by trained personnel not directly involved in subject care or in this study.
Setting
Singapore is a highly urbanized city-state in Southeast Asia comprising of one main island along with 63 other islets, with a population of 5.6 million, a population density of 7,797 per square kilometre, and a median age of 40.0 years (30). In the late 20th century, Singapore’s public governmental hospitals were restructured while remaining as not-for-profit institutions wholly-owned by the government so as to improve management autonomy and flexibility. As of start of OHCA data collection in 2010, there were six adult acute restructured hospitals in Singapore (randomly labelled Hospitals A-F and in no particular order), equipped with 6,686 (82.9%) beds which accommodated 343,332 (78.5%) admissions in that year (31). Five of the 6 hospitals (B-F) provide 24-hour emergency PCI services. There were also seven private hospitals in Singapore equipped with 1,378 beds (32), however they do not receive OHCA cases from emergency medical services (EMS) and do not manage post-OHCA patients. There is also a paediatric restructured hospital, KK Women’s and Children’s Hospital, which does not manage adult OHCA patients, and only received 30 OHCAs during the study period. Hospital teaching status was defined as the presence of an adjacent affiliated medical school.
Prehospital EMS is provided by the Singapore Civil Defence Force (SCDF), a uniformed government agency responsible also for fire-fighting, disaster relief, and search and rescue. To do so, it operates a publicly funded fire-based system with a centralized phone dispatch system, and has under its purview 46 ambulances and 15 fast response paramedics (FRP) on first-aid equipped motorcycles (33). Paramedics are trained in basic life support, 12-lead electrocardiography (ECG), automated external defibrillator usage, and adrenaline administration (34). SCDF uses a catchment zone policy where patients from defined geographic areas will be conveyed to the public hospital nearest to the incident location, regardless of prehospital symptoms or diagnosis. Therefore, no significant “Hawthorne effect” noted on behalf of the EMS personnel. Average response time is <8 minutes (16). There are also several private ambulance companies in Singapore but they do not respond to 995 dispatch or OHCA and are largely utilized for elective inter-facility transfers.
Analysis
The effects of hospital-based resuscitative interventions and admitting hospital on outcome were compared using Chi-squared tests and multivariate logistic regression models respectively, using IBM SPSS Statistics 21 (IBM Corporation, Armonk, NY, USA). Hospitals were benchmarked against Hospital F, the oldest and largest restructured hospital in Singapore. The parameters eventually selected for the multivariate logistic regression models are known to current literature, and were first investigated using univariate logistic regression. These include age, gender, cause of arrest (cardiac/respiratory/traumatic/others), witnessed arrest, bystander CPR, and first arrest rhythm [asystole/pulseless electrical activity (PEA)/ventricular tachycardia (VT)/ventricular fibrillation (VF)/other]. We subsequently attempted to explain any dissimilarities in outcomes via Chi-squared tests on inter-hospital factors both proven in literature: PCI capability and OHCA patient volume, and otherwise: years in operation, teaching status, and bed number. In an attempt to explain variations in OHCA outcomes, five inter-hospital factors were analysed: PCI capability, years in operation, teaching status, bed number, and OHCA patient volume.
Results
Demographics of study cohort
Out of a total of 7,609 patients, 4,952 (65.1%) were male, and had ages ranging from 19 to 115, with a median age of 66 years. In terms of cause of arrest, the most common was cardiac, followed by respiratory and traumatic with frequencies of 5,384 (70.8%), 481 (6.3%), and 224 (2.9%) respectively. The most common first arrest rhythm was asystole, followed by PEA, VF, and then VT, with frequencies of 3,873 (50.9%), 2,100 (27.6%), 1,248 (16.4%), and 34 (0.4%) respectively. In terms of pre-hospital management, 4,466 (58.7%) were witnessed arrests, and 2,732 (35.9%) received bystander CPR (Table 1).
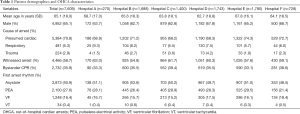
Full table
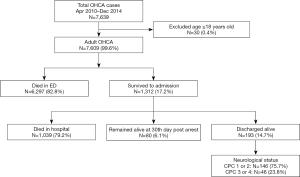
OHCA outcomes
Out of the 7,609 cases analysed, 1,312 (17.2%) survived to admission from the ED, out of which 268 (20.4%) underwent PCI, and 220 (16.8%) underwent TTM. Subsequently, 193 (14.7%) were discharged alive, and an additional 80 (6.1%) remained alive at 30 days. Out of the 193 patients who were discharged alive, 146 (75.7%) retained good cognitive function with CPC ≤2, while the remaining 46 (23.8%) had a CPC >2, and 1 (0.5%) had missing CPC data (Figure 1).
Inter-hospital comparison of OHCA outcomes
Survival to discharge or 30 days post-arrest, our primary outcome, varied across hospitals from 2.6% to 6.2% (rate difference, 3.6%; 95% CI: 1.7–5.5%). On univariate logistic regression, the following variables were associated with improved OHCA outcomes: witnessed arrest [odds ratio (OR) 3.7, 95% CI: 2.7–5.1, P<0.001], bystander CPR (OR 1.5, 95% CI: 1.1–1.9, P=0.002) and cardiac or respiratory cause of arrest (OR 2.1, 95% CI: 1.4–3.0, P<0.001; OR 1.9, 95% CI: 1.0–3.4, P=0.04) as opposed to traumatic and other causes (e.g., drowning). Older age (OR 0.98, 95% CI: 0.98–0.99, P<0.001), female gender (OR 0.65, 95% CI: 0.52–0.80, P=0.002) and non-VT first arrest rhythm, i.e., VF, asystole, PEA, other perfusing rhythm (OR 0.51, 95% CI: 0.23–1.1, P=0.098; OR 0.09, 95% CI: 0.03–0.025, P<0.001; OR 0.091, 95% CI: 0.39–0.21, P<0.001; OR 0.29, 95% CI: 0.12–0.70, P=0.006) were predictors of worse outcome.
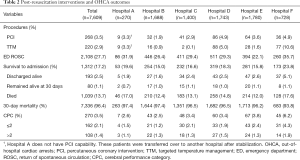
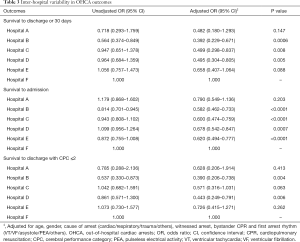
After subsequent multivariate analysis to eliminate known confounders, it was noted that as compared to Hospital F the study benchmark, Hospitals B, C, and D had a lower survival to discharge or 30 days post-arrest [adjusted odds ratio (AOR) 0.392, 95% CI: 0.229–0.671, P=0.0006; AOR 0.499, 95% CI: 0.298–0.837, P=0.008; AOR 0.495, 95% CI: 0.304–0.805, P=0.005]. Survival to ED admission also varied from 15.0% to 23.8% (rate difference, 8.8%; 95% CI: 5.3–12.3%), with Hospitals B, C, D, and E experiencing lower survival to ED admission (AOR 0.582, 95% CI: 0.462–0.733, P<0.0001; AOR 0.600, 95% CI: 0.474–0.759, P<0.0001; AOR 0.678, 95% CI: 0.542–0.847, P=0.0007; AOR 0.620, 95% CI: 0.494–0.777, P<0.0001). Lastly, survival to discharge with CPC ≤2 varied from 1.2% to 4.3% (rate difference, 3.1%; 95% CI: 1.5–4.7%), with Hospital B and D experiencing lower survival to discharge with good cognitive function (AOR 0.390, 95% CI: 0.206–0.738, P=0.004; AOR 0.443, 95% CI: 0.249–0.791, P=0.006) (Tables 2,3).
Full table
Full table
Hospital and post-resuscitation factors
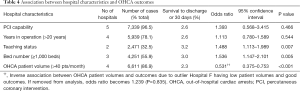
Comparisons of OHCAs presenting to hospitals with 24-hour emergency PCI capabilities and those without did not yield any significant correlation with primary outcome (OR 1.393, P>0.05). There was also no correlation between years in operation (≤20 vs. >20 years) and outcome (OR 1.113, P>0.05). Both teaching status and bed number (≥1,000 beds) are associated with improved survival to discharge or 30 days (OR 1.488, P=0.007; OR 1.536, P=0.005). Lastly, in terms of OHCA patient volume, Hospitals B, C, D and E had high patient volumes of at least 40 patients/month, while Hospitals F and A have half that or less, with 10–20 patients/month. Hospital A in particular, had the lowest patient volume, with an average of approximately 4 patients/month. Interestingly, high OHCA patient volume hospitals tended to have poorer OHCA outcomes (OR 0.531, P<0.001) (Table 4).
Full table
PCI and TTM usage were both correlated with improved survival to discharge or 30 days post-arrest if not discharged (AOR 16.2, 95% CI: 11.6–22.6, P<0.01; AOR 7.96, 95% CI: 5.44–11.70, P<0.001) and survival to discharge or 30 days post arrest if not discharged with CPC ≤2 (AOR 16.9, 95% CI: 11.2–25.5, P<0.001; AOR 5.4, 95% CI: 3.3–8.9, P<0.001). The utilization of PCI and TTM was also noted to vary significantly across hospitals (AOR 0.047, P<0.001; AOR 0.099, P<0.001), ranging from 1.9% to 4.9% (rate difference, 3.0%; 95% CI: 1.3–4.7%) and 0.1% to 10.6% (rate difference, 10.5%; 95% CI: 8.3–12.7%) respectively.
Discussion
Contrary to previous studies (6,8-10), we also report a significant correlation between both teaching status and bed number, and survival to discharge or 30 days. This is only but expected, and underscores the importance of academia and economies of scale. Furthermore, as opposed to current findings in literature (10), there is an inverse correlation between OHCA patient volumes and outcomes. This is likely because Hospital F which has the second lowest OHCA patient load (n=728) also has the best outcomes (6.2%). We postulate that this is because this hospital possesses the aforementioned factors—an adjacent affiliated medical school and a high bed number.
The primary outcome, survival to discharge or 30 days post-arrest varied from 2.6% to 6.2% (rate difference, 3.6%; 95% CI: 1.7–5.5%), similar to Hasegawa’s 3.7% to 6.1% (rate difference 2.4%; 95% CI: 2.1–2.7%) (12) and Kajino’s 5.4% to 11.6% (rate difference 6.2%; 95% CI: 4.9–7.5%) (13). Survival to discharge with good cognitive function (CPC) ≤2 was also comparable to similar studies (12,14). However, it must be stated that these are not perfect comparisons due to significant variations in EMS practices (29,34,35) and intrinsic study differences in terms of patient selection and data grouping.
This analysis of consecutive OHCAs over a 4.5-year period has strengthened current observational evidence in literature (6,8,9), demonstrating dissimilarities in OHCA interventions and outcomes between hospitals. Compared to findings of previous studies (18), we did not find any significant correlation between hospital PCI capability and outcome. One must note, however, that only one hospital does not have 24-hour emergency PCI capabilities and it still sends eligible cases to the nearest facility for post-resuscitative interventions. Although timings are not known to us, this particular hospital is located <5 km (3.1 miles) away from the nearest 24-hour emergency PCI facility.
While practice makes perfect, in this situation other factors appear to play a larger role in affecting outcomes. We were unable to assess the third hospital factor highlighted in other inter-hospital OHCA studies, i.e., governmental certification of expertise and ability as no such system currently exists in Singapore. Further studies are indicated to further delineate the relationship between hospital factors and OHCA outcomes.
This study has implications on the current consideration for establishing regional systems of care for OHCA in Singapore. At the present moment, the SCDF uses a “catchment zone” policy where patients are transported to the nearest restructured hospital based on policy-directed predefined geographic locations. However, studies published in the last decade seem to show otherwise—that distance is not associated with survival outcomes (6,13). However, although we did not analyse transport distance in this study, we have shown that the utilization of post-resuscitative interventions is strongly associated with better OHCA outcomes, and that certain hospitals have higher utilization rates than others. It may therefore indeed be prudent to designate such hospitals as specialized cardiac arrest centres, superseding transport to nearest hospital (7,36). Prior to this, however, further analysis on the factors behind variations in the utilization of post-resuscitation intervention should be carried out. Furthermore, although Singapore is small, it is not clear if there exists a distance cut-off from which distance becomes more significant a factor over admitting hospital on outcomes. Thus, a prospective study could be carried out to ascertain the relationship between distance to nearest hospital, distance to nearest specialized cardiac arrest centre, and outcomes so as to create an evidence-based tool to guide EMS providers on optimal transport destination from any given location.
Limitations
Our study findings should be interpreted with the following limitations in mind. First, as this was a multi-centre study spanning several years, data integrity, validity, and transcription errors are potential limitations. This was minimized through the standardization of definitions, data collection protocols such as the utilization of case record forms, and large sample sizes. Next, as this is an observational study, confounders are likely to be present, especially sociodemographic and economic factors. There may be diversity of our study population coupled with the geographically determined hospital-patient watershed. CPR quality data in the pre-hospital and ED setting was also not collected. Although such data is not privy to us, we have made rigorous adjustments for multiple patient and pre-hospital factors known to literature, including age, gender, cause of arrest, witnessed arrest, bystander CPR, and first arrest rhythm. Furthermore, the EMS system is generally uniform across the city, and training for both EMS and ED personnel is centralized. Thus, differences in CPR quality, if any, is unlikely to account for our study results. Additional analyses on the factors behind variations in the utilization of post-resuscitation interventions and dissimilarities in inter-hospital OHCA outcomes should be carried out.
Lastly, as our study population possesses specific patient demographics, clinical guidelines, and prehospital and medical infrastructure (36), the findings from this study may not be fully generalizable to other populations. However, as our practices largely follow that of latest evidence-based guidelines and consensus from international bodies such as the American Heart Association and the International Liaison Committee on Resuscitation (26), our findings are likely to be generalizable to most developed countries. Despite the aforementioned limitations, our study provides new insights and supports recent findings regarding factors affecting OHCA outcomes.
In summary, OHCA outcomes and the use of post-resuscitative interventions vary between hospitals in Singapore. Hospital teaching status, bed number, and OHCA patient volumes affect patient outcomes. The variation in survival outcomes indicate that there is potential for further optimization and standardization of hospital resuscitation and post-resuscitation practices. Further research into the relevant factors is indicated.
Acknowledgements
In fond memory of our dearest friend and colleague, Ms Susan Yap.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Relevant data collection processes for Singapore were reviewed and approved by Singhealth Centralised Institutional Review Boards (IRB) (CIRB ref no: 2010/270/C and 2013/604/C) and National Healthcare Group Domain Specific Review Boards (DSRB) (DSRB ref no: 2010/00545 and 2013/00929) with waiver of informed consent.
References
- Daya MR, Schmicker RH, Zive DM, et al. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation 2015;91:108-15. [Crossref] [PubMed]
- Ahn S, Lee BK, Youn CS, et al. Predictors of good neurologic outcome after resuscitation beyond 30 min in out-of-hospital cardiac arrest patients undergoing therapeutic hypothermia. Intern Emerg Med 2018;13:413-9. [PubMed]
- Chia MYC, Lu QS, Rahman NH, et al. Characteristics and outcomes of young adults who suffered an out-of-hospital cardiac arrest (OHCA). Resuscitation 2017;111:34-40. [Crossref] [PubMed]
- Spaite DW, Stiell IG, Bobrow BJ, et al. Effect of transport interval on out-of-hospital cardiac arrest survival in the OPALS study: Implications for triaging patients to specialized cardiac arrest centers. Ann Emerg Med 2009;54:248-55. [Crossref] [PubMed]
- Sasson C, Rogers MAM, Dahl J, et al. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:63-81. [Crossref] [PubMed]
- Tranberg T, Lippert FK, Christensen EF, et al. Distance to invasive heart centre, performance of acute coronary angiography, and angioplasty and associated outcome in out-of-hospital cardiac arrest: a nationwide study. Eur Heart J 2017;38:1645-52. [Crossref] [PubMed]
- Davis DP, Fisher R, Aguilar S, et al. The feasibility of a regional cardiac arrest receiving system. Resuscitation 2007;74:44-51. [Crossref] [PubMed]
- Stub D, Smith K, Bray JE, et al. Hospital characteristics are associated with patient outcomes following out-of-hospital cardiac arrest. Heart 2011;97:1489-94. [Crossref] [PubMed]
- Wnent J, Seewald S, Heringlake M, et al. Choice of hospital after out-of-hospital cardiac arrest – a decision with far-reaching consequences: a study in a large German city. Crit Care 2012;16:R164. [Crossref] [PubMed]
- Carr BG, Kahn J M, Merchant RM, et al. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation 2009;80:30-4. [Crossref] [PubMed]
- Girotra S, Diepen S, Brahmajee KN, et al. Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation 2016;133:2159-68. [Crossref] [PubMed]
- Hasegawa K, Tsugawa Y, Camargo CA, et al. Regional variability in survival outcomes of out-of-hospital cardiac arrest: The All-Japan Utstein Registry. Resuscitation 2013;84:1099-107. [Crossref] [PubMed]
- Kajino K, Iwami T, Daya M, et al. Impact of transport to critical care medical centers on outcomes after out-of-hospital cardiac arrest. Resuscitation 2010;81:549-54. [Crossref] [PubMed]
- Engdahl J, Abrahamsson P, Bång A, et al. Is hospital care of major importance for outcome after out-of-hospital cardiac arrest? Experience acquired from patients with out-of-hospital cardiac arrest resuscitated by the same Emergency Medical Service and admitted to one of two hospitals over a 16-year period in the municipality of Göteborg. Resuscitation 2000;43:201-11. [Crossref] [PubMed]
- Choi SW, Shin SD, Ro YS, et al. Effect of therapeutic hypothermia on the outcomes after out-of-hospital cardiac arrest according to initial ECG rhythm and witnessed status: A nationwide observational interaction analysis. Resuscitation 2016;100:51-9. [Crossref] [PubMed]
- Lai H, Choong CV, Fook-Chong S, et al. Interventional strategies associated with improvements in survival for out-of-hospital cardiac arrests in Singapore over 10 years. Resuscitation 2015;89:155-61. [Crossref] [PubMed]
- Nolan JP, Morley PT, Hoek TLV, et al. Therapeutic hypothermia after cardiac arrest. An advisory statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation. Resuscitation 2003;57:231-5. [Crossref] [PubMed]
- Spaulding CM, Joly LM, Rosenberg A, et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med 1997;336:1629-33. [Crossref] [PubMed]
- Dalby M, Bouzamondo A, Lechat P, et al. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction: A meta-analysis. Circulation 2003;108:1809-14. [Crossref] [PubMed]
- Okubo M, Kiyohara K, Iwami T, et al. Nationwide and regional trends in survival from out-of-hospital cardiac arrest in Japan: A 10-year cohort study from 2005 to 2014. Resuscitation 2017;115:120-8. [Crossref] [PubMed]
- Rea TD, Eisenberg MS, Becker LJ, et al. Temporal trends in sudden cardiac arrest: A 25-year emergency medical services perspective. Circulation 2003;107:2780-5. [Crossref] [PubMed]
- Herlitz J, Bång A, Gunnarsson J, et al. Factors associated with survival to hospital discharge among patients hospitalised alive after out of hospital cardiac arrest: change in outcome over 20 years in the community of Göteborg, Sweden. Heart 2003;89:25-30. [Crossref] [PubMed]
- American Heart Association. Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: Post-cardiac arrest care. Dallas, Texas, American Heart Association, 2015. (Accessed 5 May 2017). Available online: https://eccguidelines.heart.org/wp-content/themes/eccstaging/dompdf-master/pdffiles/part-8-post-cardiac-arrest-care.pdf
- Nolan JP, Soar J, Cariou A, et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines for Post-Resuscitation Care 2015 Section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation 2015;95:202-22. [Crossref] [PubMed]
- Anantharaman V. The post-resuscitation bundle. Singapore Med J 2011;52:607-10. [PubMed]
- Pang PYK, Wee GHL, Huang MJ, et al. Therapeutic hypothermia may improve neurological outcomes in extracorporeal life support for adult cardiac arrest. Heart Lung Circ 2017;26:817-24. [Crossref] [PubMed]
- Merchant RM, Soar J, Skrifvars MB, et al. Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest. Crit Care Med 2006;34:1935-40. [Crossref] [PubMed]
- Abella BS, Rhee JW, Huang KN, et al. Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey. Resuscitation 2005;64:181-6. [Crossref] [PubMed]
- Ong ME, Shin SD, De Souza NN, et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015;96:100-8. Erratum in: Resuscitation 2016;98:125-6. [Crossref] [PubMed]
- Singapore Department of Statistics. Latest data. Available online: (accessed 2 June 2017)https://www.singstat.gov.sg/find-data/search-by-theme/population/population-and-population-structure/latest-data
- Ministry of Health, Singapore. Hospital admissions by sector, gender and age group. Available online: (accessed 10 June 2017)https://www.moh.gov.sg/resources-statistics/singapore-health-facts/admissions-and-outpatient-attendances
- Ministry of Health, Singapore. Number of acute hospitals and specialty centres. Available online: (accessed 10 June 2017)https://www.moh.gov.sg/resources-statistics/singapore-health-facts/beds-in-inpatient-facilities-and-places-in-non-residential-long-term-care-facilities
- Ho AFW, Loy EY, Pek PP, et al. Emergency medical services utilization among patients with ST-segment Elevation Myocardial Infarction: Observations from the Singapore Myocardial Infarction Registry. Prehosp Emerg Care 2016;20:454-61. [Crossref] [PubMed]
- Shin SD, Ong ME, Tanaka H, et al. Comparison of emergency medical services systems across Pan-Asian countries: a Web-based survey. Prehosp Emerg Care 2012;16:477-96. [Crossref] [PubMed]
- Ong ME, Cho J, Ma MH, et al. Comparison of emergency medical services systems in the pan-Asian resuscitation outcomes study countries: Report from a literature review and survey. Emerg Med Australas 2013;25:55-63. [Crossref] [PubMed]
- Geri G, Gilgan J, Wu W, et al. Does transport time of out-of-hospital cardiac arrest patients matter? A systematic review and meta-analysis. Resuscitation 2017;115:96-101. [Crossref] [PubMed]
Cite this article as: Tan TX, Hao Y, Ho AF, Shahidah N, Yap S, Ng YY, Doctor N, Leong BS, Gan HN, Mao DR, Chia MY, Cheah SO, Ong ME. Inter-hospital variations in resuscitation processes and outcomes of out-of-hospital cardiac arrests in Singapore. J Emerg Crit Care Med 2019;3:21.


