
An anti-human immunodeficiency virus-negative pregnant woman was diagnosed with both cerebral venous sinus thrombosis and intracranial Cryptococcus simultaneously
Introduction
It has been reported by Liang (1) that the incidence rate of cerebral venous thrombosis (CVT) during pregnancy and puerperium is 11.6 per 100,000 deliveries in developed countries (2), around 450 per 100,000 deliveries in India (3) and 202 per 100,000 deliveries in China. It has been suggested that one of the main pathophysiologic changes that lead to pregnancy-related CVT is the hypercoagulability in pregnancy and puerperium (1). Other related factors may include iron deficiency anemia, alteration of platelet function as well as serum prothrombotic and anti-thrombotic molecules levels, injury and bleeding during labor and delivery (1). Intracranial cryptococcal infection occurs mainly in immunocompromised patients, ranging from those who are infected with human immunodeficiency virus (HIV) to those who are suffering from severe immune diseases (4). It was rarely reported on pregnant women without any immunodeficiency (5). There was only one case (6) reporting that intracranial cryptococcal infection was one of the rare causes of CVT. However, occurrence of HIV-negative pregnant woman with both CVT and intracranial cryptococcal infection simultaneously has not been reported yet. Here we discuss a HIV-negative pregnant patient who was diagnosed with both diseases at the same time.
Case presentation
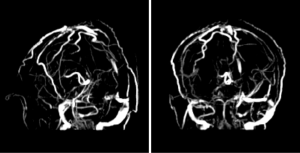
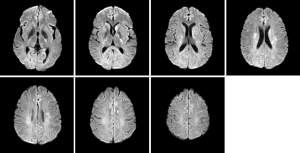
A 31-year-old pregnant woman at 35.5 weeks’ gestation was admitted to our hospital because of recurrent headache, which had last for a month. It was paroxysmal headache without any symptom of limb twitching, nausea or vomiting, but accompanied with irritability. This was her second pregnancy. She was briefly healthy before except an upper respiratory infection one month before admission. She also denied any history of otitis media, rhinosinusitis, abortion, oral contraceptives or travelling to endemic area. Given the persistence of headache after symptomatic treatment, we did not exclude nervous system diseases. The patient received cranial magnetic resonance venography (MRV) after careful physical examinations and was confirmed with thrombi in bilateral transverse sinuses, superior sagittal sinus and inferior longitudinal sinus (Figure 1). MRV also indicated multiple ischemic foci in the left center of semi oval circle, bilateral basal ganglia and cerebellar hemispheres (Figure 2). Considering the risk that the fetus would face, caesarean section was performed immediately after her admission and followed by prompt transfer to our intensive care unit (ICU) for post-operative care and diagnostic evaluation. The patient was in normal temperature upon arrival of ICU without any manifestation of cranial or facial infection. Blood test showed that white blood cell count was 11.3×109/L, C-reactive protein was 5.9 mg/L and procalcitonin was 0.04 ng/mL. Serologic tests revealed CD4/CD8 ratio of 1.31, IgM of 0.65 g/L (normal, 0.40–2.3 g/L), IgA of 6.89 g/L (7.0–16.0 g/L) and IgG of 6.89 g/L (7.0–16.0 g/L). Prothrombin time was 11.0 s, activated partial thromboplastin time was 26.2 s and D-dimer was 469 ug/L. Anti-phospholipid antibody was normal. Anti-edema treatment was initiated after the surgery while intramuscular low molecular heparin was prescribed 12 hours after. Lumbar puncture that was performed six hours after the transfer to ICU revealed an intracranial pressure of more than 400 mmH2O as well as canary yellow-appeared cerebral spinal fluid (CSF). Analysis of CSF showed nucleated cell count of 628/uL, neutrophils 68%, lymphocytes 24%, monocytes 8%, glucose level of 0.93 mmol/L, protein level of 1,263 mg/dL, adenosine deaminase of 1.0 U/L, lactate deaminase of 60.8 IU/L and chloride of 123 mmol/L. India stain of CSF (Figure 3) indicated cryptococcal infection as later CSF and blood culture also indicated. However, the patient was neither related to HIV infection nor immune diseases. Anti-fungal therapy with amphotericin B (300 mg/day) and flucytosine (4,000 mg/day) were given upon diagnosis for 8 weeks. Methylprednisolone (80 mg/day) was used in parallel but gradually adjusted. And these were substituted by fluconazole (400 mg/day) after. There was no severe complication during the treatment. The symptom of headache was ameliorated gradually till its complete disappearance after 2 months. Continuous fluconazole was advised when the patient was discharged in order to achieve one-year course of the antifungal therapy. We also prolonged the treatment of the Metso (8 mg/d) according to the severity of symptom. However, 2 months after discharge, the patient self-discontinued Metso, which led to reappearance of mild headache. Following our suggestion, the patient retook Metso and had not complained any incidence of headache since then. It is the eighth month of the anti-fungal therapy and she is in good condition and keeps regular follow-ups in clinic.
Discussion
CVT has been reported as a rare neurologic emergency, which is more common on pregnant and puerperal women than general population (7). Previous study has suggested that the major pathophysiologic change that leads to pregnancy-related CVT is the hypercoagulable state during pregnancy and puerperium (1). The previous study (1) also reported that the morbidity rate of CVT during pregnancy and puerperium is 11.6 per 100,000 deliveries in developed countries (2), around 450 per 100,000 deliveries in India (3) and 202 per 100,000 deliveries in China. Intracranial cryptococcal infection is commonly found in immunocompromised patients, such as patients with HIV or other immune diseases (4). One explanation for Cryptococcus infection on pregnant women is that they are in a relatively immunocompromised condition and predisposed to the opportunistic fungal infection (8). However, intracranial cryptococcal infection is still rare on pregnant woman without immunodeficiency (5), let alone accompanying with CVT. An immunocompetent patient was simultaneously diagnosed with CVT and intracranial cryptococcal infection during pregnancy, which induces us to report it as a rare case. It is widely accepted that headache is the most common symptom of both neurological cryptococcosis and CVT (1,5). Therefore, it was difficult for us to diagnose both diseases in a HIV-negative pregnant woman without the result of the lumbar puncture, especially when CVT itself could totally explain the manifestations of the patient. She might be in great motility risk if the fungal infection was not properly diagnosed and promptly treated. In general, we are not likely to consider intracranial infection if a patient does not present with any symptom of recurrent infection or central nervous system (CNS) sign. One clue we could find on this patient was that she had upper respiratory infection followed by headaches one month prior to admission. However, it is still unclear to us whether the CNS infection was developed earlier than CVT. On the other hand, hypercoagulable state during pregnancy is also responsible for the increased the susceptibility to CVT. There is a report presenting that the intracranial cryptococcal infection is one of the rare cause of the CVT (6). We still cannot identify whether the pre-existing upper respiratory infection would lead to a immunocompromised status and further cause the cryptococcal infection that triggered the CVT formation since pregnancy alone can increase the risk of CVT. On the other hand, raised intracranial pressure in cryptococcal infection could interrupt CSF circulation, especially as well as venous drainage, which could explain the pathogenesis of CVT. These two diseases can be independently or sequentially developed. Given the similar clinical manifestation, lumbar puncture is critical for differential diagnosis in such patient. It was reported by Liang et al. (1) that infection is the most common cause of CVT, but they haven’t described a specific type of infection or the essence of routine lumbar puncture on CVT patients. As far as we concerned, even if CVT is explicitly diagnosed and able to explain the manifestations, we need to be cautious about the underlying condition, especially CNS infection. We still consider it necessary to perform lumbar puncture on patient without significant CNS infection signs or symptoms if the patient is infected during the pregnancy.
In summary, our patient was diagnosed with both CVT and intracranial cryptococcal infection simultaneously during pregnancy in absence of immunocompromised condition. With the timely caesarean section, the fetus was delivered healthily. The prognosis of this patient is benign upon appropriate anti-fungal treatment.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was taken from the patient for publication of this case report.
References
- Liang ZW, Gao WL, Feng LM. Clinical characteristics and prognosis of cerebral venous thrombosis in Chinese women during pregnancy and puerperium. Sci Rep 2017;7:43866. [Crossref] [PubMed]
- Lanska DJ, Kryscio RJ. Risk factors for peripartum and postpartum stroke and intracranial venous thrombosis. Stroke 2000;31:1274-82. [Crossref] [PubMed]
- Srinivasan K. Cerebral venous and arterial thrombosis in pregnancy and puerperium. A study of 135 patients. Angiology 1983;34:731-46. [Crossref] [PubMed]
- Byrnes EJ 3rd, Marr KA. The Outbreak of Cryptococcus gattii in Western North America: Epidemiology and Clinical Issues. Curr Infect Dis Rep 2011;13:256-61. [Crossref] [PubMed]
- Costa ML, Souza JP, Oliveira Neto AF, et al. Cryptococcal meningitis in HIV negative pregnant women: case report and review of literature. Rev Inst Med Trop Sao Paulo 2009;51:289-94. [Crossref] [PubMed]
- Senadim S, Alpaydin Baslo S, Tekin Güveli B, et al. A rare cause of cerebral venous thrombosis: cryptococcal meningoencephalitis. Neurol Sci 2016;37:1145-8. [Crossref] [PubMed]
- O'Brien P, Heaney D. Cerebrovascular complications during pregnancy and the puerperium. Eur J Neurol 2011;18:801-2. [Crossref] [PubMed]
- Ely EW, Peacock JE Jr, Haponik EF, et al. Cryptococcal pneumonia complicating pregnancy. Medicine (Baltimore) 1998;77:153-67. [Crossref] [PubMed]
Cite this article as: Ren B, Guo Y, Chen K, Chen L. An anti-human immunodeficiency virus-negative pregnant woman was diagnosed with both cerebral venous sinus thrombosis and intracranial Cryptococcus simultaneously. J Emerg Crit Care Med 2018;2:55.



