
Ocular parasitosis in the emergency room
A 47-year-old Caucasian male came up in the emergency room with severe itch, burning sensation, redness and irritation of the right eye (Figure 1A). Three weeks before he had a swelling in the sub-mandibular region, some five days later the swelling migrated toward the right zygomatic area and thereafter in the right eyebrow. The ophthalmic examination was performed under topical anesthesia and a moving nematode was extracted following a small incision of the perilimbal bulbar conjunctiva. The worm was sent for further microbiological examination and microscopy, and was found to pertain to the genus of Dirofilaria (Figure 1B).
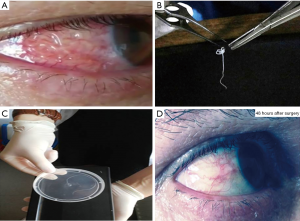
Albania and the Mediterranean area are considered as endemic for the Dirofilaria, with canines and other domestic pets being more frequently infested as previously thought (Figure 1C). In our experience, these are more common in patients living in rural areas, where the sanitary conditions are generally unsatisfactory. For a clinician, it is important to consider the probability of nematodes infesting the ocular structures when foreign bodies are expected and a differential diagnosis is needed, although the course is generally a benign one with complete healing (Figure 1D). The infectious disorders specialist will decide if further antiparasitic drug therapy is needed.
Parasites can attack the anterior ocular chamber and need urgent intervention, since severe itch and irritation will provoke further injuries to the ocular structures. Helminths (round worms or nematodes, such as in our case with Dirofilaria, but with Onchocerca and Toxocara canis being probable as well) are not the only parasites that might affect the ocular structures. Protozoas (mainly amoebas, Giardia, plasmodia, Leishmania); flat worms (Cysticercus, Echinococcus) as well as ectoparasites (ticks) can be present and induce serious challenges to the treating clinician: hence the great importance of a prompt and reliable microbiological identification.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Consent was obtained for the use of information and images. The patient’s identity has been kept confidential.
Cite this article as: Bulica E, Sinamati A, Vyshka G. Ocular parasitosis in the emergency room. J Emerg Crit Care Med 2018;2:58.


