
A severe case of acute respiratory distress syndrome (ARDS) in a primigravida recently diagnosed with acute myeloid leukemia (AML)
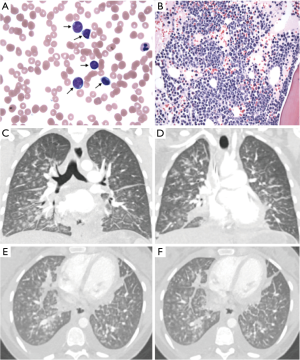
The incidence of leukemia during gestation ranges from 1 in 75,000 to 1 in 100,000. We report a rare case of acute respiratory distress syndrome (ARDS) in a 30-year-old second trimester primigravida diagnosed with acute myeloid leukemia (AML) upon hospital admission (Figure 1A,B).
The patient presented with frontal headache, subconjunctival hemorrhage, and palatal petechiae, with laboratory results showing leukocytosis, anemia, and thrombocytopenia. She underwent induction chemotherapy consisting of cytarabine and daunorubicin.
One day later, the patient became febrile, tachypneic, and hypoxic. Chest X-ray showed interstitial and alveolar edema. Two days post-induction, chest X-ray showed significant worsening of airspace disease with superimposed nodular opacification due to underlying edema, diffuse alveolar hemorrhage, or pneumonia; CT showed diffuse ground glass opacities (Figure 1C,D,E,F). She was transferred to the MICU, where she was intubated, started on inhaled vasodilators, vasopressors, steroids, and broad spectrum antibiotics.
On day 4, the patient had a P/F ratio of 73, indicating severe ARDS. She underwent low tidal volume ventilation, reaching a maximum of 16 cmH2O PEEP and 100% FiO2. She was treated with neuromuscular blockade for ventilator dyssynchrony and underwent prone positioning. The likely source of her ARDS was noninfectious—either intrapulmonary tumor lysis syndrome or transfusion associated lung injury.
On day 5, the patient developed acute renal failure requiring continuous veno-venous hemofiltration, and subsequently, had premature rupture of membranes; fetal demise was confirmed by bedside ultrasound. On day 6 of chemotherapy, labor was induced with mifepristone, and a male fetus of 23 weeks was delivered vaginally. The following day, she was found to have fixed and dilated pupils, and fulfilled criteria for brain death.
This case highlights the challenges of induction chemotherapy in patients with leukemia during pregnancy.
Acknowledgements
Study was funded by the Brigham and Women’s Hospital Critical Care Research Collaborative and Consortium (BCCRCC).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Under our local IRB policy, this case report was exempt from review. And since the information presented in this case report are de-identified, there was no need for obtaining written informed consent per our local IRB policy.
Cite this article as: Joshi S, Gandee Z, Baron RM, Hou PC. A severe case of acute respiratory distress syndrome (ARDS) in a primigravida recently diagnosed with acute myeloid leukemia (AML). J Emerg Crit Care Med 2018;2:92.


