
Recurrent vertebrobasilar insufficiency—bow hunter’s syndrome
Introduction
Bow hunter’s syndrome or rotational vertebrobasilar insufficiency syndrome was first described by Sorensen in 1978 in a patient who developed lateral medullary syndrome during archery practice (1). The rarity of this condition is exemplified by the fact that it has been described in the form of case reports and few case series. Jost and Dailey as well as Rastogi et al. have carried out systematic review of literature providing information regarding the characteristics of this condition (2,3).
The paired vertebral arteries are the first and largest branches of the subclavian arteries. They ascend through the transverse processes of the upper six cervical vertebrae, pass behind the lateral masses of the atlas, enter the dura mater behind the occipital condyles. It winds behind the superior articular process of the atlas and enters the cranium through the foramen magnum where it unites with the opposite vertebral artery to form the basilar artery (at the lower border of the pons) (4). This course through soft tissue and bony canal subjects the artery to strain caused by neck movements.
Bow hunter’s syndrome is a clinical manifestation arising due to dynamic compression of vertebral arteries during extension and rotational neck movement. The underlying pathology is usually a herniated disc, degenerative conditions such as spondylosis, an osteophyte or thickened ligament (5-9). At the level of atlantoaxial joint, the lesion may be caused by an ossified or thickened atlanto-occipital membrane, a dural fold in the foramen magnum, occipitalised atlas, an accessory ossicle behind the atlanto-odontoid junction, erosive rheumatoid arthritis of C1-C2 or C1-C2 facet hypertrophy (10-14). At the subaxial level compression is caused by a bony spur or herniated disc (15).
The underlying pathogenesis is due to endothelial damage by repetitive shear stress or stasis of blood leading to increased propensity for thromboembolism (16).
Case presentation
A 52-year-old male patient presented to emergency department with complaint of sudden onset giddiness, nausea, vomiting, slurring of speech and imbalance of gait. On examination, he was conscious and vitals were normal. His higher mental functions like attention, executive function, judgement, language and praxis did not show any impairment. He had dysarthria and right sided gaze evoked nystagmus. Examinations of cranial nerves did not show any deficit. Motor system examination was normal. There was no sensory deficit. He had intention tremor and impaired finger—nose test in right upper limb. Gait was severely ataxic with tendency to fall on either side. There was no history of headache, trauma to head, fever, loss of consciousness, neck pain or seizure.
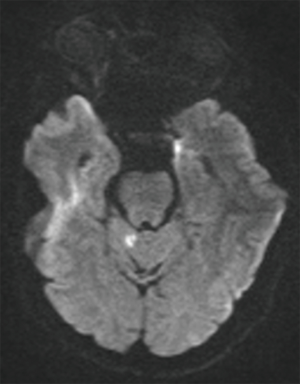
Magnetic resonance imaging (MRI) brain showed diffusion restriction in right cerebellar vermis suggestive of acute infarction (Figure 1). There were foci of gliosis in left cerebellar hemisphere (Figure 2). He was diagnosed as a case of ischemic stroke involving posterior circulation and treated with oral antiplatelet and statin. He was advised gait training exercises and rehabilitation for ataxia. Magnetic resonance angiography of neck and brain vessels did not show any vessel stenosis. He was evaluated for cardiac causes of stroke. Thrombophilia work up was negative.
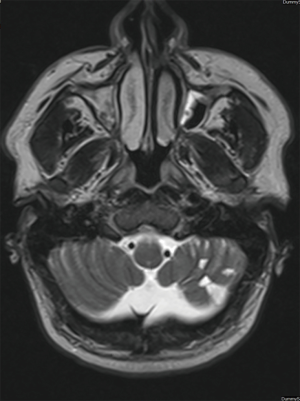
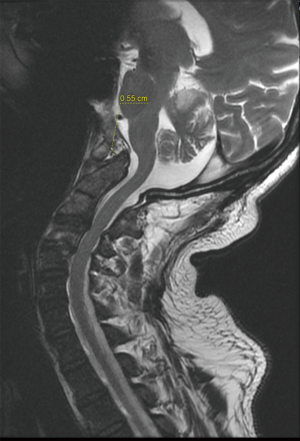
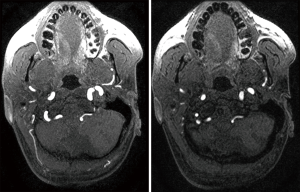
In view of chronic left cerebellar infarcts evident on MRI, the case history was reviewed with the patient. He described intermittent episodes of dizziness and nausea which were self-limiting. He was unclear on the factors that had precipitated these symptoms. Review of MRI images showed presence of craniovertebral junction anomaly with occipitalised atlas and mild basilar invagination indenting the cervicomedullary junction (Figures 3 and 4).
Dynamic magnetic resonance angiography was done which showed compressive occlusion of right vertebral artery on extending the neck (Figure 5).
After review of case history, a diagnosis of vertebrobasilar insufficiency (bow hunter’s syndrome) was made. Neurosurgical opinion was obtained. The potential risk of recurrent posterior circulation stroke was discussed with the patient in detail. He was provided information and counseling regarding the available treatment modalities. He chose to be on conservative management and deferred any kind of intervention at present.
Discussion
Jost and Dailey reviewed 128 patients of bow hunter syndrome and determined that the occlusion was subaxial (between C3 and C7) in 58% cases, 36% at C1-C2 level and in 6% cases proximal to C7 and distal to C1. The mean age at presentation was 58±11 year with male predominance (54% vs. 46%) (2). According to review by Rastogi et al., the mean age at presentation was 53 years and the level of the atlantoaxial (C1-C2) joint was most commonly involved (99/142) (3). In our case, the dynamic compression was at the level of atlantoaxial joint and symptoms were precipitated with neck extension.
In these had dominant vertebral artery compression at the atlantoaxial or subaxial level with the non-dominant vessel being hypoplastic, stenotic or occlusive by arteriosclerosis. The posterior communicating arteries are generally hypoplastic or aplastic leading to poor communication with circle of Willis and inadequate collateral blood flow from anterior circulation.
Husni and Storer reported 23 patients with vertebrobasilar insufficiency induced by the rotational occlusion of one vertebral artery with the opposite artery being hypoplastic or absent in 22 patients and narrowed at its origin in 1 patient (17).
Repeated sheering forces and compression by external compression like that by a bony spur can lead to intimal and/or medial tear and increased platelet aggregation. Arterial dissection and thrombus formation are prominent causes of artery to artery embolism leading to this syndrome (18,19). There was no evidence of dissection or thrombosis in our patient.
Clinical manifestation consists of a spectrum ranging from transient ischemic attacks (TIA) to posterior circulation stroke. Symptoms can be repeatedly precipitated by rotation or extension of the head and neck and resolve immediately as the head returns to a neutral position. The classic presentations of this syndrome were summarized by Velat et al. include dizziness, vertigo, nystagmus, nausea with associated emesis, Horner’s syndrome, syncope, and motor or sensory deficits that occur with head rotation (15).
Diagnostic evaluation includes computed tomography (CT) and MRI to visualize the bony and soft tissue structures leading to vascular compression. CT angiography/MR angiography sequences are required to characterize the vascular occlusion. The gold standard diagnostic test is digital subtraction angiography (DSA). It evaluates vessel patency in neutral and in the rotated position and thus supplements diagnosis, localization and planning of treatment (20).
There are still no standard treatment options for bow hunter syndrome owing to the rarity of this condition (16). In their study, Choi et al. analyzed the outcome of patients diagnosed with dynamic compression of vertebral artery and managed with conservative measures. The median follow-up period was 37.5 months with 2 patients out of 21 treated with surgical fusion of C1-C2 vertebrae (21). The remaining 19 patients did not show any fresh deficit during the period of follow up. This study led to conclusion that conservative treatment protocol might be safe and might be considered as a first-line treatment modality. In other studies patients who were treated conservatively with medication may require surgery because of repeated, aggravated symptoms (22).
Surgical treatments, often involving surgical decompression of the VA or C1-C2 fusion, were performed in the majority of cases resulting from abnormal bony structures, disc herniation, instability of the joint and others. in the setting of contralateral VA stenosis, angioplasty with or without stent placement of the stenotic portion will provide a sufficient effect (23).
Conclusions
Recurrent vertebrobasilar insufficiency or bow hunter’s syndrome presents with recurrent symptoms like vertigo, tinnitus and imbalance. Many cases are treated as inner ear disease. Though the incidence of this condition is rare, it can potentially cause infarction and irreversible brain injury. Possibility of this condition should be considered in patients with recurrent symptoms of posterior circulation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: We confirm that a written informed consent was taken from the patient for publication of this case report and images.
References
- Sorensen BF. Bow hunter’s stroke. Neurosurgery 1978;2:259-61. [Crossref] [PubMed]
- Jost GF, Dailey AT. Bow hunter’s syndrome revisited: 2 new cases and literature review of 124 cases. Neurosurg Focus 2015;38. [Crossref] [PubMed]
- Rastogi V, Rawls A, Moore O, et al. Rare etiology of bow hunter’s syndrome and systematic review of literature. J Vasc Interv Neurol 2015;8:7-16. [PubMed]
- Standring S. Gray's Anatomy: The Anatomical Basis of Clinical Practice, Expert Consult - Online and Print 40th Edition. Churchill Livingstone, 2008;78:688-91.
- Zaidi HA. Diagnosis and management of bow hunter’s syndrome: 15-year experience at barrow neurological institute. World Neurosurg 2014;82:733-8. [Crossref] [PubMed]
- Ding D, Mehta GU, Medel R, et al. Utility of intraoperative angiography during subaxial foramen transversarium decompression for bow hunter’s syndrome. Interv Neuroradiol 2013;19:240-4. [Crossref] [PubMed]
- Thomas B, Barreau X, Pointillart V, et al. Endovascular embolization of a nondominant vertebral artery compressed by an osteophyte to prevent recurrence of vertebrobasilar infarctions. J Stroke Cerebrovasc Dis 2015;24:e257-9. [Crossref] [PubMed]
- Healy AT, Lee BS, Walsh K, et al. Bow hunter’s syndrome secondary to bilateral dynamic vertebral artery compression. J Clin Neurosci 2015;22:209-12. [Crossref] [PubMed]
- Sarkar J, Wolfe SQ, Ching BH, et al. Bow hunter’s syndrome causing vertebrobasilar insufficiency in a young man with neck muscle hypertrophy. Ann Vasc Surg 2014;28:1032.e1-10. [Crossref] [PubMed]
- Sakai K, Tsutsui T. Bow hunter’s stroke associated with atlantooccipital assimilation - case report. Neurol Med Chir (Tokyo) 1999;39:696-700. [Crossref] [PubMed]
- Akar Z, Kafadar AM, Tanriover N, et al. Rotational compression of the vertebral artery at the point of dural penetration. Case report. J Neurosurg 2000;93:300-3. [PubMed]
- Puca A, Scogna A, Rollo M. Craniovertebral junction malformation and rotational occlusion of the vertebral artery. Br J Neurosurg 2000;14:361-4. [Crossref] [PubMed]
- Robinson BP, Seeger JF, Zak SM. Rheumatoid arthritis and positional vertebrobasilar insufficiency. Case report. J Neurosurg 1986;65:111-4. [Crossref] [PubMed]
- Chough CK, Cheng BC, Welch WC, et al. Bow hunter’s stroke caused by a severe facet hypertrophy of C1-2. J Korean Neurosurg Soc 2010;47:134-6. [Crossref] [PubMed]
- Velat GJ, Reavey-Cantwell JF, Ulm AJ, et al. Intraoperative dynamic angiography to detect resolution of bow hunter’s syndrome: technical case report. Surg Neurol 2006;66:420-3. [Crossref] [PubMed]
- Cornelius JF, George B, N’dri OD, et al. Bow-hunter’s syndrome caused by dynamic vertebral artery stenosis at the cranio-cervical junction - a management algorithm based on a systematic review and a clinical series. Neurosurg Rev 2012;35:127-35. [Crossref] [PubMed]
- Husni EA, Storer J. The syndrome of mechanical occlusion of the vertebral artery: further observations. Angiology 1967;18:106-16. [Crossref] [PubMed]
- Anene-Maidoh TI, Vega RA, Fautheree GL, et al. An unusual case of pediatric bow hunter’s stroke. Surg Neurol Int 2013;4:148. [Crossref] [PubMed]
- Kawasaki T, Dewerchin M, Lijnen HR, et al. Mouse carotid artery ligation induces platelet-leukocyte-dependent luminal fibrin, required for neointima development. Circ Res 2001;88:159-66. [Crossref] [PubMed]
- Kuether TA, Nesbit GM, Clark WM, et al. Rotational vertebral artery occlusion: a mechanism of vertebrobasilar insufficiency. Neurosurgery 1997;41:427-32. [Crossref] [PubMed]
- Choi KD, Choi JH, Kim JS, et al. Rotational vertebral artery occlusion: mechanisms and long-term outcome. Stroke 2013;44:1817-24. [Crossref] [PubMed]
- Go G, Hwang SH, Park IS, et al. Rotational vertebral artery compression: bow hunter’s syndrome. J Korean Neurosurg Soc 2013;54:243-5. [Crossref] [PubMed]
- Sugiu K, Agari T, Tokunaga K, et al. Endovascular treatment for bow hunter’s syndrome: case report. Minim Invasive Neurosurg 2009;52:193-5. [Crossref] [PubMed]
Cite this article as: Trivedi T, Reddi R, Kumar A, Agarwal B. Recurrent vertebrobasilar insufficiency—bow hunter’s syndrome. J Emerg Crit Care Med 2018;2:65.



