The National Institutes of Health Stroke Scale score—a valuable stroke scale used in emergency in predicting the need for mechanical ventilation and outcome in patients of acute ischemic stroke
Introduction
Stroke is the third leading cause of death in developed countries and the leading cause of long term disability (1). Up to 10% of patients with acute stroke need mechanical ventilation (MV) due to different reasons. Patients with stroke who require MV are thought to have a very poor prognosis with mortality up to 90% and severe disability despite aggressive treatment in the ICU (1,2). However, timely MV has been found to improve the outcome of such patients (3,4). Hence identification of clinical predictors and methods which predict survival and meaningful outcome are also important, as it may influence the management decisions and justification for the use of resources. The present study has the objective of determining the predictor accuracy of the National Institutes of Health Stroke Scale (NIHSS) score for requirement of MV and outcome in patients of acute ischemic stroke.
Methods
Aim and objective
The objective of this study is to find the predictor accuracy of NIHSS score in determining the requirement for MV and outcome of patients of acute ischemic stroke.
Study design
This study was carried out in Max Superspeciality Hospital Saket, New Delhi over a period of 1.5 years. It was a prospective, cohort study.
Inclusion criteria
Patients included in the study were having all of the following: (I) stroke defined as the presence of sudden onset of focal neurological deficit and admitted within 24 h of onset of symptoms; (II) age ≥18 years and (III) written informed consent available from the legal representative of the patients.
Exclusion criteria
Patients meeting the inclusion criteria would be excluded if they would be already on ventilator support at the time of admission.
Methods of measurement of outcome of interest
The patients of acute ischemic stroke were categorized into those with NIHSS score ≤5, NIHSS score between 6 and 13 and those with NIHSS score ≥14. The predictor accuracy for the requirement of mechanical ventilator was determined for NIHSS score of ≥14. Mortality and outcome in terms of the Modified Rankin Scale (MRS) was determined in each of the NIHSS categories.
The need for the ventilation was defined by the following factors as per the standard guidelines for MV i.e., by GCS, Respiratory rate and Arterial blood gas analysis (SPO2, PAO2 and PCO2). The outcome of the patients of acute stoke was analyzed for the mortality during the hospital stay and disability if any at the time of discharge by MRS
Data collection methods
NIHSS score was applied to all acute ischemic stroke patients who were eligible for the analysis. All patients were followed up during their hospital course and records were made if they required MV and cause of intubation, clinical findings at the time of intubation, complications during hospitalization and intervention was also recorded.
Statistical analysis
The predictive utility of NIHSS score was evaluated by running a logistic regression separatively for cases requiring MV and for cases not surviving or surviving (5). Statistical significance of each predictor was assessed at 5%× level and the odds ratio (OR) and their confidence intervals were obtained. These ORs would quantify the predictive utility of various parameters. SPSS 16 software was used for statistical analysis.
Ethics committee review
This research was carried out in accordance with the Basic Principles defined ICMR ‘ethical guidelines for biomedical research on human participants [2006]’, CDSCO guidance on good clinical practice for clinical research India.
The study was conducted only after the approval by the Scientific and Ethics committees of the hospital (approval No. TS/MSSHSKT/MHIL/NEURO/MHEC/15-02).
Results
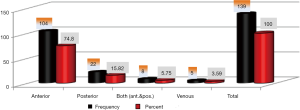
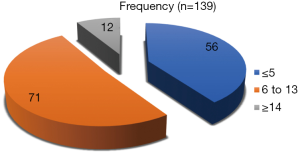
A total of 139 patients were found eligible for the study and were included for the analysis. We found that 90 (64.74%) patients were males and 49 (35.26%) were females. About 70% of patients were in the age group between 60 and 80 years and 21% patients were in the age group of 20 to 40 years. In case of ischemic stroke 104 patients were having involvement of the anterior territory, 22 patients had involvement of the posterior territory and remaining 8 patients were having involvement of both anterior and posterior circulation whereas 5 patients were having the venous infarct as shown in Figure 1. While categorizing the patients of ischemic stroke on the basis of NIHSS score, 56 (40.28%) patients had NIHSS score of ≤5, 71 (51.07%) patients had NIHSS score between 6 and 13 and remaining 12 (8.63%) patients had NIHSS score of ≥14 as shown in Figure 2.
Among the 139 patients of ischemic stroke and venous stroke, 32 patients were put on the mechanical ventilator.
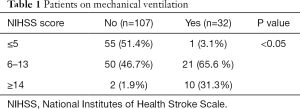
In case of ischemic stroke patients who required the MV 21 (65.6%) were having NIHSS score between 6 and 13, 10 (31.3%) patients were having NIHSS score of ≥14 and only one (3.1%) was having NIHSS score of ≤5 as shown in Table 1. We applied the NIHSS score to the patients of venous stroke also. Out of 5 (3.03%) patients of the venous stroke, 2 (40%) patients were put on the mechanical ventilator.
Full table
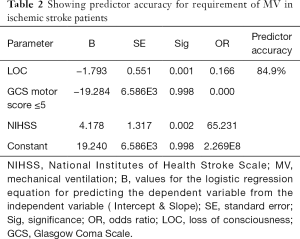
For patients of ischemic stroke presence of loss of consciousness at onset, GCS motor score ≤5 and NIHSS score showed a predictor accuracy of 84.9% for the requirement of MV (Table 2).
Full table
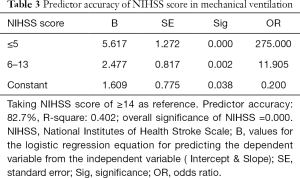
While doing the regression analysis we found the predictor accuracy of NIHSS score of about 82.7% in determining the need for ventilation support (Table 3).
Full table
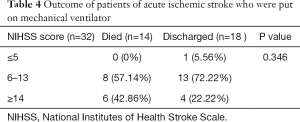
Out of 32 patients of the ischemic stroke who were put on MV 14 (43.75%) expired while as rest were discharged. Among the patients of ischemic stroke mortality rate was 57.14% (8 patients) in patients having NIHSS score between 6 and 13 and mortality was 0% in patients with an NIHSS score of ≤5 (P value =0.346) (Table 4).
Full table
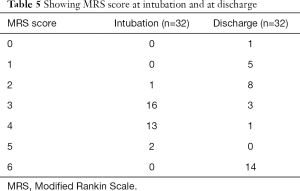
The patients who were put on mechanical ventilator and survived 77.78% (14 out of 18 patients) were having favorable outcome (MRS score ≤2) at the time of discharge where only 22.22% (4 out of 18 patients) were having unfavorable outcome (MRS score >2). Table 5 below shows the MRS score at intubation and at discharge of patients of acute ischemic stroke who were put on MV.
Full table
Discussion
In our study about 139 patients met the inclusion and exclusion criteria and were enrolled for statistical analysis and discussion. In our study we found that 64.84% of patients were males whereas 35.26% of the patients were females. A study conducted in Pakistan by Marwat et al. showed, male preponderance in stroke patients (70.4% vs. 29.6%) (6,7) which was quite in accordance with our study. The rate of MV in our study for ischemic stroke patients was 23.02%. This was in accordance with the similar study conducted by Gupta et al. (8) who reported a MV rate of 16.0% for acute ischemic stroke patients.
Among the 139 patients of ischemic stroke and venous stroke, 32 patients were put on the mechanical ventilator. In case of ischemic stroke patients who required the MV 21 (65.6%) were having NIHSS score between 6 and 13, 10 (31.3%) patients were having NIHSS score of ≥14 and only one (3.1%) was having NIHSS score of ≤5 as shown in Table 1. We applied the NIHSS score to the patients of venous stroke also. While doing the regression analysis we found the predictor accuracy of NIHSS score of about 82.7% in determining the need for ventilation support. NIHSS has been found to be a good predictor in stratifying the patients of acute stroke at the time of admission. Daniel Schlegel et al. in their study had found that disability and need for long term disability increases with increase in the NIHSS score and they had found that for each 1-point increase in NIHSS, the likelihood of patients going home was significantly reduced (OR, 0.79; 95% CI, 0.70 to 0.89, P<0.001) (9).
The overall mortality rate in case of patients acute ischemic stroke who required MV was 43.75%. Gupta et al. had reported an overall mortality of 52% in patients of acute stroke who required MV and it was 34% in patients of ischemic stroke and 62% in patients of hemorrhagic stroke. Santoli et al. in their study of 58 patients who required ventilator support, 16 had meaningful survival at the end of 1 year (10). Most of the reported previous studies of intubated patients with stroke have reported a mortality of 49% to 93%. Mayer et al. reported overall mortality at 30 days as 60% and it was 50% in patients with ischemic stroke and 71% in patients hemorrhagic stroke (11). Ludwigs et al. reported a subgroup of 65 patients from 1976 to 1986 admitted to ICU and intubated for stroke who had 75% of ICU mortality and 92% in-hospital mortality rates (12). Wijdicks et al., reported a 71% mortality rate in a series of patients intubated for hemispheric stroke, and an 88% mortality rate in vertebrobasilar ischemic stroke (13).
While seeing the mortality with respect to NIHSS in patients of ischemic stroke who were put on MV, we recorded 57.14% (8 patients) mortality rate in patients having NIHSS score between 6 and 13 while as mortality was 0% in patients with an NIHSS score of ≤5 (P value =0.346). In a study conducted by Schlegel et al., it has been observed that for each 1-point increase in NIHSS, the likelihood of patients going home was significantly reduced (OR, 0.79; 95% CI, 0.70 to 0.89, P<0.001). Categorization of NIHSS was also predictive of disposition, with NIHSS ≤5 being most strongly associated with discharge home, NIHSS 6 to 13 with rehabilitation, and NIHSS >13 with long term nursing facility requirement (P<0.001) (9).
In a study conducted by Shrestha et al. in Nepal it was found that Stroke subtype and baseline NIHSS scores were associated with death/disability (27, 48.2%) at 3 months. Large artery strokes and higher NIHSS scores were found to be significant predictors of poor outcome at 3 months (14).
Similarly in a study conducted by Adams et al. it was observed that baseline NIHSS score strongly predicted outcome, with one additional point on the NIHSS decreasing the likelihood of excellent outcomes at 7 days by 24% and at 3 months by 17%. It was also concluded that the NIHSS score strongly predicts the likelihood of a patient’s recovery after stroke. An NIHSS score of ≥16 forecasts a high probability of death or severe disability whereas a score of ≤6 forecasts a good recovery (15).
We observed in our study that MRS score predicts the requirement for MV in case of ischemic stroke patients as majority of the patients who were put on MV were having MRS score of 3 or more than 3 (P value <0.01).
The patients who were put on mechanical ventilator and survived 77.77% (14 out of 18 patients) were having favorable outcome (MRS score ≤2) at the time of discharge where only 22.23% (4 out of 18 patients) were having unfavorable outcome (MRS score >2). In a study conducted by Eva Schielke while evaluating the long-term outcome of patients with ischemic stroke requiring MV it was found that out of 33 surviving patients, 9 (27%) had a good functional outcome (MRS 0–2) (16).
Conclusions
We observed that males outnumbered the females in stroke prevalence (64.74% vs. 35.26%). We recorded a bit higher prevalence of stroke (21%) in young people (age than 40 years) than other studies (10% to 15%). Significant proportion of the patients with acute ischemic stroke (23.02%) required MV. We concluded that loss of consciousness at onset, GCS motor score ≤5 (OR =0.000) and NIHSS score were associated with overall predictor accuracy of 84.9% in determining the need for MV. NIHSS score individually was found to have predictor accuracy of 82.7% in determining the need for MV. The overall mortality rate in patients of acute ischemic stroke who were put on MV was 43.75%.
While correlating the NIHSS score with the mortality rate, 53.84% mortality rate was found in patients having NIHSS score between 6 and 13 compared to 0% mortality in patients with NIHSS score of ≤5. The patients who were put on mechanical ventilator and survived 77.77% (14 out of 18 patients) were having favorable outcome (MRS score ≤2) at the time of discharge where only 22.23% (4 out of 18 patients) were having unfavorable outcome (MRS score >2).
Keeping in view the increasing prevalence of stroke in young adults and the mortality associated with acute stroke we recommend that early recognition of the predictors determining the need for MV thereby improving the outcome of stroke patients should be contemplated at the earliest as soon as the patient lands in hospital
We recommend that stroke scores like NIHSS score should be applied to the patients of acute ischemic stroke to stratify the patients with regard to their severity and proper standardization of care to be undertaken. This will enable the physicians at the primary and secondary healthcare level to refer the sick patients to tertiary care hospitals as soon as the patients are examined by them.
Acknowledgements
Authors acknowledge the immense help received from the scholars whose articles are cited and included in the references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was conducted only after the approval by the Scientific and Ethics committees of the hospital (approval No. TS/MSSHSKT/MHIL/NEURO/MHEC/15-02). Written informed consent available from the legal representative of the patients.
References
- Burtin P, Bollaert PE, Feldmann L, et al. Prognosis of stroke patients undergoing mechanical ventilation. Intensive Care Med 1994;20:32-6. [Crossref] [PubMed]
- el-Ad B, Bornstein NM, Fuchs P, et al. Mechanical ventilation in stroke patients--is it worthwhile? Neurology 1996;47:657-9. [Crossref] [PubMed]
- Steiner T, Mendoza G, De Georgia M, et al. Prognosis of stroke patients requiring mechanical ventilation in a neurological critical care unit. Stroke 1997;28:711-5. [Crossref] [PubMed]
- Shah B, Prashant M. Workshop report on stroke surveillance in India, division of noncommunicable diseases. New Delhi, India: Indian Counc Med Res, 2006.
- Zhang Z. Univariate description and bivariate statistical inference: the first step delving into data. Ann Transl Med 2016;4:91. [Crossref] [PubMed]
- Llinas RH. Overview of the approach to the stroke patient. In: Wityk RJ, Llinas RH, editors. Stroke. Mumbai: Aramuc India Ltd., 2007:1-4.
- Marwat MA, Usman M, Hussain M. Stroke and its relationship to risk factors. Gomal J Med Sci 2009;7:17-21.
- Gupta P, Prasad K, Kumar A, et al. Clinical predictors and outcome of patients of acute stroke requiring ventilatory support: a prospective hospital based cohort study. J Neurol Sci 2014;337:14-7. [Crossref] [PubMed]
- Schlegel D, Kolb SJ, Luciano JM, et al. Utility of the NIH Stroke Scale as a predictor of hospital disposition. Stroke 2003;34:134-7. [Crossref] [PubMed]
- Santoli F, De Jonghe B, Hayon J, et al. Mechanical ventilation in patients with acute ischemic stroke: survival and outcome at one year. Intensive Care Med 2001;27:1141-6. [Crossref] [PubMed]
- Mayer SA, Copeland D, Bernardini GL, et al. Cost and outcome of mechanical ventilation for life-threatening stroke. Stroke 2000;31:2346-53. [Crossref] [PubMed]
- Ludwigs UG, Baehrendtz S, Wanecek M, et al. Mechanical ventilation in medical and neurological diseases; 11 years of experience. J Intern Med 1991;229:117-24. [Crossref] [PubMed]
- Wijdicks EF, Scott JP. Causes and outcome of mechanical ventilation in patients with hemispheric ischemic stroke. Mayo Clin Proc 1997;72:210-3. [Crossref] [PubMed]
- Shrestha S, Poudel RS, Khatiwada D, et al. Stroke subtype, age, and baseline NIHSS score predict ischemic stroke outcomes at 3 months: a preliminary study from Central Nepal. J Multidiscip Healthc 2015;8:443-8. [Crossref] [PubMed]
- Adams HP Jr, Davis PH, Leira EC, et al. Baseline NIH Stroke Scale score strongly predicts outcome after stroke: A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology 1999;53:126-31. [Crossref] [PubMed]
- Schielke E, Busch MA, Hildenhagen T, et al. Functional, cognitive and emotional long-term outcome of patients with ischemic stroke requiring mechanical ventilation. J Neurol 2005;252:648-54. [Crossref] [PubMed]
Cite this article as: Dar MA, Aggarwal V, Ahmad PB, Reddi R, Mukherjee JD, Goel K, Dar OH. The National Institutes of Health Stroke Scale score—a valuable stroke scale used in emergency in predicting the need for mechanical ventilation and outcome in patients of acute ischemic stroke. J Emerg Crit Care Med 2018;2:49.