
The evolution of trauma performance improvement
Introduction
It is well known that trauma takes a heavy toll in the United States emotionally and financially. Trauma is the number one cause of death between the ages of 1 and 44. According to the CDC, there is a trauma-related death every 3 minutes. In 2013, 617 billion dollars were spent on trauma, with $457 million being spent on nonfatal injuries (1). As a result of injury and violence, 2.5 million people were hospitalized, and nearly 26.9 million were treated in Emergency Departments in 2014. In trauma’s early beginnings, the lessons of war evolved into a civilian system that would be based on standards and evidence-based practices. These trauma programs and systems would ultimately be evaluated by the level of care achieved through a layered and detailed performance improvement (PI) program. PI itself would evolve from a system of retrospective chart reviews into a hybrid concurrent review process and with rich data integration. Through these efforts, PI has achieved leadership status in the medical community with proven human and financial savings.
Early beginnings
Trauma PI has been the back bone of trauma care since its earliest development. When trauma care was formally organized in the 1970’s, the concepts were grounded in improving care. In 1976, Dr. James Styner, an orthopedic surgeon, crashed his small plane in rural Nebraska, killing his wife and critically injuring his three children. He had flagged down a passing car and was taken to a hospital that was initially closed, and the doctor had to be called in to open the facility. The care was so inadequate; he vowed to change a system that he stated was broken (2). His pursuit led to the origins of Advanced Trauma Life Support, the standards we use to care for our most injured trauma patients.
In that same year, the American College of Surgeons (ACS) “Optimal Hospital Resources for Care of the Seriously Injured” first described the criteria for the categorization and requirements for trauma centers. Along with requirements for personnel and equipment, it also stated that “Regularly scheduled quality assurance audits, and reviews and critiques of all professional and non-professional services are, of course, mandatory” (3). They further describe medical care evaluation for:
- Special audit for trauma deaths;
- Morbidity and mortality review;
- Trauma conference, multidisciplinary;
- Medical nursing audits, utilization review, tissue review;
- Medical record review.
In 1979, the standards added Outreach, public education, and qualified personnel under the auspice of Quality Assurance. In the 1986 update, the trauma registry was required to document the severity of injury and outcome with monthly review of statistics (4). While medical care evolved through the years, such as the use of MAST garments and tourniquets, so had PI. Quality indicators, in the form of audit filters and qualified complications, were added to the items to be tracked. While trauma leadership continued to evolve and develop trauma PI and standards, the mainstream medical community was publishing literature that would also influence trauma care.
Impact from mainstream medicine
Addressing system issues and personal accountability are some of the early hallmarks of trauma PI programs. In 1990, the Institute of Medicine prepared a report stating that over 98,000 hospitalized American deaths were due to medical errors. The report; To Err is Human, provided differing viewpoints of these causes. While system failures often created the most injuries, no blame takes away accountability (5). Unfortunately, there have been further studies that suggest the number of deaths is much higher.
In 2016, researchers at Johns Hopkins published in the British Medical Journal stated their results showed a much higher mortality rate than the IOM’s 1990 study. Medical errors were reported as the 3rd leading cause of death, only behind cancer and heart disease, leading to 250,000 deaths per year (6). These errors are believed to be responsible for 9.5% of all deaths annually. Common causes are inexperienced staff, new procedures, extremes in age, complex or urgent care, poor communication, handwriting, or handoff. Largely, this is due to faulty systems and poorly designed processes vs. poor practices or incompetent practitioners.
In 2001, the Institute of Medicine’s Crossing the Quality Chasm discussed a new vision in how we approach PI. Previous focuses such as safety and error prevention were to expand with the implementation of quality improvement processes and measuring outcomes across the healthcare system (7). Outcomes, which are the results of care from the perspective of patients, providers, and payers, are influenced by society and studies conducted around the world. Often the focus is on morbidity and mortality; but tools can be used to evaluate data such as registries, audits, and surveys.
Evidenced-based medicine is a term that originated in the 1990’s. It is a method of patient care, decision making, and teaching that integrates high-quality research evidence with pathophysiologic reasoning, experience, and patient preference (8). This influence has changed medicine and greatly impacted trauma care as well. Clinicians are now encouraged to base clinical decisions on the best available evidence and understand the influence of the evidence. Thereby, understanding that in their clinical beliefs, a practice that they’ve done for years, may be wrong. This process of evidence-based practice has led to several health care agencies to implement methods that have become standards of care.
There are numerous health care agencies and organizations committed to health care quality. Some of the leading healthcare quality organizations are The Agency for Healthcare Research and Quality (AHRQ), The National Quality Forum (NQF), and the Joint Commission. An example of their integration of best practices and cooperation occurred in the late 2000’s. AHRQ, a government agency formed in 1989, commissioned a study to look at evidence-based best practice guidelines for enteral nutrition, handwashing, venous thromboembolism chemoprophylaxis, analgesia, and nursing staffing. These focus areas led to the NQF publishing 30 new best practice guidelines. The Joint Commission took 11 of the NQF’s guidelines and implemented them into the standards of hospital accreditation (8). This led to such important developments as Rapid Response Teams, medication reconciliation, perioperative antibiotic protocols, and ventilator bundle protocols. Another important organization that has led to breakthrough improvements in safety and quality healthcare is the Leapfrog Group. When founded in 2000, this Fortune 500 business Roundtable-sponsored proposal sought to identify characteristics of high-quality healthcare. Their findings included the use of electronic medical records with physician order entry, the presence of an intensivist in the ICU, and high volume in complex diseases (8).
Trauma center standards
Trauma care and its development have been historically connected by warfare. The Civil War introduced us to the first trauma systems; where a structured network was used to care for the large volumes of casualties. World Wars I and II introduced the use of blood and advanced surgical techniques such as colostomies in penetrating colon injuries. The Korean and Vietnam conflicts saw the advancement of helicopters to expedite care to forward surgical hospitals (9). They also began to understand the fluid shifts into the cell after major hemorrhage and resuscitation. It was those lessons learned from war that led to the development of the first civilian trauma centers at San Francisco General, Shock Trauma in Baltimore, and Cook County in Chicago in 1966. Also, that same year, a landmark paper was published by the National Academy of Sciences/National Research Council. Accidental Death and Disability: The Neglected Disease of Modern Society proposed a categorization of facilities to be based on the institutional capacity to deal with a broad spectrum of emergency conditions (10). When researched in 2000, the number of states with mature trauma systems since 1998 had expanded from 2 to 35.
A study in 2003 showed 83% of Level I and II trauma centers were designated or certified by the State or Region (11). The standards by which trauma centers can be designated by the state vary accordingly state to state. In that cohort, 25% of trauma centers were ACS verified (11). The National Association of State EMS Officials polled 82% of the participating states in a 2016 survey. There, 80% of the state trauma programs were housed in the state’s Health Department. The average staff for these state-based departments was 5, with a lead administrator, general staff, facility designator, data/registry, and epidemiologist. 90% of the states have the legislative authority to designate trauma centers. This study pointed out that 71% of responding states use a combination of state and ACS criteria for trauma center designation (1). As the cost of trauma center verification rises; due to survey costs, required staff, training, etc., there is concern that centers will avoid a formal verification process and have the states designate centers on their own to fulfill that need.
When the ACS’s Resources for Optimal Care of the Injured Patient was first published in 1976, initial updates were every four years. The full publications were referred by the color of the book; with Blue in 1986, then Red [1990], Gold [1999], Green [2006], and the Orange Book in 2014. These standards have been widely embraced and have become the standards for accrediting trauma centers. Yet variability remains state to state, often due to the cost of verifying the capabilities of such centers and other geographic challenges. Trauma center’s effectiveness has been further validated by ongoing research such as the National Study on the Costs and Outcomes of Trauma (NSCOT). This study reviewed care at 18 verified trauma centers and 51 non-trauma centers. When adjusted for age, injury severity, and pre-existing conditions, the overall risk of death was 25 percent lower when care was provided at a trauma center compared to that at a non–trauma center (12).
Another study looked at the outcomes before and after trauma center verification. When they measured a 2-year period before verification and a 4-year period after, there was a 27% decrease in mortality. There was a 19% reduction in length of stay and over a $4,000 per patient savings. Much of the improvement was attributed to the additional staffing required in a verified trauma center, such as the Advanced Practice Providers, administrative staff, and PI initiatives (13).
Chapter 16: the standards for trauma quality
Though earlier Optimal Hospital Resources for Care of the Seriously Injured provided the focus for quality assurance, the level of detail was not provided until its final destination was created in Chapter 16. In 1986’s “Blue Book,” the new standards required the use of a Trauma Registry (14). The first trauma registry was originally started in Illinois in 1971. That registry stored data across the state, but it was bulky and was required to be housed in a mainframe computer system. In 1985, the beginnings of widespread microcomputing use allowed for the proliferation of trauma registries systems (15). Though the Abbreviated Injury Score (AIS) and Injury Severity Score (ISS) were developed in 1969 and 1971 respectively, this new registry standard and new ease of use through computing allowed for the “documentation of severity of injury (by trauma score, age, and ISS) and outcome (survival, length of stay, and ICU length of stay) with monthly review of statistics” (16). The AIS provides the basis for ISS scoring by grading the severity of individual injuries. The ISS is defined as the sum of squares of the highest AIS grade in the three most severely injured body regions (17).
In 1990’s “Red Book,” the organizational structure provided that a designated clinician has the authority, responsibility, and accountability for the assessment and assurance of the quality of care. This 5-page chapter for quality assurance provided formal definitions for the trauma patient and a list of defined audit filters. Many of these filters are in existence today. Although the time intervals have changed; such as >6 hours for transfers out (now 3) and unplanned return to the OR in 48 hours (no current time limits). Also, a list of 35 complications was defined and to be collected in the trauma registry (18). This version also provided additional detail on the use of ISS and Trauma Injury Severity Score (TRISS). These scores were used to measure the severity of injury and predict survivability. With a TRISS below 0.5, this was used as the dividing line of survival probability. For instance, if a trauma death had a TRISS of 0.32, it would translate into a survival probability of 32%; and thereby an expected death. Other charts were also introduced to plot Injury Severity Scores (ISS) and Revised Trauma Scores (RTS). Multidisciplinary meetings were seen as the opportunity to peer review morbidity and mortality cases in a confidential setting. The outcomes of these discussions were to be stored in a secure format. The corrective action for this process included new or policy modifications, education, counseling, and credentialing. The effectiveness of the implemented plan was to be reevaluated.
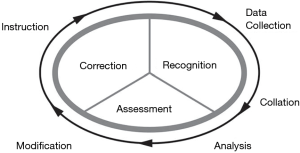
The “Gold Book” in 1999 changed the title from Quality Assurance to PI. It also provided us with such keys terms as “opportunities for improvement” and “loop closure”. Also, the figure of The Continuous Process of Performance Improvement illustrated the cycle of monitoring, assessment, and management (Figure 1). The PI process must have reliable data collection which gathers valid and objective information necessary to identify opportunities for improvement (19). This information is to be reviewed at regular intervals in a multidisciplinary format. Corrective action is to be documented and monitored as the cycle repeats itself. By monitoring this corrective action for the desired effect, the loops may be closed in the individual instance, but yet the loop may never be definitively closed. For instance, implementing changes to the departmental venous thromboembolism protocol may not eliminate all pulmonary embolisms, though with continuous monitoring it can measure if there has been a change or reduction. The concept that improved care also translated into the value of trauma care. The three core components are system of care, morbidity, and outcome. The value equation; where value equals the quality of process and quality of outcome divided by the cost. It was noted that value could be increased through improving quality, outcomes, or by decreasing costs (19). In this version, definitions were also provided for preventable, potentially preventable, and non-preventable events.
The most notable change in 2006’s “Green Book” was incorporating Patient Safety into Performance Improvement. PI in trauma care has been defined as the continuous evaluation of a trauma system and trauma providers through a structured review of the process of care as well as outcome (8). Safety had once been considered a given in medicine, but now recognized something that requires a clear effort. Patient safety is also directed at the environment in which care can be affected (20). Thereby the new acronym PIPS, where PI and Patient Safety (PS) may overlap or have its own distinctive characteristics. The goal is to reduce inappropriate variation in care and to improve patient safety. Also mentioned in this chapter was the aforementioned national Patient Safety Initiates. These initiatives laid the framework for aligning the organizations Patient Safety department and not working in individual silos. 2006 was also the year the National Trauma Data Bank (NTDB) was created and now houses the largest aggregation of trauma registry data ever assembled (15). The Criterion Deficiency (CD) was created to assist in the trauma center verification process. Therefore, centers could be cited on a specifically written standard in which they may be deficient.
The most recent iteration of the Resources for Optimal Care of the Injured Patient was published in 2014 (Figure 2). The “Orange Book” PIPS section is more than twice the size (19 vs. 8 pages) of the “Red Book.” In fact, the overall standard is 63% longer (215 pages) when compared to the 1990 version (18,21). Many of the concepts remain, including the PIPS naming convention, Continuous Process of PI model, Value, and Closing the Loop (Figure 3). Regarding Operational Concepts, the written plan, commonly referred to as a PI Plan, required centers to outline in a formal document the configuration and details of their performance improvement program. This chapter also includes new recommendations for methods to monitor the quality of the program, including the use of evidence-based practiced principles. In order to reduce unnecessary variations in care, clinical practice guidelines, protocols, and algorithms should be used for such conditions or scenarios:
- Massive transfusion protocol;
- Management of severe traumatic brain injury;
- Assessment and clearance of c-spine;
- Venous thromboembolism prophylaxis.
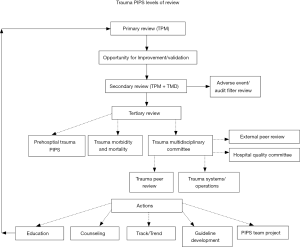
Best practice guidelines for these and others are available online at www.facs.org/quality-programs/trauma/vrc/resources (21). Minimum criteria for full trauma team activation was also included for such conditions as hemodynamic instability, gunshots wounds (all areas minus the head or below the elbow/knee), airway emergencies, blood transfusion, or Emergency Physician discretion. Several other suggestions include evaluating >10% of patients admitted to a non-surgical service, Radiology department performance, and other various performance metrics related to trauma volume and throughput. Over and undertriage had its own CD (Criterion Deficiency), requiring centers to monitor this quarterly result through a suggested Matrix Method. This method is based on a patient’s ISS (Injury Severity Score), and the highest, midlevel, and no level of trauma team activation. Appropriateness is based on the final diagnosis and subsequent Injury Severity Score. When divided between major (ISS ≥15) and minor trauma, this information does not consider patient vital signs or other conditions that would warrant the highest level of activation. Undertriage goals are to be less than 5%. The chapter continues to discuss the importance of the multidisciplinary peer review process and later alludes to using the Joint Commission’s Patient Safety Event Taxonomy. Regarding judgment classification, Chapter 16 states “mutually agreed upon nomenclature to allow for integration with the institution-wide PIPS process should be used” (21).
Trauma nomenclature
Though changes in the ACS’s Resources for Optimal Care of the Injured Patient have dictated the changes in Trauma Performance Improvement, the nomenclature has evolved with the healthcare industry. In the 1980’s, Quality Assurance (QA) was typically retrospective chart review used for looking at the documentation to reflect the quality of physician performance. QA changed to Total Quality (TQM) Management and later evolved to Continuous Quality Management (CQM) (15). These methods were still rooted in that the majority of defects in care results from failures of the system rather than the individuals themselves. Ultimately, the term PI evolved; defined as a continuous, multidisciplinary effort to measure, evaluate, and improve the process of care and its outcome (8).
In 1990, James Reason proposed the Swiss cheese model of causation. This risk analysis tool has been found to be applicable in industries such as aviation, engineering, and healthcare. He theorized there are four domains where accidents can occur: supervision, organizational influences, preconditions, and special acts. Organizational policies are represented as slices of cheese and holes are considered weaknesses. A “trajectory of accident opportunity” occurs when all of the holes line up with each slice of cheese; thereby leading to failures (22). As noted in the IOM’s To Err is Human, that humans are imperfect and error can be expected (5). Countermeasures need to be designed to build system or institutional defense and avoid these traps that can lead to failure. In this system approach, it is understood that bad things can happen to good people.
Beginning in January 2012, American College of Surgeons’ Committee on Trauma (ACS COT) had changed the nomenclature for deaths’ judgment categories. The old system included terminology as preventable, potentially preventable, and non-preventable. In a large, 6-year study at a mature Level 1 Trauma center, 2.4% of all trauma deaths were classified as being preventable or potentially preventable (23). This approach, however, does not ensure that performance is improved as much as it tends to focus on the attribution of blame. Though most states have a protected peer review process, some states have opened the peer review process to discoverability; thereby limiting judgment status (24). Also, in a growing elderly trauma population, teaching and opportunities for improvement may have been missed when patients and families chose a less aggressive plan of treatment (25). The new classification is now Unanticipated Mortality with Opportunity for Improvement, Anticipated Mortality with Opportunity for Improvement, and Mortality without Opportunity for Improvement (26).
In 2003, the Society of Trauma Nurses began offering TOPIC, the Trauma Outcomes and Performance Improvement Course. This one-day modular format teaches participants the definitions, processes, and tools needed to have a successful performance improvement program. Interactive vignettes are used to provide hands-on skills in navigating the PI process. The program was updated in 2012 to use the Joint Commission’s Patients Safety Event Taxonomy (PSET). This initial foray was the introduction for trauma centers to use a systematic approach in critically evaluating quality care and patient safety events. Though we will go into deeper analysis later in this paper, centers were encouraged to classify each event into the five groups (Impact, Type, Domain, Cause, and Prevention and Mitigation) within their corresponding subgroups.
The Pennsylvania experience
Pennsylvania has been at the forefront of our nation’s trauma system development efforts and is considered a role model for its robust trauma registry and statewide performance improvement structure. In the early 1980’s, several healthcare organizations, such as Pennsylvania’s Medical Society and Hospital and Healthsystem Association of Pennsylvania, lobbied the state legislature to create the Emergency Medical Service Act (Act 45). Signed into law in July 1985, this new law recognized the Pennsylvania Trauma Systems Foundation (PTSF) as the accrediting body for all Pennsylvania trauma centers. The Act dictates that PTSF align its standards of accreditation “at a minimum” with the American College of Surgeons but historically has exceeded the ACS in areas such as staffing and education.
By the mid-1990’s, there were over 20 accredited Level I and II trauma centers. The PTSF began organizing several state-wide committees staffed by trauma center volunteers throughout the state. In 1996, the Outcomes Committee was formed with one of their goals being to develop a database for use by every trauma center which would identify factors that impact outcomes and provide a standardized format for reviewing trauma care. Working with Digital Innovation Inc., the developer of the Collector© Trauma Registry Database, beta testing began in 2000. The new product was called POPIMS©, (Pennsylvania Outcomes and Performance Management System) with the goal of creating an interface with the Collector (Trauma Registry) which would allow for easy downloading of patient complications and demographic information. When implemented in 2001, the final product exceeded its initial goals and additionally acted as a standardized way for site surveyors to review Performance Improvement efforts during medical record review during the Accreditation survey. Future goals were to create a central PI repository which would serve to identify statewide trends in care and guide statewide education to improve patient outcomes.
In 2006, the Outcomes Committee held a meeting to assess inter-rater reliability in how POPIMS was being utilized. The data entered into POPIMS was to reflect how trauma centers reviewed their cases at peer-review conferences, judgments made, and how the information was entered. All trauma centers in the state were instructed to submit three cases (preventable, potentially preventable, and non-preventable). Twenty-eight trauma surgeons reviewed thirty-four blinded cases, with each having a minimum of 10 reviews, resulting in 314 reviewer classifications. The meeting had marked the first time a statewide PI reporting system had been used to share outcomes between trauma centers. Concluding, there were significant differences in Institutional classification and reviewer classification (27). Recommendations were to have standardized data submission and the ability to have risk-adjusted data to allow for better trauma center comparison. This paper would become the forerunner of recommendations that would be later echoed by the Joint Commission’s PSET and the ACS’s Trauma Quality Improvement Program (TQIP).
An Ad Hoc Committee was subsequently formed, and the group aimed to standardize input and assessment in the POPIMS Software. Significant headway was made by standardizing the terminology outside of ACS typical complications and audit filters. These “Opportunities for Improvement” included such problems as delays in care, Blood Bank, Nursing, and Resuscitation Issues. Many software design changes were made in collaboration with Digital Innovation, Inc. including software Narratives and templates to assist Trauma PI staff in formulating M&M or peer-review meeting agenda. A manual was created to guide trauma centers on where and how data is to be entered; as well as guides to morbidity and mortality judgment classification (28). By 2013, state trauma centers began to submit de-identified mortality data with the goal of providing education and policy when trended deviations were recognized. In 2015, the PTSF had hired a designated Manager of Trauma Performance Improvement and revised the trauma center accreditation standard requiring one Full-Time Employee (FTE) for Performance Improvement and Patient Safety. Suggestions were made to have additional staff (0.5 FTE for every 500–750 trauma contacts over the initial 1,000) based on the volume and also required TOPIC within one year of hire (29). In that same year, the Cribari Grid was implemented into POPIMS for over/under triage analysis. In 2016, Pennsylvania joined 1 of 5 statewide TQIP collaboratives. Joint Taxonomy was also integrated for all deaths in the POPIMS Software. As of 2018, the evolution continues with the integration of Taxonomy in the new Outcomes software. Analysis continues on the Central Site data, and the PA Collaborative is investigating outliers in the statewide TQIP reports with increased sharing of best practices.
Joint Commission Patient Safety Event Taxonomy
The Institute of Medicine’s reports have had a profound impact on outcomes, including the language we use to discuss care complications. The IOM’s To Err is Human, Building a Safer Health System in 1991 called for a common language that practitioners, providers, and patients can speak and understand (29). While some progress had been made, it wasn’t until the IOM’s 2003 report, Patient Safety: Achieving a New Standard of Care, recommended standardization and better management of information on patient safety (30). Including adverse events and near misses, this new strategy aimed at reducing preventable medical incidents. These studies led to the Patient Safety and Quality Improvement Act of 2005 (29). This act set into motion healthcare agencies to create taxonomy; a concept that combines terminology and the science of classification.
By 2005, the Joint Commission had created the Patient Safety Event Taxonomy (PSET). Over 500 articles were initially researched, but only 23 were found to be useful in regards to classifying medical events, errors, and reporting systems for homogeneity. Then, the Joint Commission’s Sentinel Event Program was analyzed for seven years to validate the preliminary taxonomy (31). As a result, PSET was born by using five primary root nodes or classifications, 21 sub-classifications, and 527 unique references (24). The five main nodes include: Impact—outcome or effect of the medical error, Type—implied or visible processes that failed, Domain—setting and individuals involved, Cause—Factors that led to the incident, and Prevention/Mitigation—measures to reduce the incidence and effects of adverse occurrences. When broadly applied, classifying incidents in this matter will determine the quality of incident reports, the effectiveness of the reporting system, and the success of the intervention strategies (31).
PSET was released in 2006 and was endorsed by the National Quality Forum (NQF). The NQF’s president and CEO at the time stated it was a “good first step” but had acknowledged that “frankly, needs a lot of work” (32). PSET laid the foundation for other taxonomy’s such as International Classification for Patient Safety (ICPS), by the World Health Organization. It has been difficult for a single taxonomy to gain traction as each state may use their own reporting systems. Commercial, software vendor taxonomies have experienced an outgrowth due to organizations desire to optimize services and collect information in a consistent format (30). The advances in technology and software have allowed increased flexibility to modify taxonomy based on the customer’s needs.
There are several keys concepts necessary for a successful taxonomy. There must be usability, whereas methods are easily understood. Different users should be able to use the approach and classify events in the same way. There should also be a means to capture the context and texture of the story. Otherwise, key points may be missed. The change must also be cost-effective and offer something new from the previous system (30).
In an analysis of six international articles that utilized the PSET, there are remarkable similarities. All but the Spanish article (33) used a retrospective review of previously reviewed charts to determine judgment status using the old nomenclature—of preventable or potentially preventable deaths. While the range of potentially preventable deaths at trauma centers can range from 2% to 22% (33), these studies had an average of 10.2% of preventable and potentially preventable deaths. The American, Spanish and French studies showed the error Type to be from Clinical Performance, Communication, and Clinical Management (33-36). An American and United Kingdom (UK) center noted errors in treatment and assessment (37,38). The most frequent Domain was the ED during the resuscitation phase, except the French study noted errors in Pre-Hospital care (36). Overwhelmingly, the Causes were human error (34-36), citing Rule and Skill-based errors (33). The UK noted these were mostly errors in omission, the failure to act when necessary. Mitigation and prevention were addressed in an American and the Spanish article, where the errors were frequently Universal (33,35). However, care must be made to differentiate the definitions between mitigation and prevention, as they are not always mutually exclusive. Prevention is often the focus and mitigation may be difficult to gauge and assess. They had also noticed a bias in judgment with more complex patients, and only 23% of the errors had been concurrently addressed in M&M type meetings (37). All of these articles went on to further analyze the errors in a level of detail not captured in PSET; such as delays in the OR, unstable patient in CT, issues with hemorrhage control, and airway management. One of the American studies had raised the question of whether PSET’s limitations are due to the complexity limiting it to be useful (34). One of the American study’s noted the Hawthorne-type effect of enhanced awareness might also contribute to a reduction in errors (38).
Trauma Quality Improvement Program
In 1987, the U.S. Congress required the Veterans Health Administration (VHA) to report outcomes of major surgery as per national averages and risk-adjusted for the patient’s illness. The new mandate led to the implementation of the National Surgical Quality Improvement Program (NSQIP) in 1994. This first of its kind system allowed for continuous quality improvement and comparative analysis. While available through the ACS since 2004, NSQIP showed a 27% reduction in mortality (39). The ACS COT looked to this model to establish risk-adjusted analysis of trauma mortality, comorbidities, and injury cohorts. When used with the NTDB, these semiannual reports with box decile graphs were designed to provide trauma centers feedback on their performance and benchmark against national standards. Launched in 2006 (40) and mandated by the ACS COT 2017 (21), this has provided trauma centers the data to implement necessary changes to improve patient outcomes. This has also led to a renewed focus on data quality to ensure accurate reports; as centers drill down on their data for each report. The organization now has over 800 trauma centers and has annual meetings where PI initiatives and Best Practice Guidelines are presented. Massive Transfusion Protocol, Geriatric Trauma, and Management of Traumatic Brain Injury are some of the new tool’s centers are using to implement care based on evidence-based practices (Figure 4) (41).
Zero preventable deaths after injury
There has been considerable discussion about whether the approach towards patient safety acknowledges that certain errors are unavoidable. Rather, should a concept like the Swedish have used; that aim for a total reduction in road traffic crashes (34). In 2016, a report was presented from both military and civilian sectors in order to create a national trauma system. In A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury, it points out that we are achieving our highest level of trauma care on the battlefield yet civilian care is dependent upon where and when the injury occurs (42). With these gaps, preventable deaths and disability are due to these inconsistencies and a lack of consolidated leadership. In a proposed national trauma system, the care would be grounded in sound learning principals from the time of injury, acute care, rehabilitation, and beyond. Looking to leadership from the White House, a standardization of policy integration, data collection, and infrastructure support could lead to an enhanced performance improvement method that can innovate best practices. Similarly, but outside the trauma, the Patient Safety Movement Foundation has vowed to reach zero preventable deaths by 2020. During their 2016 summit and beyond, they will strive to unify health ecosystems, promote quality and safety transparency, and identify the challenges that are killing patients to create actionable solutions (43) (Figure 5).
Summary
Quality has become paramount in healthcare; from saving lives, impacting the hospital’s bottom line, to being the difference in trauma center verification or accreditation. Performance Improvement will continue to evolve from the realization of quality data abstraction and collection. From reports and thorough collaborative efforts such as TQIP, they will continue to evolve our best practices. It is anticipated there will be better issue related inter-rater reliability with the “Traumafication” of the Taxonomy by members of the ACS COT and Society of Trauma Nurses (24). Also, the ACS COT will also provide Clarification Documents, that allow the trauma standards to be modified in a shorter time cycle than have been previously published. Through our evolution of trauma care, we have learned to err is human. It is now contingent upon us to learn and act upon this information.
Acknowledgements
The author would like to acknowledge the contributions of Juliet Altenburg, MSN, RN, Executive Director of the Pennsylvania Trauma Systems Foundation, in the review and editing of portions of this article specific to PTSF.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- National Association of State EMS Officials. Status of State Trauma System Planning and Development: Utilization of the HRSA Model Trauma Systems Planning and Evaluation Document. September 2016.
- American College of Surgeons. Available online: https://www.facs.org/quality-programs/trauma/atls/about, accessed October, 2018.
- Optimal hospital resources for care of the seriously injured. Bull Am Coll Surg 1976;61:15-22. [PubMed]
- Hospital and prehospital resources for optimal care of the injured patient. Committee on Trauma of the American College of Surgeons. Bull Am Coll Surg 1986;71:4-23. [PubMed]
- Institute of Medicine. To Err is Human: Building a Safer Health System. Washington, DC: Institute of Medicine, 1999.
- Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ 2016;353:i2139. [Crossref] [PubMed]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21 Century. Washington, DC: Institute of Medicine, 2001.
- Feliciano D, Mattox K, Moore E. Trauma Outcomes” Trauma, 6th Edition. New York City, NY: McGraw-Hill Professional, 2007.
- Trunkey DD. History and development of trauma care in the United States. Clin Orthop Relat Res 2000.36-46. [Crossref] [PubMed]
- Hospital Resources for Optimal Care of the Injured Patient. Committee on Trauma of American College of Surgeons. Bull Am Coll Surg 1979;64:43-8. [PubMed]
- MacKenzie EJ, Hoyt DB, Sacra JC, et al. National Inventory of Hospital Trauma Centers. JAMA 2003;289:1515-22. [Crossref] [PubMed]
- MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A National Evaluation of the Effect of Trauma-Center Care on Mortality. N Engl J Med 2006;354:366-78. [Crossref] [PubMed]
- DiRusso S, Holly C, Kamath R, et al. Preparation and Achievement of American College of Surgeons Level I Trauma Verification Raises Hospital Performance and Improves Patient Outcome. J Trauma 2001;51:294-9; discussion 299-300. [Crossref] [PubMed]
- American College of Surgeons. Resources for Optimal Care of the Injured Patient. 1986.
- Nwomeh BC, Lowell W, Kable R, et al. History and development of trauma registry: lessons from developed to developing countries. World J Emerg Surg 2006;1:32. [Crossref] [PubMed]
- Baker SP, O'Neill B, Haddon W, et al. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974;14:187-96. [Crossref] [PubMed]
- Pohlman T, Bjerke H, et al. Trauma Scoring Systems. May 2014. Available online: https://emedicine.medscape.com/article/434076-overview, accessed October 2018.
- American College of Surgeons. Resources for Optimal Care of the Injured Patient. Chicago, 1990.
- Committee on Trauma American College of Surgeons. Resources for Optimal Care of the Injured Patient. Chicago, 1997.
- Committee on Trauma American College of Surgeons. Resources for Optimal Care Of the Injured Patient. Chicago, 2006.
- Committee on Trauma American College of Surgeons. Resources for Optimal Care of the Injured Patient. Chicago, 2014.
- James R. The Contribution of Latent Human Failures to the Breakdown of Complex Systems. Philosophical Transactions of the Royal Society of London. April 1990; Series B, Biological Sciences.
- Tiexeria P, Inaba K, Hadjizacharia P, et al. Preventable or Potentially Preventable Mortality at a Mature Trauma Center. J Trauma 2007;63:1338-46; discussion 1346-7. [Crossref] [PubMed]
- Reed R. Joint Commission Taxonomy Implementation for Trauma Performance Improvement. Available online: https://www.facs.org/~/media/files/quality%20programs/trauma/vrc%20resources/12_ofi%20jacho%20taxonomy%20implementation%20for%20trauma%20performance%20improvement.ashx, accessed October 2018.
- McGonigal M. Trauma Mortality: The New Nomenclature. Available online: https://thetraumapro.com/2012/07/05/trauma-mortality-the-new-nomenclature/, accessed October 2018.
- American College of Surgeons. Available online: http://www.facs.org/trauma/vcnews.html, accessed February 2011.
- Pasquale MD, Peitzman AB. Pennsylvania Trauma Systems Foundation Outcomes Committee. Preventability Classification in Mortality Cases: A Reliability study. J Trauma 2009;67:1097-102. [Crossref] [PubMed]
- Pennsylvania Trauma Systems Foundation. 2017 POPIMS Operations Manual. Available online: http://ptsf.org/upload/POPIMS_Manual_2017_-_Final.pdf, accessed October 2018.
- Pennsylvania Trauma Systems Foundation. Adult Level 1, 2, & 3 Standards of Accreditation Version 08.01.2018. Available online: http://digital.graphcompubs.com/publication, accessed October 2018.
- Simmons S. American Society for Healthcare Risk Management Data for Safety Taxonomy Task Force. Tackling patient safety taxonomy: A must for risk managers. J Healthc Risk Manag 2008;28:7-17. [Crossref] [PubMed]
- Chang A, Schyve P, Croteau R, et al. The JCAHO patient safety event taxonomy: a standardization of terminology and classification schema for near misses and adverse events. Int J Qual Health Care 2005;17:95-105. [Crossref] [PubMed]
- NQF endorses patient safety event taxonomy. Healthcare Benchmarks Qual Improv 2005;12:113-5. [PubMed]
- Montmany S., Pallisera A, Rebasa P, et al. Preventable deaths and potentially preventable deaths. What are our errors? Injury 2016;47:669-73. [Crossref] [PubMed]
- Ivatury RR, Guilford K, Malhotra AK, et al. Patient Safety in Trauma: Maximal Impact Management Errors at a Level I Trauma Center. J Trauma 2008;64:265-70; discussion 270-2. [Crossref] [PubMed]
- Vioque SM, Kim PK, McMaster J, et al. Classifying errors in preventable and potentially preventable trauma deaths: a 9-year review using the Joint Commission’s standardized methodology. Am J Surg 2014;208:187-94. [Crossref] [PubMed]
- Girard E, Jegousso Q, Boussat B, et al. Preventable deaths in a French regional trauma system: A six-year analysis of severe trauma mortality. Journal of Visceral Surgery 2018. (In Press). Available online: https://doi.org/. [Crossref]
- Pucher PH, Aggarwal R, Twaij A, et al. Identifying and Addressing Preventable Process Errors in Trauma Care. World J Surg 2013;37:752-8. [Crossref] [PubMed]
- Gruen RL, Jurkovich G, McIntyre L, et al. Patterns of Errors Contributing to Trauma Mortality: Lessons Learned from 2,594 Deaths. Ann Surg 2006;244:371-80. [PubMed]
- Pasquale MD. Outcomes for Trauma: Is There an End (Result) in Sight? J Trauma 2008;64:60-5. [Crossref] [PubMed]
- Shafi S, Nathens A, Cryer H, et al. The Trauma Quality Improvement Program of the American College of Surgeons Committee on Trauma. J Am Coll Surg 2009;209:521-530.e1. [Crossref] [PubMed]
- Trauma Quality Improvement Program (TQIP). Available online: https://www.facs.org/quality-programs/trauma/tqp/center-programs/tqip, accessed October 2018.
- National Academies of Sciences, Engineering, and Medicine. A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. Washington, DC: The National Academies Press, 2016.
- Patient Safety Movement Foundation. Available online: https://patientsafetymovement.org/, accessed October 2018.
Cite this article as: Mowry M. The evolution of trauma performance improvement. J Emerg Crit Care Med 2019;3:6.


