Infection control bundles in low-middle income countries: an international cross-sectional survey (study protocol)
Introduction
Nosocomial infections (NIs) are the most common adverse events related to health care worldwide, with high morbidity, mortality and economic burden. Also, it is an important quality measure for hospitals (1). NIs affects 5–10% of admitted patients and the incidence is highest in intensive care units (ICUs) with the rate exceeding 25%. For many reasons, in low-to-middle income countries (LMICs), the magnitude of the problem is bigger than high income countries; over 10% in hospitals and reach 50% in ICUs (2-4). Although LMICs represent 80% of the global population, they consume only 20% of the world’s resources (5). Lower resources impact on the quality of healthcare provision and NI indicators can be helpful in gauging such impacts. As well, half of the European countries are classified as middle-income country (6). Infection prevention/control (IPC) bundles are often recommended to reduce NI burdens. However, there is limited data about NIs and infection control measures from LMICs (7). Our hypothesis is that organisation of infection control activities and compliance of infection control bundles in LMICs are lower than high income countries (HICs).
Methods
The report will describe the practices of infection control from participating investigators in 2017. A questionnaire will be emailed by invitation to Infectious Diseases International Research Initiative (ID-IRI) Group Members (314 members in 2017) and dedicated IPC doctors working in LMICs (46 doctors) to examine self-reported practices/policies regarding IPC bundles. Also, the survey will be send to dedicated IPC doctors in high income European countries with low antimicrobial resistance rates (8). The survey follows the checklist rules reported by Pulcini and Leivovici (9). Informed consent or ethical board approval is not required.
Responding country incomes will be classified by World Bank definitions into low, middle and high (low-income economies are defined as those with a gross national income (GNI) per capita of $1,005 or less; lower middle-income economies are those with a GNI per capita between $1,006 and $3,955; upper middle-income economies are those with a GNI per capita between $3,956 and $12,235; high-income economies are those with a GNI per capita of $12,236 or more). Countries with incomes lower than $12,236 will be the focus of this study. Their data will be compared with a control group from high income countries.
Questionnaire
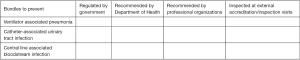
The survey will gather data on key aspects of infection control activities and bundle strategies in ICU. Details of survey are summarized in Supplementary and Figure S1.
Statistical analysis
All responses to survey questions are categorical variables and will be analyzed by using descriptive statistics, reporting proportions (percentages). Data were reported as median (IQR) when a non-normal distribution occurs. Chi-square test (or Fisher’s exact test when appropriate) will be performed to evaluate potential differences between HIC and LMIC. P value
Aim
To determine the status of IPC bundle practice and regulations in LMICs, compared with HICs with the further goal of reflecting on results, updating it and identify priorities. A secondary objective is to compare if there are differences between European and non-EU LMICs.
Supplementary
Survey questionnaire for bundle strategies
Institutional infrastructure:
- Country
- Type of hospital
- Acute secondary care hospital (yes: 1, no: 0)
- Acute secondary care hospital-tertiary referral centre
- Specialised (type of hospital)
- Population
- Adult
- Pediatric
- Combined
- Funding
- Public
- Private
- Both
- Type of ICU
- Medical
- Surgical
- Medical-surgical
- Trauma
- Coronary care
- Other
- Total number of beds in tertiary ICU
- If ≤8 (yes: 1, no: 0)
- 9–16
- ≥16
- Nurse to patient ratio (in a tertiary ICUs) in a shift?
- If 1–3 (yes: 1, no: 0)
- If 3–6 (yes: 1, no: 0)
- Infection control facilities
- Do you have any infection control committee in your hospital? (yes: 1, no: 0)
- If yes, do you have annual agreed programme? (yes: 1, no: 0)
- Do you have annual report about nosocomial infection rates? (yes: 1, no: 0)
- Do you have any full time equivalent infection control doctor? (yes: please write the number, no: 0)
- Do you have any full time equivalent infection control nurse? (yes: please write the number, no: 0)
- Surveillance
- Dou you have invasive device-related infection surveillance programme in your ICUs? (yes: 1, no: 0)
- Ventilator associated pneumonia (yes: 1, no: 0)
- Catheter-associated urinary tract infection (yes: 1, no: 0)
- Central line associated blood stream infection (yes: 1, no: 0)
- Nosocomial infection rates in ICU in 2015
- Ventilator associated pneumonia: 1,000 ventilator days
- Catheter-associated urinary tract infection: 1,000 catheter days
- Central line associated blood stream infection: 1,000 central line days
- Bundle strategies
- Do you perform bundle strategies to prevent ventilator associated pneumonia? (yes: 1, no: 0)
- If yes, with [1] or without [0] process monitoring (compliance)
- If with process monitoring
- Continuous process monitoring [1]
- Periodical (samplings-wise) [2]
- Do you perform bundle strategies to prevent catheter-associated urinary tract infection? (yes: 1, no: 0)
- If yes, with [1] or without [0] process monitoring (compliance)
- If with process monitoring
- Continuous process monitoring [1]
- Periodical (samplings-wise) [2]
- Do you perform bundle strategies to prevent central line associated blood stream infection? (yes: 1, no: 0)
- If yes, with [1] or without [0] process monitoring (compliance)
- If with process monitoring
- Continuous process monitoring [1]
- ii. Periodical (samplings-wise) [2]
- Do you perform bundle strategies to prevent dissemination of multidrug resistant pathogens?
- If yes, with [1] or without [0] process monitoring (compliance)
- If with process monitoring
- Continuous process monitoring [1]
- Periodical (samplings-wise) [2]
- Bundle parameters
- Which parameters are included in your ventilator associated pneumonia bundle?
- Hand hygiene before care of patients (yes: 1, no: 0)
- Elevation of the head of bed to 30–45 degrees
- Daily oral care with chlorhexidine
- Daily oral care with antiseptic agent other than chlorhexidine
- Daily sedation vacation and assessment of readiness to extubate
- Peptic ulcer disease prophylaxis
- Deep vein thrombosis prophylaxis
- Aspiration of subglottic secretions
- Manual control of endotracheal cuff pressure (of at least 20 cmH2O) at least every 8 hrs.
- Continuous endotracheal cuff pressure by means of an automated device
- Other
- Which parameters are included in your catheter-associated urinary tract infection bundle?
- Consideration of alternatives to indwelling urinary catheterization
- Insert catheters using aseptic technique and sterile equipment
- Hand hygiene and standard (or appropriate isolation) precautions
- Daily reviewing of necessity of the catheter
- Only properly trained persons insert and maintain catheters
- Maintain a closed drainage system (includes catheterization with the catheter already connected with the collector, i.e., closed system)M
- Maintain unobstructed urine flow
- Meatal cleaning with appropriate antiseptic solution
- Meatal cleaning with normal saline
- Obtain urine samples aseptically
- Use a catheter with the smallest gauge
- Other
- Which parameters are included in your central line associated blood stream infection bundle?
- Decontaminate hands with either antiseptic-containing soaps or alcohol-based gels/foams before inserting, repairing, replacing, or dressing a CVC
- Use a cap, mask, sterile gown, sterile gloves, and a sterile full body drape when inserting CVCs and PICCs or performing guidewire exchange(s)
- Prepare clean skin with chlorhexidine preparation with alcohol before CVC insertion and during dressing changes
- Whenever possible, use the subclavian site, rather than the jugular or femoral sites
- Minimize contamination risk by scrubbing the access site with an appropriate antiseptic (chlorhexidine, povidone iodine, or 70% alcohol) prior to accessing the CVC
- Daily evaluation and prompt removal of CVCs that are no longer clinically warranted
- The use of trained personnel dedicated to the placement of CVCs in ICU and hospitalized patients
- Use of antiseptic coated CVCs in all or selected patients?
- Use of chlorhexidine gluconate impregnated dressing (or equivalent approach)
- Other
- Bundle monitoring (yes: 1, no: 0)
- Were the introductions of bundles in your hospital accompanied by convening a group to oversee this?
- Was the group multidisciplinary including for example doctors and nurses?
- Was there an examination of the evidence base for the bundle parameters?
- Are there a group(s) which looks at the results of the bundle monitoring and ensure that results are feed-back to the relevant clinicians?
- Are the results of the bundle programme reviewed at least annually?
Acknowledgements
We would like to thank Fatma Cevahir, Infection Control Nurse in Erciyes University, Medical Faculty, Infection Control Committee, for her support while collecting data from centers and statistical analyses.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Pittet D.. Infection control and quality health care in the new millennium. Am J Infect Control 2005;33:258-67. [Crossref] [PubMed]
- Vilar-Compte D, Camacho-Ortiz A, Ponce-de-León S. Infection control in limited resources countries: challenges and priorities. Curr Infect Dis Rep 2017;19:20. [Crossref] [PubMed]
- Alp E, Damani N. Healthcare-associated infections in intensive care units: epidemiology and infection control in low-to-middle income countries. J Infect Dev Ctries 2015;9:1040-5. [Crossref] [PubMed]
- Alp E, Leblebicioglu H, Doganay M, et al. Infection control practice in countries with limited resources. Ann Clin Microbiol Antimicrob 2011;10:36. [Crossref] [PubMed]
- Shah A. Poverty Facts and Stats. Available online: http://www.globalissues.org/article/26/poverty-facts-and-stats
- The World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- Rosenthal VD. International Nosocomial Infection Control Consortium (INICC) resources: INICC multidimensional approach and INICC surveillance online system. Am J Infect Control 2016;44:e81-90. [Crossref] [PubMed]
- European Centre for Disease Prevention and Control. Surveillance of antimicrobial resistance in Europe 2016. Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). Available online: https://ecdc.europa.eu/sites/portal/files/documents/AMR-surveillance-Europe-2016.pdf
- Pulcini C, Leibovici L. CMI Editorial Office. CMI guidance for authors of surveys. Clin Microbiol Infect 2016;22:901-2. [Crossref] [PubMed]
Cite this article as: Alp E, Cookson B, Erdem H, Rello J. Infection control bundles in low-middle income countries: an international cross-sectional survey (study protocol). J Emerg Crit Care Med 2018;2:40.