Knowledge retention of the traumatic brain injury guidelines at a Level 1 trauma center
Introduction
According to the Institute of Medicine 2012 report, there is a need for trauma education and training not only for nursing but for all healthcare providers. Trauma/unintentional injury is the leading cause of death in those age 1–45 and the 3rd leading cause of death overall in all groups with an annual cost of 671 billion dollars according to the National Trauma Statistics (1,2). Traumatic brain injury (TBI) accounts for one third or thirty percent of injury related deaths in the United States (2). There are 2.8 million traumatic brain injuries with approximately 282,000 of those persons being hospitalized. In 2000 the cost of TBI related direct medical cost and indirect cost, loss of productivity was $60 billion (3,4). Therefore, it is imperative that continuing education is provided in an efficient manner especially for the trauma population. Implementation of evidence-based guidelines has been associated with a decrease in overall TBI mortality (4,5). In addition to impacting mortality, adherence to establish TBI treatment implementation guidelines and early interventions can decrease the incidence of disabilities associated with TBI (5-8). Despite the important benefits of reduction in morbidity and mortality associated with adhering to TBI guidelines, compliance with the guidelines remained poor (6-11). Therefore the focus of our review was on the educational process and knowledge retention regarding the TBI guidelines.
The implementation of the educational process to improve the compliance of our institutional TBI guidelines was only a portion of the complete process improvement project. The education process was utilized to ensure the nurses and resident physicians who cared for patients with traumatic brain injuries were able to identify the appropriate guideline to follow. Education on the updated institutional guidelines is imperative because caring for patients with severe TBI is a fluid and dynamic process which requires a basic understanding of the underlying pathophysiology in order to understand the significance of clinical changes and make appropriate adjustments in therapy at the bedside in real time based on pre-established guidelines.
The implementation of a new learning process to ensure that education is provided across the continuum of care can be a daunting task especially in the healthcare arena. The demanding and productivity-based environment in healthcare does not always lend itself to a positive approach to education. There are many time constraints placed on the learner as well as the educator to provide meaningful education and a means in which the learner feels compelled to be present in the education process (12). The atmosphere and climate that provides the best approach to entitle the learner to be present is one in which they feel that they will gain from this experience (13). As healthcare educators we must possess the knowledge of the learning styles of our learners. Due to time constraints, the educational process was developed to incorporate the three basic learning styles: visual, auditory, kinesthetic (Table 1) (14).
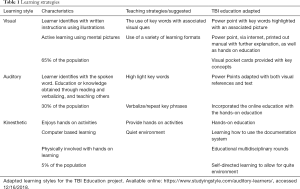
Full table
Most learners engage in education to understand a new skill, behavior or attitude and develop the knowledge needed to extrapolate and utilize the new process (15). Adult learners achieve the most satisfaction when they engage in meaningful education (15). Although a majority of the participants had a prior knowledge regarding the TBI guidelines, there were changes that required acknowledgment to sustain compliance with the institutional guidelines. The guideline for traumatic brain was changed to meet the newest brain trauma foundation guidelines. Our institutional guidelines were reduced and simplified from a fifteen page document to a four page document. This required all participants to have a strong foundation in TBI care in addition to understanding the newly revised guidelines
The on-line NetLearning® system was utilized to distribute the education material. The process was easily accessible to the participants and they already had a familiarity of the learning system. Adult learners gain value from self-directed learning to feed the intrinsic need for timely or self-directed knowledge. It is for this reason the on-line NetLearning® system was used to provide self-directed learning modules. It is evident that we need a more effective teaching method related to the decreased work hours of our residents, increased responsibility of the nursing staff as well as the ongoing clinical demands of the in-patient setting (16). However, not all individual learners can use a self-directed learning approach. Therefore, the on- line self -directed learning module was coupled with a hands-on learning portion.
Methods
This was a process improvement endeavor to ensure institutional compliance with the newly implemented revised TBI guidelines, the education and knowledge retention was a small portion of the project. The testing process was implemented through an on-line NetLearning® program which was available to all Memorial Medical Center employees who were involved with the care of the traumatic brain injured patient in the intensive care setting, including the resident physicians and critical care nurses who were required to access and review the educational materials as well as complete the pre and posttests. The pre-test was administered prior to reviewing the educational material. Immediately following the pretest, education was provided through the online learning modality which consisted of a PowerPoint presentation which described all the changes to the TBI guideline. Immediately following, there was a test in which all participants completed (post-test). At 6 months they again were required to participate in the traumatic brain injury on-line test. However, at 6 months there was no education provided as we were looking for knowledge retention.
The performance improvement project did not focus on the educational background, years of experience, and or years associated with the use of the TBI protocol. Unfortunately there was no data collection for this criteria related to the education. We can state that the resident physicians had approximately 3–5 years of experience and the nurses had anywhere between 6 months and 50 years of nursing experience. The nurses have to exhibit proficiency in TBI care to be considered the primary nurse. The nurses also complete a four hour TBI education dedicated to the pathophysiology, guidelines, equipment necessary to care for the patient’s.
This process improvement project was implemented at MMC, a rural community, non-university based Level 1 trauma center in west central Pennsylvania. Approval was obtained from the MMC Scientific Review Committee of the Office of Research Administration, as a quality improvement project. Consent was not required for this quality improvement project.
Results
Data analysis
Education: pre-test, immediate post-test and 6-month post-test scores were reported as mean with standard deviation for nurses and residents completing all three tests. The combined group (nurses and resident physician) mean scores were compared across the three time points using two-way repeated measures ANOVA with Bonferroni correction to adjust for multiple testing. The software that was utilized was the IBM SPSS v. 24.0. A P value of <0.0005 was consider statistically significant.
TBI education module
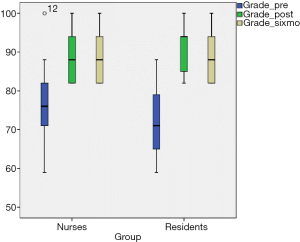
Thirty-nine ICU nurses and nineteen resident physicians completed the educational module, the pretest and immediate posttest. Of those, twenty nine nurses and twelve resident physicians completed the 6-month posttest and these scores were compared between groups. The difference in the numbers at 6 months is related to the turnover of nursing and graduation of resident physicians. The mean score on the pretest for nurses (75%±9.75%) and resident physicians (73%±8.54%) was similar. Likewise, improvements were seen in both groups for the immediate post-test with nurses scoring (88%±6.31%) and physicians (91%±5.98%). The improvement in scores was sustained at the 6-month point for both nurses and physicians (Table 1). For the nurse and physician combined scores there was a statistically significant improvement between pretest and immediate posttest mean scores (74%±9.35% pre vs. 88%±6.23% post, P<0.0005), and no meaningful change between the immediate post-test and 6-month post test scores, indicating sustained improvement (Figure 1).
Discussion
Implementation of education on an institutional specific TBI guideline in a Level I trauma center has a variety of obstacles to overcome. The education needs to be timely as well as implemented throughout multiple shifts and disciplines. Learning styles further limit the dissemination of education across disciplines. Challenges associated with devising an education process that is suitable to all disciplines are extensive and further inhibited by the pre-existing cognitive experience of the participants. There must be some aspect of TBI knowledge in order to comprehend the newly revised TBI algorithms for treatment guidelines. The cohort of nurses and residents who were evaluated in this education process have a varying degree of background in the treatment of trauma patients as well as in the use of the TBI guidelines and care of the TBI patient. Achieving the most appropriate educational method was paramount and research has shown that the standard method using continuing education paradigm, relied on teacher vs student. This method of training has a unilateral flow which provides knowledge from the instructor to the student (8). Education between clinician and learner should be based on a collaborative approach (5). In addition the learner must have an understanding as to why this education is important. Young adults are more adapt at self-learning concepts at which the education process can be unilateral, and they can still ascertain the knowledge that is needed from self-learning on-line education. A knowledge gap of the provided information is also an important aspect of the process, as all participants must understand that there is a gap in the current knowledge regarding the process and the process in which they are being educated. In order to provide knowledge across all disciplines and levels of knowledge, supplemental information was provided in the form of journals as well as provided in the PowerPoint. The education was also offered with a continuing credit in trauma hour.
Although with standard Continuing Learning (CE) education processes, the credit is obtained by being present, most often there was not an evaluation of the learned education. The TBI education process required being present as well as determination of knowledge retention. In order to attain the CE for completion of the TBI guidelines education the participant had to complete all portions of the education which included the on-line NetLearning® portion, hands-on portion utilizing super trainers from both the residents and nursing staff, a review on the on-line documentation form, and on-going evaluation through daily multidisciplinary rounds on the TBI patients.
The education process used in the implementation of the new institution specific revised TBI guidelines. This education process was a part of a separate project ensuring compliance, utilizing an electronic TBI tracking tool and with the newly updated institutional specific revised TBI guidelines The education process and the retention of knowledge which is being reported in this article, is directly related to the compliance with TBI guidelines. The data for compliance tracking is not being reported as the information is too extensive for review in this brief review.
The institutional TBI guidelines were utilized at the bedside by the nurses and residents who cared for TBI patients. The guidelines are printed and at the bedside and used as a visual que while caring for the patient. An understanding of the concepts associated with the guidelines was important in the application of treatment measures at the bedside. The educational design accounted for the varying levels of experience and education of the participants. Perception on comprehension of visual images is often directly related to the design of the presentation but it plays an important part in the depths of cognition (17).
Limitations
The study participants that followed through to the 6-month evaluation was limited by the loss of nursing staff and the graduation of the resident physicians. However, because they no longer were caring for TBI patient at 6 months, they were excluded. The implementation of the education process used a pre-test prior to the education. The post test was delivered following the education process. There was not a defined time between the pretest and the posttest as this was a self-paced educational program. This may have made a difference in the original pre-test and posttest numbers. However, this would not have affected the 6-month knowledge retention during which time there was no further education provided. There was a potential for limitations regarding the learning styles of the participants to gear the education to meet most of the learning styles. The education could have been further enhanced with the use of a learning style survey. There were limitations in this review related to the baseline characteristics of the nurses and resident physician’s. This data collection was not completed as it was not the primary process improvement project.
Further investigation
A twelve-month posttest evaluation to determine knowledge retention at 12 months. As mentioned previously, the use of a learning style survey could further enhance future studies regarding knowledge retention.
Conclusions
This education process played an imperative part in the implementation of the new TBI guidelines at our institution. The education process employed was devised to meet the needs of a variety of learning methods among variable levels of healthcare knowledge regarding the use of TBI guidelines and the care of the TBI patient. The post test scores were sustained for both residents and nurses at 6 months. Identifying that the need for further education prior to 6 months is not necessary. Further investigation would be beneficial to determine when the knowledge retention would begin to deteriorate. This would provide a timeline for further education regarding the TBI guidelines.
Acknowledgements
Jodi Noon RN, CCRN, DLP-Memorial Medical Center. The authors thank Jodi Noon RN, CCRN who worked in the critical care unit at the time of the study and was instrumental in the data extraction, hands-on education, and super trainer for the electronic TBI tracking tool. Tom Simunich, MS, MBA, statistician. The authors thank Thomas Simunich, MS, MBA a research statistician at DLP-Memorial Medical Center for conducting the statistical testing.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Available online: https://www.nattrauma.org/what-is-trauma/trauma-statistics-facts/, accessed 9/12/2018.
- Available online: https://www.cdc.gov/traumaticbraininjury/data/dist_death.html, accessed 9/12/2018.
- Available online: https://www.brainline.org/article/get-stats-traumatic-brain-injury-united-states, accessed 12/16/2018.
- Available online: https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_06.pdf, accessed 9/12/2018.
- Carney N, Totten AM, O'Reilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery 2017;80:6-15; discussion 499-500.
- Fakhry SM, Trask AL, Waller MA, et al. Management of brain- injured patients by an evidence based medicine protocol improves outcomes and decreases hospital charges. J Trauma 2004;56:492-499. [Crossref] [PubMed]
- Arabi YM, Haddad S, Tamim HM, et al. Mortality reduction after implementing a clinical practice guidelines-based management protocol for severe traumatic brain injury. J Crit Care 2010;25:190-5. [Crossref] [PubMed]
- Chesnut RM. Care of central nervous system injuries. Surg Clin North Am 2007;87:119-56. vii. [Crossref] [PubMed]
- Hesdorffer DC, Ghajar J, Iacono L. Predictors of compliance with the evidence-based guidelines for traumatic brain injury care: A survey of United States trauma centers. J Trauma 2002;52:1202-9. [Crossref] [PubMed]
- Vukic M, Negovetic L, Kovac D, et al. The effect of implementation of guidelines for the management of severe head injury on patient treatment and outcome. Acta Neurochir (Wien) 1999;141:1203-8. [Crossref] [PubMed]
- American College of Surgeons Trauma Quality Improvement Program. ACS TQIP best practices in the management of traumatic brain injury.
- Beckman TJ, Lee MC. Proposal for a collaborative Approach to Clinical Teaching. Mayo Clin Proc 2009;84:339-44. [Crossref] [PubMed]
- Bankert EG, Kozel VV. Transforming Pedagogy in Nursing Education: A caring learning environment for adult students. Nurs Educ Perspect 2005;26:227-9. [PubMed]
- Sparling LA. Enhancing the Learning in Self-Directed Learning Modules. J Nurses Staff Dev 2001;17:199-205. [Crossref] [PubMed]
- Stickrath C, Aagaard E, Anderson M. MiPLAN: a learner-centered model for bedside teaching in today's academic medical centers. Acad Med 2013;88:322-7. [Crossref] [PubMed]
- Russell SS. An overview of adult-learning processes. Urol Nurs 2006;26:349-52, 370. [PubMed]
- Lee H, Plass JL, Homer BD. Optimizing cognitive load for learning from computer-based science simulations. J Educ Psychol 2006;98:902-13. [Crossref]
Cite this article as: Gorman KM, Dumire RD. Knowledge retention of the traumatic brain injury guidelines at a Level 1 trauma center. J Emerg Crit Care Med 2019;3:17.