Utility of ultrasound of upper airway for confirmation of endotracheal intubation and confirmation of the endotracheal tube position in the intensive care unit patients
Introduction
Endotracheal intubation in the intensive care unit (ICU) is an extremely high risk procedure since the ICU patients are much sicker, with poor physiological reserve. Any delay in recognition of an oesophageal intubation or repeated attempts to intubate can lead to disastrous consequences (1,2). The NAP 4 Audit conducted in UK showed that 25% of airway complications happen in the ICU (3). Emergency endotracheal intubations are associated with higher incidence of oesophageal tube placement and delayed recognition of incorrect placement. A prospective study of all emergency intubations found that in 8% of total intubation attempts, the endotracheal tube (ETT) was initially placed into the oesophagus (2). Presently the waveform capnography is considered the standard of care for the confirmation of ETT placement and though this is highly sensitive and specific, it can have malfunction and mechanical problems and can be less reliable in low cardiac output states or cardiac arrest situations (4). It needs 4 to 5 breaths to confirm correct ETT placement and hence takes vital time. Also one may encounter malfunctioning gas analysers. It’s not only important to place ETT in the trachea but it’s equally important to place the ETT at correct depth in trachea since placement of tube too far in or too far out can lead to complications. Routine clinical examination is unreliable to identify correct depth of tube placement. Ideal ETT tip position should be in the mid-trachea (around 4 cms above the carina), and inappropriate positioning can result in unintended extubation, carinal stimulation or endobronchial placement. Various methods that have been described to confirm the correct position of ETT tip are predictive length of ETT placement according to height of the patient, cuff palpation in suprasternal notch (5,6), radiological confirmation (7) and fibreoptic bronchoscopy (FOB). FOB is considered to be the most dependable and the gold standard (8). However, each of these methods has their own limitations. Palpating ETT cuff at suprasternal notch may not always be feasible especially in patients with unfavorable neck anatomy. Chest X-ray may not be readily available, and is associated with radiation exposure; and availability of bronchoscope also can be an issue in many ICUs. Traditionally final position of tube depth was decided according to the height of the patient and most standard text books advice fixing the ETT at about 21 cm for females and 23 cm for males at incisor teeth level (9,10), however following western guidelines can result in significant malposition of ETT (11). Moreover, chest radiography takes time and is cumbersome to be done in the ICU.
Point of care ultrasound is being increasingly used in emergency situations and in the ICU. It is commonly used to evaluate and monitor different clinical conditions in the ICU (12). It is also being used to evaluate the airway for preintubation assessment before intubation, double-lumen intubation, and extubation outcomes. One important use is correct ETT placement in the trachea (13). Confirmation of ETT position with ultrasound can be a potential alternative to capnography. Previous studies in adults and pediatrics evaluating ultrasound for confirming ETT intubation has shown high sensitivity and specificity (14,15).
Air is a poor medium for propagation of ultrasound waves and it does not let us visualize the position of ETT. However, ultrasound of the saline-filled ETT cuff can be used to determine appropriate ETT depth in the trachea. The ultrasound of saline-filled cuff technique is a rapid and reliable method, involves no radiation, requires no patient positioning, and can be done as many times as needed. Very few studies regarding use of ultrasound and saline-filled cuff to confirm ETT placement have been described before with different ultrasound techniques (16,17).
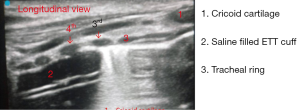
We hypothesized that placing upper edge of saline filled cuff at the level of 3rd and 4th tracheal ring would correlate with position of ETT tip appropriately i.e., between sternoclavicular joint above to 4 cm above carina below.
Methods
This prospective observational study was conducted to determine the role of ultrasound for confirmation of ETT placement in trachea (snow storm sign) and accuracy of correct depth of insertion of ETT in trachea with the use of ultrasonography to visualize saline filled cuff technique in adult ICU patients. After obtaining Institutional Ethical Committee (IEC) approval, this study was conducted at mixed medical surgical oncological ICU over a period of 1 year. IEC allowed deferred consent. All adult patients requiring intubation in the ICU were screened for inclusion in the study.
We excluded patients who required intubation during cardiac arrest. We followed institutional ICU protocol for intubation. This includes rapid assessment of airway, and rapid sequence intubation with Sellick’s manoeuvre and confirmation of correct tube placement using waveform capnography. All intubations were performed by a trained intensive care fellows and Anaesthesiologists. The male patient’s trachea was intubated with ETT No. 8 and in females a 7.0 ETT was used. Upper airway ultrasonography was performed during intubation by an intensivist trained in airway ultrasonography.
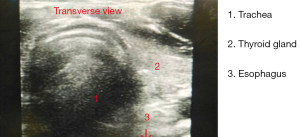
The linear probe (7–13 MHz Sonosite M-Turbo®/MyLab™Five Esaote) was placed transversely over trachea between suprasternal notch and cricothyroid membrane during intubation and presence or absence of snow storm sign (disturbance of tracheal air-mucosa interface with comet tail artefacts) was reported during intubation (Figure 1). Efforts were made to identify oesophageal opening on ultrasound and oesophageal intubation was identified by appearance of double track sign and absence of loss of snow storm sign (18-21). Endotracheal intubation was confirmed with waveform capnography and the tube was fixed. After fixation of the tube ultrasound of trachea was performed in sagittal plane to identify the cricoid cartilage and the tracheal rings. ETT cuff was completely deflated and re-inflated with 10cc normal saline. ETT cuff was identified as anechoic shadow in trachea. The upper end of cuff was fixed at the level at 3rd or 4th tracheal ring (Figure 2). After final placement of the tube, the saline from ETT cuff was aspirated and cuff was re-inflated with air to maintain intracuff pressures between 20–25 cm H2O. To determine the volume of the saline we did few pilot cases and found that 10 cc saline was appropriate for ultrasound visualisation of tube cuff and was not associated with high cuff pressures.
Final position of tube tip was confirmed on chest X-ray AP view with the neck in neutral position with the bed at semi recumbent position. The desired position of ETT tip on X-ray was between the sternoclavicular joint superiorly and at least 4 cm above carina inferiorly for determining appropriateness of the tube position. The distance of ETT tip was measured from carina on X-ray chest AP view by digital caliper measurement. If the ETT tip position was found to be inappropriate, the ETT was repositioned and the finding recorded for analysis. Any complications during the intubation were also recorded.
Statistical analysis
We recorded loss of snow storm sign as an indication of endotracheal intubation. We also recorded number of times double track sign was visualised during intubation that suggested oesophageal intubation. We looked at the concordance between tracheal ultrasound and capnography for detecting endotracheal intubation and compared airway USG to X-ray for position of tube depth by using the McNamar test. Specificity, sensitivity, and appropriateness of tube position, positive predictive value was calculated using standard formulae. All statistical analyses were performed using SPSS statistical software, version 20.
Results
A total of 89 intubations were included in the study over a period of one year. All the intubations were confirmed with capnography, and there were no complications noted in relation to ultrasonography. The ultrasound confirmation of the placement of the tube with the loss of snow storm sign was seen in 86 patients. In 3 patients, we could not visualise loss of snow storm sign however the intratracheal position was confirmed by capnography and identified with inflation of saline filled cuff on ultrasound. In 2 patients, we identified oesophageal intubation real time with positive double track sign with absence of loss of snow storm sign and thus avoided oesophageal intubation by withdrawing the ETT and reinserting it in the trachea. In these two patients we did not wait to confirm oesophageal intubation by capnography since it would entail the risk and possibility of ventilating the stomach and increase chance of aspiration in critically ill patients. The capnographic confirmation was done after reinserting the tube in the trachea.
The saline filled cuff could be visualized in all 89 patients.
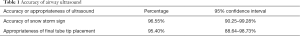
The overall sensitivity of airway ultrasound for confirmation of ETT placement was 96.55% (CI: 90.25–99.28%). The PPV was 100% (CI: 0.94–1.00). The double track sign specific for oesophageal intubations was seen in 2 patients. Three patients were found to have inappropriate ETT tip placement on X-ray which required tube repositioning thus the accuracy for depth of insertion of ETT by airway ultrasound as compared to X-ray was found to be 95.40% (CI: 88.64–98.73%) (Table 1). No complications were observed related to cuff inflation and deflation and to use of airway ultrasound.
Full table
In our study we found that ultrasound probe did not interfere with performance of Sellick’s manoeuvre. However, the Sellick’s manoeuvre had to be terminated in 2 patients to facilitate tube placement.
Discussion
In this prospective observational study, we found that airway ultrasonography is useful for confirmation of tracheal intubation with high sensitivity (96.55%). Tracheal intubation performed in the ICU can be technically challenging, with less experienced clinicians under suboptimal conditions doing high risk intubations. This may result in complications such as oesophageal intubation, delayed or traumatic intubation with associated complications. Although direct visualization of the ETT passing through the vocal cords confirms correct tracheal placement, it cannot confirm correct ETT depth of insertion. Clinical assessment by auscultation and chest rise may not detect malpositioned ETT.
Quantitative waveform capnography is the standard of care for confirmation of correct tracheal ETT placement and is also recommended by 2015 AHA resuscitation guidelines (22,23). Capnography has its own limitations in low cardiac output states and cardiac arrest situations (24). It can confirm tracheal intubation but provides no information on ETT depth in the trachea (25-31).
Chest radiography is commonly used to confirm position of ETT but is time-consuming, and may require patient movement which may be sometimes difficult. The safety of ultrasound has been widely accepted in clinical practice however the applications for airway and lungs were not popular before as air is a poor conductor of ultrasound waves (26). However, in late 90s and early 2000s, studies showed that using artifacts generated during ultrasonography, one can detect many pathologies of lungs and also use ultrasound to aid bedside procedures (27-30). Using ultrasound of airway to predict difficult airway and as an aid during intubation has gained momentum recently (31-33).
Various studies have used ultrasound of neck, or anterior chest for lung slide or subcostal diaphragmatic movement for confirmation of ETT placement (34-37). Trans-cricoid or trans- thyroid ultrasonography and ultrasonography for assessing lung slide were found to have 100% sensitivity and specificity in verification of tube placement in emergency settings (35). Radiological sign that has been described to confirm ETT placement takes into account disturbance of the air mucosa interface (called the snowstorm sign). We looked at confirmation of ETT position by loss of snowstorm sign (38-40). We also confirmed the placement of ETT at an appropriate depth in the trachea with the saline filled cuff technique and compared it with the current gold standard i.e., the chest X-ray.
We found that airway ultrasound can be used for rapidly detecting ETT placement in trachea.
In our study the airway ultrasonography was able to confirm ETT placement with 96% sensitivity and 100% specificity. Loss of snow storm sign was identified in all patients except 3 patients in whom the tube placement was confirmed by capnography. The saline filled cuff was visualized in all patients and was 100% specific for correct depth of ETT in the trachea when compared with chest X-ray. In 2 patients, we could detect esophageal intubation in real time by identifying the double track sign and absence of loss of snow storm sign and hence may have prevented esophageal intubations.
While a cuff filled with air cannot be sonographically distinguished from the surrounding air-filled trachea, prior reports in adult cadavers showed that ultrasonography at the suprasternal notch can visualize a saline-inflated ETT cuff (41).
In a recent study, Chen et al. looked at combined video laryngoscope, fibrescope and ultrasound with saline filled cuff technique to measure correct depth insertion of ETT and found excellent results but this method can only confirm appropriate upper end of the tube (15).
We hypothesized that if we positioned the upper border of saline-filled ETT cuff at the level of 3rd or 4th tracheal ring, it will result in correct position of tip of ETT.
We found that accuracy for appropriateness of final position of ETT by ultrasonography as compared to chest X-ray was 95.40%.
It has been speculated that performing ultrasonography in the anterior neck area can adversely affect the success of intubation hence studies have looked at lung slide or subcostal diaphragmatic motions to confirm ETT placements. In our study there was no hindrance to application of Sellick’s manoeuvre during ultrasound confirmation of ETT placement, however in 2 patients the Sellick’s manoeuvre had to be discontinued for facilitation of ETT insertion. In our study the ETT was placed in the oesophagus in 2 patients (2.0%). This rate of esophageal intubation is far less than other studies (2,3). This may be because in our study all intubations were performed by Anesthesiology and Intensive care fellows.
Our study is unique in the fact that we used ultrasonography to confirm correct tracheal placement of ETT and ascertain the appropriate depth of ETT position in trachea in ICU patients.
The learning curve for performing ultrasound for ETT confirmation has not been found to be difficult. Moreover, ultrasound is an important tool in the day to day diagnosis, management and clinical decision making in the ICU (42,43).
Conclusions
This prospective study suggests that airway ultrasonography can be used as an adjunct to capnography for real time and rapid confirmation of ETT placement. Airway ultrasonography, using a saline-filled ETT cuff can accurately and rapidly confirm the appropriate depth of tube placement in the trachea and can avoid the need for chest X-ray for tube confirmation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Institutional Ethical Committee (IEC) and IEC allowed deferred consent.
References
- Adriani J. Unrecognized esophageal placement of endotracheal tubes. South Med J 1986;79:1591-3. [Crossref] [PubMed]
- Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults a prospective investigation of 297 tracheal intubations. Anesthesiology 1995;82:367-76. [Crossref] [PubMed]
- Cook TM, Woodall N, Harper J, et al. Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth 2011;106:632-42. [Crossref] [PubMed]
- Grmec Š. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med 2002;28:701-4. [Crossref] [PubMed]
- McKay WP, Klonarakis J, Pelivanov V, et al. Tracheal palpation to assess endotracheal tube depth: an exploratory study. Can J Anaesth 2014;61:229-34. [Crossref] [PubMed]
- Cullen DJ, Newbower RS, Gemer M. A new method for positioning endotracheal tubes. Anesthesiology 1975;43:596-9. [Crossref] [PubMed]
- Brunel W, Coleman DL, Schwartz DE, et al. Assessment of routine chest roentgenograms and the physical examination to confirm endotracheal tube position. Chest 1989;96:1043-5. [Crossref] [PubMed]
- Angelotti T, Weiss EL, Lemmens HJ, et al. Verification of endotracheal tube placement by prehospital providers: is a portable fiberoptic bronchoscope of value? Air Med J 2006;25:74-8. [Crossref] [PubMed]
- Gal TJ. Airway management. In: Miller RD. editor. Anesthesia, 6 edition. Philadelphia: Elsevier, 2005:1617-52.
- Dorsch JA, Dorsch SE. Carbon dioxide analysis. Understanding anesthesia equipment. 4th ed. Baltimore: The Williams & Wilkins Co., 1999:714-33.
- Varshney M, Sharma K, Kumar R, et al. Appropriate depth of placement of oral endotracheal tube and its possible determinants in Indian adult patients. Indian J Anaesth 2011;55:488-93. [Crossref] [PubMed]
- Reardon R, Heegaard B, Plummer D, et al. Ultrasound is a necessary skill for emergency physicians. Acad Emerg Med 2006;13:334-6. [Crossref] [PubMed]
- Sustić A. Role of ultrasound in the airway management of critically ill patients. Crit Care Med 2007;35:S173-7. [Crossref] [PubMed]
- Galicinao J, Bush AJ, Godambe SA. Use of bedside ultrasonography for endotracheal tube placement in pediatric patients: a feasibility study. Pediatrics 2007;120:1297-303. [Crossref] [PubMed]
- Ramsingh D, Frank E, Haughton R, et al. Auscultation versus Point-of-care Ultrasound to Determine Endotracheal versus Bronchial Intubation: A Diagnostic Accuracy Study. Anesthesiology 2016;124:1012-20. [Crossref] [PubMed]
- Chen X, Zhai W, Yu Z, et al. Determining correct tracheal tube insertion depth by measuring distance between endotracheal tube cuff and vocal cords by ultrasound in Chinese adults: a prospective case-control study. BMJ Open 2018;8:e023374. [Crossref] [PubMed]
- Tessaro MO, Salant EP, Arroyo AC, et al. Tracheal rapid ultrasound saline test (TRUST) for confirming correct endotracheal tube depth in children. Resuscitation 2015;89:8-12. [Crossref] [PubMed]
- Raphael DT, Conard FU. Ultrasound confirmation of endotracheal tube placement. J Clin Ultrasound 1987;15:459-62. [Crossref] [PubMed]
- Vaghadia H, Jenkins LC, Ford RW. Comparison of end-tidal carbon dioxide, oxygen saturation and clinical signs for the detection of oesophageal intubation. Can J Anaesth 1989;36:560. [Crossref] [PubMed]
- Drescher MJ, Conard FU, Schamban NE. Identification and description of esophageal intubation using ultrasound. Acad Emerg Med 2000;7:722-5. [Crossref] [PubMed]
- Milling TJ, Jones M, Khan T, et al. Transtracheal 2-d ultrasound for identification of esophageal intubation. J Emerg Med 2007;32:409-14. [Crossref] [PubMed]
- Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: adult advanced cardiovascular life support. Circulation 2015;132:S444-64. [Crossref] [PubMed]
- MacLeod BA, Heller MB, Gerard J, et al. Verification of endotracheal tube placement with colorimetric end-tidal CO2 detection. Ann Emerg Med 1991;20:267-70. [Crossref] [PubMed]
- Cook TM, Nolan JP. Use of capnography to confirm correct tracheal intubation during cardiac arrest. Anaesthesia 2011;66:1183-4. [Crossref] [PubMed]
- Li J. Capnography alone is imperfect for endotracheal tube placement confirmation during emergency intubation1. J Emerg Med 2001;20:223-9. [Crossref] [PubMed]
- Merritt CR. Ultrasound safety: what are the issues? Radiology 1989;173:304-6. [Crossref] [PubMed]
- Yang PC, Luh KT, Chang DB, et al. Ultrasonographic Evaluation of Pulmonary Consolidation. Am Rev Respir Dis 1992;146:757-62. [Crossref] [PubMed]
- Lichtenstein D, Hulot JS, Rabiller A, et al. Feasibility and safety of ultrasound-aided thoracentesis in mechanically ventilated patients. Intensive Care Med 1999;25:955-8. [Crossref] [PubMed]
- Lichtenstein D, Goldstein I, Mourgeon E, et al. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 2004;100:9-15. [Crossref] [PubMed]
- Werner SL, Smith CE, Goldstein JR, et al. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med 2007;49:75-80. [Crossref] [PubMed]
- Kabil AE, Ewis AM, Al-Ashkar AM, et al. Real-time tracheal ultrasonography for confirming endotracheal tube placement. Egypt J Bronchol 2018;12:323-8. [Crossref]
- Chou HC, Tseng WP, Wang CH, et al. Tracheal rapid ultrasound exam (TRUE) for confirming endotracheal tube placement during emergency intubation. Resuscitation 2011;82:1279-84. [Crossref] [PubMed]
- Takeda T, Tanigawa K, Tanaka H, et al. The assessment of three methods to verify tracheal tube placement in the emergency setting. Resuscitation 2003;56:153-7. [Crossref] [PubMed]
- Park SC, Ryu JH, Yeom SR, et al. Confirmation of endotracheal intubation by combined ultrasonographic methods in the emergency department. Emerg Med Australas 2009;21:293-7. [PubMed]
- Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med 2006;13:239-44. [Crossref] [PubMed]
- Hosseini JS, Talebian MT, Ghafari MH, et al. Secondary confirmation of endotracheal tube position by diaphragm motion in right subcostal ultrasound view. Int J Crit Illn Inj Sci 2013;3:113. [Crossref] [PubMed]
- Oulego-Erroz I, Alonso-Quintela P, Rodriguez-Blanco S, et al. Verification of endotracheal tube placement using ultrasound during emergent intubation of a preterm infant. Resuscitation 2012;83:e143-4. [Crossref] [PubMed]
- Sağlam C, Ünlüer EE, Karagöz A. Confirmation of endotracheal tube position during resuscitation by bedside ultrasonography. Am J Emerg Med 2013;31:248-50. [Crossref] [PubMed]
- Arntfield RT, Millington SJ. Point of care cardiac ultrasound applications in the emergency department and intensive care unit-a review. Curr Cardiol Rev 2012;8:98-108. [Crossref] [PubMed]
- Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med 2011;364:749-57. [Crossref] [PubMed]
- Uya A, Spear D, Patel K, et al. Can Novice Sonographers Accurately Locate an Endotracheal Tube With a Saline-filled Cuff in a Cadaver Model? A Pilot Study. Acad Emerg Med 2012;19:361-4. [Crossref] [PubMed]
- Gottlieb M, Bailitz JM, Christian E, et al. Accuracy of a novel ultrasound technique for confirmation of endotracheal intubation by expert and novice emergency physicians. West J Emerg Med 2014;15:834. [Crossref] [PubMed]
- Blehar DJ, Barton B, Gaspari RJ. Learning curves in emergency ultrasound education. Acad Emerg Med 2015;22:574-82. [Crossref] [PubMed]
Cite this article as: Patil V, Bhosale S, Kulkarni A, Prabu N, Bhagat V, Chaudhary H, Sarawar S, Narkhede A, Divatia J. Utility of ultrasound of upper airway for confirmation of endotracheal intubation and confirmation of the endotracheal tube position in the intensive care unit patients. J Emerg Crit Care Med 2019;3:15.