Survival after out of hospital cardiac arrest with prolonged period of resuscitation (250 minutes)
Introduction
In the United Kingdom it is estimated that only 8% of patients who suffer out of hospital cardiac arrest (OHCA) will survive to leave hospital (1). This case report discusses a patient’s excellent recovery, following prolonged resuscitation and highlights factors that may affect a favourable outcome, as well as the potential role of percutaneous coronary intervention (PCI) in OHCA.
Case presentation
This case presents a 68-year-old gentleman with a background of significant alcohol consumption, who smoked up to 60 cigarettes per day and had a previous transient ischaemic attack (TIA). He was otherwise living independently at home with his partner. He had a witnessed collapse whilst at home, following an episode of chest pain. His wife was unable to elicit any response and hence called for an ambulance.
Paramedics reportedly arrived on scene and were with the patient within four minutes of the call. Cardiopulmonary resuscitation (CPR) was initiated by the paramedics with an initial rhythm of ventricular fibrillation (VF). Using a LUCAS device, they delivered a total of nine 360J shocks, with three doses of (1 mg 1:10,000 IV) adrenaline, as well as a single dose of (300 mg IV) amiodarone, with rhythms varying between VF, and pulseless electrical activity (PEA) with intermittent short periods (longest period less than 30 minutes on route) of return of spontaneous circulation (ROSC). His ECG at this point demonstrated a right bundle branch block (RBBB) pattern, a copy of which was sent to the local PCI suite en route to hospital. As there were no ST elevation changes on the ECG the decision was to attend the Emergency department first for assessment/stabilisation.
On arrival at the Emergency Department (60 minutes post collapse), patient initially had ROSC (admission ABG: pH 7.094, pO2 8.89, pCO2 7.3, lactate 9.1, HCO3 16.0, BE −12.1, SO2 82.1). The airway was maintained with a supraglottic airway and LUCAS device remained in situ. His pupils were size 3, equal and reactive.
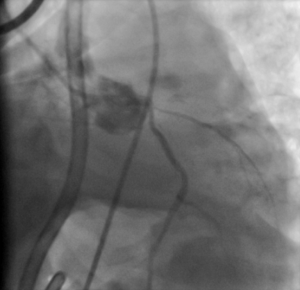
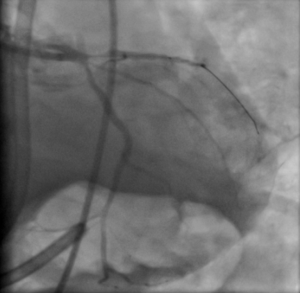
Within 1 minute of arrival, he had a further loss of output with PEA. CPR was commenced using LUCAS device with appropriate pharmacological intervention (boluses of 100 mcg of adrenaline, 300 mg amiodarone, before an adrenaline infusion 200 mcg/mL commenced at 8 mL/min). A bedside ECHO demonstrated globally impaired function with poor LV contractility. He was intubated and ventilated (with ketamine and suxemethonium), before being transferred for primary PCI (PPCI) with the LUCAS ongoing. Patient arrived for PPCI (3 hours post original collapse) and was found to have an occluded ostial left anterior descending (LAD) coronary artery (Figure 1). A cardiac stent was inserted (Figure 2) with good reperfusion (3.45 hours post cardiac arrest). An intra-aortic balloon pump was then inserted. The LUCAS device was stopped after 4 hours 10 min of resuscitation as patient had ROSC with adequate blood pressure.
He was transferred to the intensive care unit, where therapeutic hypothermia (TH) was initiated for 12 hours at 32–34 °C, before slow rewarming. Post resuscitation chest X-ray demonstrated dense consolidation throughout the right lung, suggestive of a possible collection or haemothorax. He was commenced on IV antibiotics for pneumonia (likely aspiration), which was later escalated to IV Tazocin. A subsequent CT thorax demonstrated sternal fractures and bilateral anterior rib fractures with right sided haemothorax, requiring a CT guided chest drain with 1.5 L drained. Given significant chest injury with slow respiratory wean, Cardio-Thoracic surgical team were consulted however no intervention deemed necessary. A CT scan of his head demonstrated some mild loss of grey/white differentiation, but no significant cerebral oedema and no other acute changes.
On day 9 of admission he underwent tracheostomy due to slow respiratory wean, confounded by significant chest wall injury secondary to chest compressions. He was successfully de-cannulated on day 18 of admission and stepped down to the cardiology ward after 21 days on ICU for further management. On discharge he was compos mentis and managing to mobilise short distances (albeit with some assistance).
Discussion
This case appears to be somewhat unique, describing a favourable outcome following a period of resuscitation this prolonged (>4 hours) following OHCA. According the Resuscitation Council (UK), around 28,000 people have attempted resuscitation following OHCA each year, of which approximately only 8% survive to leave hospital (1).
Following successful resuscitation, anoxic neurologic injury still remains a significant cause of morbidity and mortality (2). Anoxic brain injury remains a significant burden for patients who survive cardiac arrest, with only 3–7% recovering to their previous functional baseline (3). In cardiac arrest, brain injury is suggested to occur through a two-step process, with ischemia directly from cardiac arrest, which is then followed by a secondary re-perfusion injury. Iqbal et al. [2015] found that survival with favourable outcome falls significantly with each minute of CPR (4).
Four suggested criteria, which predict survival from OHCA include: cardiac arrest which is witnessed by a bystander or emergency service, as well as delivery of effective bystander CPR, a shockable cardiac rhythm, and ROSC at the scene (5).
TH
Following resuscitation, subsequent hypoxic brain injury still remains a significant cause of morbidity and mortality (2). TH following cardiac arrest, has been suggested to improve survival rates and offers neuroprotective benefits (6,7).
Cerebral ischemia can persist for hours after resuscitation, hence treatment with induced hypothermia has been proposed as a means to reduce cerebral oxygen requirement (2). There are several proposed theories as to why inducing mild hypothermia may improve neurological outcome following resuscitation. Hypothermia reduces the cerebral metabolism and hence subsequent oxygen demand. It also suppresses many chemical reactions that occur from reperfusion injury, including free radical production, excitatory amino acid release, and calcium shifts, which may subsequently lead to mitochondrial damage and cell death (6,7).
Mechanical resuscitation devices
Along with pre-morbid function and CPR duration, the quality of CPR plays a significant role in the outcome from resuscitation (3). Poor quality CPR is associated with reduced rates of ROSC, survival and favourable neurological outcomes (8,9). Studies suggest that quality of compression decreases after just the first minute of CPR (8), but even with adequate compressions, it is suggested that the probability of survival to hospital discharge with good outcome declines rapidly with each minute of CPR (8,10). Provider fatigue is a significant factor in quality of CPR, and hence mechanical chest compression devices should be considered when prolonged resuscitation is expected.
Mechanical chest compression devices can be used to aid resuscitation efforts, by providing consistent high-quality compressions. Whilst considered safe, numerous studies found no superiority over manual CPR (thought to be partly due to interruptions in CPR and delay in device deployment) (11-13). On the other hand, one can observe why its use would be positive in the case of prolonged resuscitation, during patient transport or during intervention such as PPCI.
Coronary artery disease and PPCI
A study by Iqbal et al. [2015], suggested that coronary artery disease accounts for >70% of OHCA, and that rapid access to a specialist heart attack centre improves outcome in this patient subgroup (4). Their paper identified predictors of survival and favourable function status, which include lower patient co-morbidity, provision of bystander CPR, a short duration of resuscitation, with VT/VF as the initial rhythm and absence of cardiogenic shock. A paper by Dumas et al. [2010] supported immediate intervention with coronary angiography in OHCA, in patients where no obvious non-cardiac cause of arrest (with or without ST-segment elevation) (14). They had similar findings, with a significant coronary artery lesion in 70% of patients following OHCA where no obvious non-cardiac cause of cardiac arrest was found. Their overall hospital survival was 39%, however, this rate increased from 31% (in patients with no or failed PCI) to 51% in patients that had successful immediate revascularization.
Iqbal et al. also found that the administration of adrenaline and inotropic support was associated with worse functional outcome. This is supported by a recent 2018 study which found that although adrenaline use resulted in a significantly higher survival rate, there was also a considerable associated increase in severe neurologic impairment with adrenaline use when compared with placebo (15).
Conclusions
The outcome from this case is clearly unexpected given the prolonged nature of resuscitation, particularly given the significant morbidity and mortality associated with OHCA. There were numerous favourable factors for survival, such as minimal patient co-morbidity, witnessed collapse and shockable initial rhythm, however, there was equally delay in bystander CPR, as well as the longevity of resuscitation itself. This case does highlight the value of mechanical resuscitation devices for consistent compressions, as well as consideration of early intervention with PCI in those with potential cardiac causes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript.
References
- Nolan J, Soar J. Resuscitation Guidelines 2015 Introduction. Resus Council (UK) [cited 25/7/18] Available online: https://www.resus.org.uk/resuscitation-guidelines/introduction/
- Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002;346:557-63. [Crossref] [PubMed]
- Patel JK, Chabra V, Parnia S. Making sense of clinical outcomes following cardiac arrest. Curr Opin Crit Care 2015;21:453-9. [Crossref] [PubMed]
- Iqbal MB, Al-Hussaini A, Rosser G, et al. Predictors of survival and favorable functional outcomes after an out-of-hospital cardiac arrest in patients systematically brought to a dedicated heart attack center (from the Harefield Cardiac Arrest Study). Am J Cardiol 2015;115:730-7. [Crossref] [PubMed]
- El Sayed M, Al Assad R, Abi Aad Y, et al. Measuring the impact of emergency medical services (EMS) on out-of-hospital cardiac arrest survival in a developing country: A key metric for EMS systems' performance. Medicine (Baltimore) 2017;96:e7570. [Crossref] [PubMed]
- Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002;346:549-56. [Crossref]
- Nolan JP, Morley PT, Vanden Hoek TL, et al. Therapeutic hypothermia after cardiac arrest: an advisory statement by the advanced life support task force of the International Liaison Committee on Resuscitation. Circulation 2003;108:118-21. [Crossref] [PubMed]
- Ochoa FJ, Ramalle-Gómara E, Lisa V, et al. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation 1998;37:149-52. [Crossref] [PubMed]
- Hightower D, Thomas SH, Stone CK, et al. Decay in quality of closed-chest compressions over time. Ann Emerg Med 1995;26:300-3. [Crossref] [PubMed]
- Reynolds JC, Frisch A, Rittenberger JC, et al. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies?. Circulation 2013;128:2488-94. [Crossref] [PubMed]
- Wik L, Olsen JA, Persse D, et al. Manual vs. integrated automatic load-distributing band CPR with equal survival after out of hospital cardiac arrest. The randomized CIRC trial. Resuscitation 2014;85:741-8. [Crossref] [PubMed]
- Smekal D, Johansson J, Huzevka T, et al. A pilot study of mechanical chest compressions with the LUCAS™ device in cardiopulmonary resuscitation. Resuscitation 2011;82:702-6. [Crossref] [PubMed]
- Rubertsson S, Lindgren E, Smekal D, et al. Mechanical chest compressions and simultaneous defibrillation vs conventional cardiopulmonary resuscitation in out-of-hospital cardiac arrest: the LINC randomized trial. JAMA 2014;311:53-61. [Crossref] [PubMed]
- Dumas F, Cariou A, Manzo-Silberman S, et al. Immediate percutaneous coronary intervention is associated with better survival after out-of-hospital cardiac arrest: insights from the PROCAT (Parisian Region Out of hospital Cardiac ArresT) registry. Circ Cardiovasc Interv 2010;3:200-7. [Crossref] [PubMed]
- Perkins GD, Ji C, Deakin CD, et al. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med 2018;379:711-21. [Crossref] [PubMed]
Cite this article as: Butter C, Somasundaram K. Survival after out of hospital cardiac arrest with prolonged period of resuscitation (250 minutes). J Emerg Crit Care Med 2019;3:19.