
Nutritional therapy for burns in children
Introduction
Polytrauma (multi-trauma) is a short verbal equivalent to describe (mainly) blunt trauma patients whose injuries involve multiple body regions or cavities, compromise the patients’ physiology and potentially cause dysfunction of uninjured organs. These patients are at risk of higher morbidity and mortality than the summation of expected morbidity and mortality of their individual injuries (1). Burns are the main example of polytrauma, as they affect the skin, as well as the cardiovascular, respiratory and renal systems. In polytrauma management a pivotal role is played by nutritional support.
Among children, burns are a serious injury and one of the main reasons of trauma, especially during the first 5 years of life. For these patients, the nutritional support has been acknowledged as one of the most significant aspects of the medical burns treatment in terms of mere nutrition and protection from infections.
Energy target
In burned children, a sound increase in caloric requirement is necessary, as much as in adults, because of a marked hypermetabolism immediately or early after burn. Hypermetabolism can be caused by burn injuries, by the release of catecholamines just after the injury, but also by pain, anxiety, surgical procedures, and metabolic requirements by tissues. Moreover, it can persist for up 2 years post burn.
Resting energy expenditure (REE) has a curvilinear increasing trend according to the total burned surface area (TBSA). Hence, children with burns affecting ≤10% of total body surface area have a percentage of REE very close to the normal, whereas children with burns affecting more than 40% of TBSA have an increase in REE, which becomes 1–1.5 times higher than standard by the first 2 weeks post burn.
Evidence shows that in sterile environments, at a temperature of 30 °C, the metabolic rates of the patients under consideration are around 150% REE, and they decrease to 135% upon wound healing (2).
The loss of weight and the various metabolic measurements lead to the development of the concept of “hyper-nutrition” that causes a massive over-nutrition of the patient, such as the uptake of 5,000 kcal/die, that is considered normal according to the equation of Curreri (3). The supply of too many calories has been, nevertheless, often associated to an acceleration of metabolism, hyperglycemia, liver failure and an increase in the production of carbon dioxide (4-6). Most equations and mathematic formulas, developed to estimate energy requirements in burned patients, use, in fact, body weight, age, sex and burned surface area as the key determinants of the calories intake, and they do not consider the wide range of variations along the timeline.
Over the last years, several studies have shown that the increase in REE is more evident in the first weeks, and gradually decreases thereafter. Moreover, the advancements in treatment of burn injuries have reduced the amplitude of hypermetabolic response, and thus the target of a more moderate nutrition has been possible (7). For these reasons, indirect calorimetry is considered the most accurate method to evaluate the energy output of burned patients (8).
That technique allows to evaluate energy expenditure by measuring any O2 and CO2 variation in respiratory gases, and by calculating the oxidation of energy substrates (carbohydrates, lipids, proteins). Measurements are taken after meals, and results are rounded to the nearest thousandth, without exceeding 10% of the measured value. Moreover, as the metabolic rate varies in patients during the recovery period, it is recommended to use indirect calorimetry twice a week for a correct regulation of the nutritional support. However, in case this method cannot be applied, the formulas most frequently used to evaluate the energy expenditure in burned children are reported in Table 1 (9).
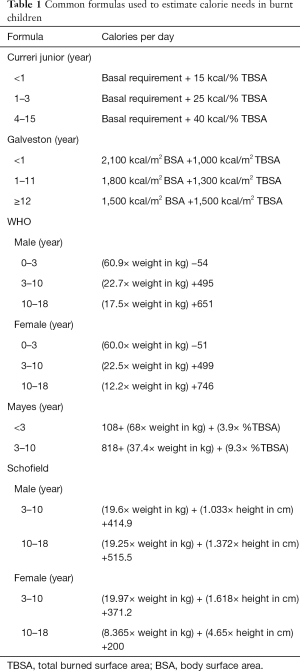
Full table
Nutritional support
Nutritional therapy is very important to offer favorable conditions for the establishment of the therapeutic plan and to provide energy, fluids and nutrients in adequate quantities so as to maintain vital functions and homeostasis. Nutritional support also contributes to recovering the activity of immune system, reducing the risks of overfeeding, ensuring offers of protein and energy necessary to minimize the protein catabolism and nitrogen loss (10).
In children with major burns, an adequate and efficient nutritional therapy is necessary as soon as possible, in order to limit losses and obtain a positivization of nitrogen balance, to reduce translocation bacteremia from the colon and to increase immune function.
As regards the nutritional intake of macronutrients, protein needs of burned patients are increased because of losses through urine and wounds, increased use in gluconeogenesis, and wound healing. High-protein feedings have shown successful in burned patients. Protein need in burned children is generally agreed to be higher than recommended dietary allowance (11). In burned children, a diet with increased protein intake (23% of total calories) was associated with improved immune function, less bacteremia and increased survival. As burn size increases, progressively more protein is required for positive nitrogen balance (12). Protein requirements have been considered to be around 1.5–3.0 g/kg/die (7,12).
As essential fatty acid deficiency is a well-documented complication in hospital patients receiving long-term nutritional supplements, most intensive care units (ICUs) provide a significant amount of caloric requirements as fat. This has been shown to reduce the requirements for carbohydrates and can improve significantly glucose tolerance, which is often altered in the patient after burn. For these reasons, diets containing 30% to 50% fat have become commonplace in the therapy of critically sick patients throughout the world. However, several studies showed that increased fat administration may lead to increased complications, including hyperlipidemia, hypoxemia, hepatic steatosis, a higher incidence of infection and a higher postoperative mortality rate in the burned patient population (13).
Recent reviews and guidelines enable recommending to deliver 55–60% of the total energy intake (TEI), as carbohydrates without exceeding 5 mg/kg/min, whereas lipid intake should be lower than 35% of TEI (7).
As regards the intake of micronutrients, vitamin needs are increased for burned patients to stimulate wound healing. Vitamin C is involved in collagen synthesis and immune function and may be required in increased amounts for wound healing. Vitamin A is also an important nutrient for immune function and epithelialization. Vitamin D is needed for burned patients because burns cause an impairment of vitamin D metabolism with resultant low 25-hydroxy vitamin D levels and reduced bone formation in adults and children but the exact requirements in burned subjects have not been determined (11). Also zinc is required for many metalloenzymes associated with wound healing and immune function (12).
Children suffering from major burns should receive vitamin supplementation in the form of a multivitamin, in addition to vitamin C, vitamin A and zinc sulfate to ensure adequate wound healing (14,15), as shown in Table 2.
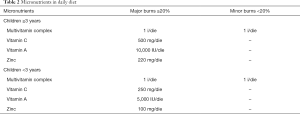
Full table
Whether the nutritional therapy is adequate or otherwise should be checked by monitoring body weight and nitrogen balance.
Route and timing of administration
Nutritional therapy should be initiated early within 12 h of injury and preferentially by the enteral route (7).
Very early enteral feeding, i.e., initiated within the first 6–12 h after injury by the gastric route, is associated with numerous clinical and biological advantages, such as attenuation of the stress hormone levels and of the hypermetabolic response (16), and it results in increased immunoglobulin production (17), reduction of stress ulcers, while reducing the risk of malnutrition and of energy deficit (18,19). Other studies recommended that feedings should be started soon after fluid resuscitation is complete to avoid gastrointestinal dysfunction (11). Early enteral feeding within 24 h from hospitalization has been shown to decrease the hypercatabolic response, thus decreasing the release of catecholamines, glucagon, and weight loss, increase caloric intake, stimulate insulin secretion, improve protein retention, and shorten hospital length of stay (11). The reluctance of some clinicians to start immediate enteral feeding is related to a fear that it will result in more complications than delayed feeding. This has been shown not to be warranted (20).
Tube feeding can be given through different types of tubes which, depending on whether they are placed through the nose into the stomach or bowel, are called nasogastric or nasoenteral feeding tubes, respectively.
When enteral nutrition is contraindicated or is not feasible, or when it cannot guarantee an adequate intake of nutrients in early stages, because the patients have severe diarrhea or serious tube feeding intolerance or previous gastrointestinal problems and cannot have sufficient enteral calories, parenteral nutrition is used. This parenteral nutrition should be by the central route because peripheral support will not provide adequate calories to prevent catabolism from the burns (11). Parental nutrition implies an even stricter monitoring of glycemia and adherence to the patient’s energy requirement to avoid overfeeding (7,14). Central lines used for total parental nutrition can develop serious infections, including catheter sepsis, septic thrombophlebitis, and even endocarditis and risk is increased if lines are left in place for long periods, and if they are used for multiple purposes (blood draws, hemodynamic monitoring, antibiotics maintenance fluids, etc.) (12). Hence the use of parenteral nutrition should be limited to only extreme cases.
Conclusions
To conclude, it is mandatory to perform an accurate evaluation of the nutritional status of burned patients. Patient’s energy requirement is to be assessed through indirect calorimetry. An adequate amount of calories must be provided to tackle patient hypermetabolism. It is also necessary to increase the protein intake, as long as a satisfactory healing of wounds is achieved. Nutrients should be supplied preferably by early enteral feeding, whereas parenteral nutrition is to be limited to the cases where enteral feeding is contraindicated, or is not feasible, or cannot guarantee an adequate supply of nutrients in the early stages.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus. Injury. 2009;40 Suppl 4:S12-22. [Crossref] [PubMed]
- Jeschke MG, Chinkes DL, Finnerty CC, et al. Pathophysiologic response to severe burn injury. Ann Surg 2008;248:387-401. [PubMed]
- Rodriguez NA, Jeschke MG, Williams FN, et al. Nutrition in Burns: Galveston Contributions. JPEN J Parenter Enteral Nutr 2011;35:704-14. [Crossref] [PubMed]
- Askanazi J, Elwyn DH, Silverberg PA, et al. Respiratory distress secondary to a high carbohydrate load: a case report. Surgery 1980;87:596-8. [PubMed]
- Askanazi J, Rosenbaum SH, Hyman AI, et al. Respiratory changes induced by the large glucose loads of total parenteral nutrition. JAMA 1980;243:1444-7. [Crossref] [PubMed]
- Burke JF, Wolfe RR, Mullany CJ, et al. Glucose requirements following burn injury. Parameters of optimal glucose infusion and possible hepatic and respiratory abnormalities following excessive glucose intake. Ann Surg 1979;190:274-85. [Crossref] [PubMed]
- Rousseau AF, Losser MR, Ichai C, et al. ESPEN endorsed recommendations: Nutritional therapy in major burns. Clin Nutr 2013;32:497-502. [Crossref] [PubMed]
- Suman OE, Mlcak RP, Chinkes DL, et al. Resting energy expenditure in severely burned children: analysis of agreement between indirect calorimetry and prediction equations using the Bland-Altman method. Burns 2006;32:335-42. [Crossref] [PubMed]
- Schulman CI, Ivascu FA. Nutritional and Metabolic Consequences in the Pediatric Burn Patient. J Craniofac Surg 2008;19:891-4. [Crossref] [PubMed]
- Medeiros NI, Schott E, Silva R, et al. Efeitos da terapia nutricional enteral em pacientes queimados atendidos em hospital publico de Joinville, Santa Catarina. Rev Bras Queimaduras 2009;8:97-100.
- Chan MM, Chan GM. Nutritional therapy for burns in children and adults. Nutrition 2009;25:261-9. [Crossref] [PubMed]
- Saffle JR, Graves C. Nutritional support of the burned patient. In: Total Burn Care. Elsevier Inc., 2007:398-419.
- Lee JO, Gauglitz GG, Herndon DN, et al. Association between dietary fat content and outcomes in pediatric burn patients. J Surg Res 2011;166:e83-90. [Crossref] [PubMed]
- Gonzalez R, Shanti CM. Overview of current pediatric burn care. Semin Pediatr Surg 2015;24:47-9. [Crossref] [PubMed]
- Samour PQ, Helm KK, Lange CE. Handbook of pediatric Nutrition, 2nd edition. Aspen Publishers, Inc. Gaitherburg, Maryland, 1999:502.
- Mochizuki H, Trocki O, Dominioni L, et al. Mechanism of prevention of postburn hypermetabolism an catabolism by early enteral feeding. Ann Surg 1984;200:297-310. [Crossref] [PubMed]
- Lam NN, Tien NG, Khoa CM. Early enteral feeding for burned patients: an effective method which should be encouraged in developing countries. Burns 2008;34:192-6. [Crossref] [PubMed]
- Chiarelli A, Enzi G, Casadei A, et al. Very early nutrition supplementation in burned patients. Am J Clin Nutr 1990;51:1035-9. [Crossref] [PubMed]
- Venter M, Rode H, Sive A, et al. Enteral resuscitation and early enteral feeding in children with major burnseeffect on McFarlane response to stress. Burns 2007;33:464-71. [Crossref] [PubMed]
- Hansbrough WB, Hansbrough JF. Success of immediate intragastric feeding with patients with burns. J Burn Care Rehabil 1993;14:512-6. [Crossref] [PubMed]
Cite this article as: Galfo M, De Bellis A, Melini F. Nutritional therapy for burns in children. J Emerg Crit Care Med 2018;2:54.


