Essential processes of successful trauma systems: template for analysis of trauma systems
Introduction
Organized care of patients with traumatic injuries has advanced dramatically since the inception of the first trauma programs in Illinois, United States of America and Japan in the mid-1960s (1,2). This organized care has largely focused on establishing trauma centers that are now recognized worldwide to produce superior outcomes in patient care (3). Trauma centers now exist in all 50 of the United States and in many other countries throughout the world, each with regional adaptations and variations to suit particular socio-geographic needs. Trauma centers have been the core of trauma systems however defining the ideal or model trauma system has been difficult. There have been numerous papers published on various components of trauma systems such as prehospital care, hospital care transport types and Trauma center designation. Several papers have been published analyzing the systems themselves. Each looking for the “ideal” trauma system which hopefully would then lead to one unified best trauma system. Unfortunately, none of these publications has been able to achieve this goal, often leading to conflicting conclusions on the value of various trauma system elements. The reader is referred to the wildly divergent opinions on helicopter transport as an example (4,5). The recent meta-analysis of trauma systems worldwide by Moore, which was published while we were actively pursuing research on our paper, also failed to identify the ideal system (6). Our working hypothesis was that analysis of large systems many of which have similar elements was likely to produce inconclusive results, if the goal was to identify an ideal or model trauma system. Our premise was that any system with the proper elements or processes would likely yield similar outcomes. We reviewed the literature with an eye towards identifying the common elements or processes present within successful trauma systems. The design of our review was not to establish primacy but rather to define the relative frequency of processes in the trauma literature as a template for a Trauma System. The literature to date has never considered this as a unifying foundation for research into systems design. As such each article tried to imply it was talking about a System or assumed a system when really, they were discussing processes.
Methods
Literature search
A systematic literature search was performed using the United States National Library of Medicine’s PubMed database in October 2017. Works containing at least one of the following terms in their title or abstract were identified: trauma care, trauma system, trauma team, trauma training, trauma team training, Advanced Trauma Life Support (or ATLS®), International Trauma Life Support (or ITLS®), Prehospital Trauma Life Support (or PHTLS®), Advanced Trauma Care for Nurses (or ATCN®), trauma registry, trauma database, injury registry (Supplementary).
Study selection
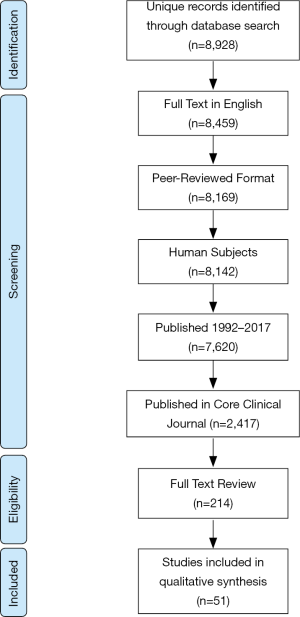
Details regarding study selection are reported in Figure 1. Exclusion criteria were (I) publications not available in English; (II) non-peer-reviewed work; (III) non-human experimental subjects; (IV) studies published prior to January 1, 1992; and (V) non-clinical research. The exclusion criterion regarding publication year was selected to focus this investigation on the modern era of trauma care.
Ultimately, full-text original research studies were included if they reported trauma patient outcomes in association with the implementation of trauma training or trauma system infrastructure. Articles meeting these criteria included case-control and cohort studies, which incorporated prospective and retrospective study designs.
Data collection and quality assessment
Data on the following aspects were extracted from included studies: year of publication, study design (randomized control trial, prospective observational, retrospective), study population (single center or multi-center), sample size, statistical significance of reported outcomes, and subjective assessment of potential bias or confounds.
More specifically, studies assessing the impact of trauma system infrastructure were reviewed for the type of system (pre-hospital, hospital-based or combination), the extent of the system (institutional, state/regional or national), the rationale of the system (mandated or voluntary), the state- or American College of Surgeons-designated level of the system (if applicable), and the reported elements composing the system. Studies investigating the effect of trauma training were similarly reviewed for the training program, the focus of training (pre-hospital or hospital-based), the type of training (individual/skills-based or team), the rationale of the training (mandated or voluntary) and the format of the training.
Results
There were 51 articles that met our initial criterion for inclusion, however the article by Nirula only looked at trauma centers and assumed they represented a trauma system so was excluded on detailed review (7). This left 27 focused on different elements of trauma systems and 25 concentrated on training both individual and team.
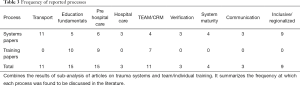
Review of 27 domestic and international research articles on the impact of trauma systems on survival and functional status post injury uncovered several processes common to these systems (Table 1). The most cited reason for a favorable outcome related to timely transport and transfer of critically ill patients to trauma centers, was mentioned in 11 papers (8-18). Timely transport was highly important and included the availability of EMS services by ground or air. System inclusiveness and regionalization was felt to be an important process in nine papers (10,12,13,19-24). Pre-Hospital care was mentioned six times (8,14,21,25-27), and Education that included ATLS® and ongoing refresher courses five times (8,23,28-30). Noted four times were system maturity, (14,19,25,31), and TEAM/CRM training (8,19,29,32). Mentioned 3 times each were: Communication either within the hospital, between EMS and hospital personnel, or between hospital, but largely prehospital (8,15,21), Hospital care (15,26,28), and Formal verification (8,22,32). Interestingly, one of the authors found that even voluntary designation of a trauma center improved patient outcomes (32) (Table 1).
Full table
There were 24 articles reviewed regarding trauma training and care for the trauma patient as a team, these all broadly would fit into education (33-56). Sub-analysis revealed general physician education using ATLS® or ATLS® like courses was noted in seven articles (33,34,47,48,50,52-56), Results as measured by mortality were not consistent with the one Cochrane analysis showing no difference in mortality with ATLS® training (50). Six team training: two RTTDC® (35,36), four other facility based individualized team training including simulation (37-39,56). Sixteen specifically noted System Inclusiveness (34,40-46,48-55), 13 regionalization (33-36,48-56), 7 pre-hospital care (40-46). Transport and communications are part of ATLS®, PTHLS®, ALS®,BLS® and RTTDC® so they also fit these categories 21 times. ATLS® and RTTDC® both allude to some sort of verification but the articles did not stress that point (Table 2).

Full table
There were eleven articles which dealt exclusively with the Advance Trauma Life Support (ATLS®) program and its impact on patient care (33,34,48-56). These articles dealt primarily with care of the trauma patients once they arrived at the hospital, particularly the initial assessment. Two articles reported a decrease in mortality and improved patient outcomes (53,55), while two other articles reported improved outcomes in the first 24 hours, but no improvement in overall mortality (48,49). One article reported an improvement in cognitive performance and a positive impact within the trauma team (54). Three articles referred to alternative standardized training programs for the care of trauma patients, and these articles showed improved patient outcomes, including improved mortality (39,44,47). Three of the eleven articles were systemic reviews and they showed no improvement in mortality, but one of them did comment on improved knowledge, clinical skills, and decision making with ATLS® (34,50,51). One article compared physicians with varying levels of ATLS® training which showed improved patient assessment by physicians with ATLS® exposure (56). This was contradicted by the article from Drimousis, which showed worse outcomes in trauma patients treated by ATLS® certified physicians, but this was done in non-trauma hospitals which lacked some resources typically seen in trauma centers (i.e., CT scanners) and the providing physician was not always a surgeon (52). The article by Vestrup showed no improvements in patient outcomes and had more missed injuries post ATLS® (33).
There were 7 articles that were reviewed that involved prehospital trauma life support (PHTLS) and other pre-hospital support programs (40-46). The outcomes of these articles again showed mixed results regarding patient outcomes, with five of these articles reporting improvements in mortality (40-42). No improvement in mortality was seen in the article by Stiell, but this involved BLS and ALS and not specific trauma training (43). The remaining article by Bowman involved pre-hospital training for the military, specifically for pre-hospital pain medication administration, which there was increased compliance after the training (44). These articles not only highlight the importance of pre-hospital care but also the importance of the pre-hospital staff as an integral part of the trauma team and the need for standardized training for these providers.
The composition of the trauma team varied not only from hospital to hospital, but also from state to state and country to country (38). This fact helps reinforce the need for standardized training for the various types of providers. It also highlights the need for these trauma teams to be comfortable and confident when working with each other. Of the articles reviewed two of them involved training for rural trauma teams and in both instances, there was a decrease in transfer time to a trauma center (35,36). Three articles dealt exclusively with training teams and working together in simulated scenarios and in both articles better communication and improved patient care was reported (37,38,56).
The Frequency a at which the different systems component processes were cited in the literature both for trauma systems papers and trauma training papers is summarized in Table 3. Meta-analysis could not be performed on the individual processes because the definitions varied form paper to paper and the data was poorly reported.
Full table
Discussion
We reasoned that identifying the common Trauma System/Care processes could help developed a template for trauma system design. It was our contention that discrepancies found within the literature may be related to regional modifications of these common elements as well as the erroneous usage of Process outcomes to assess System effectiveness. Moore’s paper listed all the processes found in our analysis but did not reach their research goal of describing the “ideal” trauma system (57). Ironically their data did support, that well-developed systems with common elements or better termed processes all had similar effects. This is to be expected, and as we believe resulted from a misrepresentation of what a system is. Processes have outcomes while Systems are composed of processes that result in an effect (58,59). Therefore if we compare “outcomes” of similar processes in various Systems it should not be surprising to find no difference or diametrically opposed results. This can be illustrated by the helicopter transport debate: Efficiently transporting a patient to a receiving hospital is dependent on time versus severity of the injury. When evaluating types of patient transport, one must consider the environment (rural/mountainous/urban/weather), distance and travel times, and severity of injury. Often the question asked is: “Is helicopter transport important in a trauma system;” trauma center mortality by transport mode is then used a surrogate measurement for transport outcome. It is not surprising that the results show urban systems with an increase in mortality and rural mountainous regions may show an improvement (4,5). The question asked tried to use a System effect (mortality) to measure a process outcome. A better system question would be: Is Helicopter transport necessary for a particular system based on types of expected injuries and ability of ground transport to deliver these patients to the hospital in an acceptable time frame for the best outcome? In our opinion, the use of process outcomes to measure System effectiveness is at the crux of the confusion in the literature. The overarching questions facing Trauma System analysis are: What is an Ideal or Model Trauma System and What should be its effect? The components (processes) of the “Ideal” System would each improve the effectiveness.
Our study identified several common processes in trauma care delivery as measured by mortality and morbidity outcomes (Tables 1 and 2) Using this observational approach, the more common the process is the more it was deemed core to a trauma system (Table 3). There was clear interrelatedness to several of the processes. This may account for some of diametrically opposed statistically significant literature. When analyzing a system thru its individual processes we are dealing with a domino effect. A failure of one process may doom an entire system or an extremely strong process, such as a highly efficient trauma hospital, can overshadow weakness in other areas such as prehospital care. In addition, some components may be inappropriately invalidated by failure to have supporting essential processes. Such as the disparity in the results of ATLS® like courses in outcomes. At least two studies that showed no improvement or worsening in care each study was hampered by no control over EMS or in hospital care (50,52).
System inclusiveness is a somewhat nebulous concept made murkier by the lack of a standardized definition. Several articles credited inclusiveness with improved patient outcomes, collectively describing it as the efficient and timely triage of trauma patients to appropriate sites of care. System inclusiveness requires intra and inter-system communication as in between providers, trauma centers of various level designations, non-trauma hospitals, pre-hospital care teams, etc.; education of trauma care providers; and a hierarchical relationship between area hospitals where injured patients are distributed according to their injury severity. Trauma system inclusiveness seems to occur as a system naturally matures. System maturity implies that patient outcomes improve the longer a trauma system exists. Although once again the concept is poorly defined, it suggests that the mere passage of time correlates to better results. Nevertheless, it is crucial to understand that this depends on conscious actions by the members of a system rather than temporality. More often the system was not evaluated but rather the outcomes at the trauma centers. Mature trauma centers recognize the policies, procedures, and resources that decrease mortality and improve patient care, and prune away those that do not.
Inclusiveness and could be facilitated by regionalization (60). Regionalization implies a trauma system set up to meet the needs of socio-geographic regions thru an organized and regulated process. Regionalization is often voluntary and can be affected by political considerations separate from those directed by patient needs. The states of Illinois and Pennsylvania in the United States have state “Trauma Systems”, however, in each state the number of trauma centers is not mandated nor is a region required to use the trauma centers in its geographic area. As noted in the workshop summary of the Institute of Medicine’s Regionalizing of Emergency Care, “regionalization is not about centralization and it’s not about designating certain facilities as the place to go for anything. It’s about how to structure the utilization of resources in any one location, given that one area will be very different from the next. The aim… is to get the right resources to the right patient at the right time, which may not even involve moving the patient. It can also mean moving resources, personnel, or simply knowledge” (61). Prehospital care is any care a patient receives prior to admission to a trauma center. The details of this topic were poorly addressed but involved EMS and transport to trauma centers.
Verification was an interesting process to review. There are NO verification programs for trauma systems only for trauma centers. When discussing verification of trauma centers there is even more variability as no one verification program exists. In the example above of Pennsylvania and Illinois these states have state mandated verification programs that are distinct from the Trauma Verification Program of the American College of Surgeons®, while Australia and Japan have their own process. What can be said about these verification programs is that they try to analyze how trauma care processes interact to effect care. Therefore, a verification process may not be an essential component in and of itself but maybe seen to monitor whether a system has good and effective processes.
We were particularly interested in the impact of training and education either as an individual or team was a common core element. Observationally it seemed obvious that every process must have an educational component and we wondered if that may be one of the confounders in discerning differences in outcome. The articles on training varied on their opinions about whether standardized training provided any benefit to patient care and outcomes. This can potentially be explained by the inability to measure the effect of training when combined with variations in how the training is applied.
A unifying element of all medical systems was team cohesiveness and that may be achieved best by educational programs. Therefore, solid educational programs that support interdependence and communication within a system may be the single most important factor in developing a trauma system.
The laudable goal of the Meta- analysis performed by the international group headed by Lynne Moore was to help health care planners in allocating resources to Trauma Systems (6). We agree whole heartedly with their conclusion that: “Future research should …aim to…understand (the) interplay between the components of trauma systems” We propose that a Trauma System should be one that contains the common processes identified by the literature. The Effect of a Trauma System is to identify and treat injured patients in the most efficient way to obtain a favorable outcome for each patient. One may argue that this is an Objective and therefore not testable. That is correct. However, one can define individual processes that impact the effect and these can be measured. The sum of these processes results in the effect. The National Conference of State Legislators in the USA stated the “Effect” of Trauma systems this way: “The Right Patient, The Right Place, The Right Time.” (62). Nowak in his article on Patient flow within a medical center also echoed this: “right care, right time, right place” (63). The paper by Brink drew conclusions that echo our findings and presents another summary of an “Ideal” Trauma system (see Table 1) (28). We hope that our paper will serve as a template for analyzing the effect of the group of processes interacting in a trauma system. We believe that trauma systems should all contain the same common processes but be tailored to the individual needs of the region served (55,64). A good example of this approach can be seen in the adaptation of ATLS® by TEAM Broken Earth® and the novel team training done in Hangzhou, China (38,65). A Google search using the phrase “trauma systems in the United States” only yields articles relating to trauma centers which are one of the processes of a system. Even in the United States of America, arguably the birth place of modern trauma care, there is no one trauma center verification program (66).
Weaknesses
Our study has several weaknesses. As with any descriptive study, there is always a potential for selection bias that can be introduced. This is compounded by selecting only papers written in English. Given the premise of our paper that the current literature had erroneously confused process outcomes with system effectiveness, there was often shared bias between articles reviewed especially when the same author had written several papers on different aspects of the trauma care delivery. We believe our paper does help shed light one of the difficulties of trauma system analysis; that being not confusing process outcome with effect.
Conclusions
The results of our study show that defining an ideal system should not be confused with analyzing the processed within a care delivery system. Individual processes should be analyzed with a view towards how they contribute to the effect of the system they support. A system’s effect must be clearly defined. We suggest Nowak’s definition of “Right Care to the Right Place at the Right time” as care of the injured patient starts once he/she is identified (63). Outcomes of each the processes that support a System would be judged based on how they supported this effect. This would mean for planners that they should concentrate on building systems with the core processes mentioned above. Resources could be allocated as needed in a step-wise fashion depending on where the needs of the current care delivery system were most acute. An underdeveloped country may wish to start with education while a more developed one may wish to tackle the political hurdle of mandated regionalization. We suggest that further research be careful to not mix system analysis with process analysis and be cognizant that components of processes (transport vehicles/care). Trauma systems and the processes that support them cannot be separated from the socio-geographic-culture in which they function.
Acknowledgements
Marie Hunsinger, Senior Research Coordinator Surgical Institute, Geisinger Health System. The Asian Society for Emergency and Critical Care Medicine for the inviting this paper. The authors thank Marie Hunsinger for administrative support.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This research was approved by the Geisinger Health System IRB as an Exempted Literature Review Study.
References
- Trunkey DD. History and development of trauma care in the United States. Clin Orthop Relat Res 2000.36-46. [Crossref] [PubMed]
- Tanaka T, Kitamura N, Shindo M. Trauma care systems in Japan. Injury 2003;34:699-703. [Crossref] [PubMed]
- Celso B, Tepas J, Langland-Orban B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma 2006;60:371,8; discussion 378.
- Thomas SH, Harrison TH, Buras WR, et al. Helicopter transport and blunt trauma mortality: a multicenter trial. J Trauma 2002;52:136-45. [Crossref] [PubMed]
- Schiller WR, Knox R, Zinnecker H, et al. Effect of helicopter transport of trauma victims on survival in an urban trauma center. J Trauma 1988;28:1127-34. [Crossref] [PubMed]
- Moore L, Champion H, Tardif PA, et al. Impact of Trauma System Structure on Injury Outcomes: A Systematic Review and Meta-Analysis. World J Surg 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Nirula R, Brasel K. Do trauma centers improve functional outcomes: a national trauma databank analysis? J Trauma 2006;61:268-71. [Crossref] [PubMed]
- McDermott FT, Cordner SM, Cooper DJ, et al. Management deficiencies and death preventability of road traffic fatalities before and after a new trauma care system in Victoria, Australia. J Trauma 2007;63:331-8. [Crossref] [PubMed]
- Härtl R, Gerber LM, Iacono L, et al. Direct transport within an organized state trauma system reduces mortality in patients with severe traumatic brain injury. J Trauma 2006;60:1250-6; discussion 1256. [Crossref] [PubMed]
- Mckee JL, Roberts DJ, van Wijngaarden-Stephens MH, et al. The right treatment at the right time in the right place: a population-based, before-and-after study of outcomes associated with implementation of an all-inclusive trauma system in a large Canadian province. Ann Surg 2015;261:558-64. [Crossref] [PubMed]
- Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA 1994;271:1919-24. [Crossref] [PubMed]
- Twijnstra MJ, Moons KG, Simmermacher RK, et al. Regional trauma system reduces mortality and changes admission rates: a before and after study. Ann Surg 2010;251:339-43. [Crossref] [PubMed]
- Barquist E, Pizzutiello M, Tian L, et al. Effect of trauma system maturation on mortality rates in patients with blunt injuries in the Finger Lakes Region of New York State. J Trauma 2000;49:63-9; discussion 69-70. [Crossref] [PubMed]
- Tallon JM, Fell DB, Ackroyd-Stolarz S, et al. Influence of a new province-wide trauma system on motor vehicle trauma care and mortality. J Trauma 2006;60:548-52. [Crossref] [PubMed]
- Gerndt SJ, Conley JL, Lowell MJ, et al. Prehospital classification combined with an in-hospital trauma radio system response reduces cost and duration of evaluation of the injured patient. Surgery 1995;118:789-94; discussion 794-6. [Crossref] [PubMed]
- Brink JA, Allen CF, Goslar PW, et al. Can we improve trauma mortality in a state with a voluntary trauma system. Am J Surg 2001;182:738-42. [Crossref] [PubMed]
- Porter A, Wyrick D, Bowman SM, et al. The effectiveness of a statewide trauma call center in reducing time to definitive care for severely injured patients. J Trauma Acute Care Surg. 2014;76:907-11; discussion 911-2. [Crossref] [PubMed]
- Hulka F, Mullins RJ, Mann NC, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Trauma 1997;42:514-9. [Crossref] [PubMed]
- Maggio PM, Brundage SI, Hernandez-Boussard T, et al. Commitment to COT verification improves patient outcomes and financial performance. J Trauma 2009;67:190-4; discussion 194-5. [Crossref] [PubMed]
- He JC, Kreiner LA, Sajankila N, et al. Performance of a regional trauma network: A state-wide analysis. J Trauma Acute Care Surg 2016;81:190-5. [Crossref] [PubMed]
- Utter GH, Maier RV, Rivara FP, et al. Inclusive trauma systems: do they improve triage or outcomes of the severely injured? J Trauma 2006;60:529-35; discussion 535-37. [Crossref] [PubMed]
- Gabbe BJ, Simpson PM, Sutherland AM, et al. Improved functional outcomes for major trauma patients in a regionalized, inclusive trauma system. Ann Surg 2012;255:1009-15. [Crossref] [PubMed]
- Leung GK, Chang A, Cheung FC, et al. The first 5 years since trauma center designation in the Hong Kong Special Administrative Region, People's Republic of China. J Trauma 2011;70:1128-33. [Crossref] [PubMed]
- Kelly ML, Banerjee A, Nowak M, et al. Decreased mortality in traumatic brain injury following regionalization across hospital systems. J Trauma Acute Care Surg 2015;78:715-20. [Crossref] [PubMed]
- Marson AC, Thomson JC. The influence of prehospital trauma care on motor vehicle crash mortality. J Trauma 2001;50:917-20; discussion 920-1. [Crossref] [PubMed]
- Gabbe BJ, Biostat GD, Lecky FE, et al. The effect of an organized trauma system on mortality in major trauma involving serious head injury: a comparison of the United kingdom and victoria, australia. Ann Surg 2011;253:138-43. [Crossref] [PubMed]
- Esposito TJ, Sanddal TL, Reynolds SA, et al. Effect of a voluntary trauma system on preventable death and inappropriate care in a rural state. J Trauma 2003;54:663-9; discussion 669-70. [Crossref] [PubMed]
- Olson CJ, Arthur M, Mullins RJ, et al. Influence of trauma system implementation on process of care delivered to seriously injured patients in rural trauma centers. Surgery 2001;130:273-9. [Crossref] [PubMed]
- Groven S, Eken T, Skaga NO, et al. Long-lasting performance improvement after formalization of a dedicated trauma service. J Trauma 2011;70:569-74. [Crossref] [PubMed]
- Murphy EE, Murphy SG, Cipolle MD, et al. The pediatric trauma center and the inclusive trauma system: Impact on splenectomy rates. J Trauma Acute Care Surg 2015;78:930-3; discussion 933-4. [Crossref] [PubMed]
- He JC, Kreiner LA, Sajankila N, et al. Performance of a regional trauma network: A state-wide analysis. J Trauma Acute Care Surg 2016;81:190-5. [Crossref] [PubMed]
- Simons R, Kasic S, Kirkpatrick A, et al. Relative importance of designation and accreditation of trauma centers during evolution of a regional trauma system. J Trauma 2002;52:827-33; discussion 833-4. [Crossref] [PubMed]
- Vestrup JA, Stormorken A, Wood V. Impact of advanced trauma life support training on early trauma management. Am J Surg 1988;155:704-7. [Crossref] [PubMed]
- Mohammad A, Branicki F, Abu-Zidan FM. Educational and clinical impact of Advanced Trauma Life Support (ATLS®) courses: a systematic review. World J Surg 2014;38:322-9. [Crossref] [PubMed]
- Dennis BM, Vella MA, Gunter OL, et al. Rural Trauma Team Development Course decreases time to transfer for trauma patients. J Trauma Acute Care Surg 2016;81:632-7. [Crossref] [PubMed]
- Malekpour M, Neuhaus N, Martin D, et al. Changes in rural trauma prehospital times following the Rural Trauma Team Development Course training. Am J Surg 2017;213:399-404. [Crossref] [PubMed]
- Capella J, Smith S, Philp A, et al. Teamwork training improves the clinical care of trauma patients. J Surg Educ 2010;67:439-43. [Crossref] [PubMed]
- Hong Y, Cai X. Effect of team training on efficiency of trauma care in a Chinese hospital. J Int Med Res 2018;46:357-67. [Crossref] [PubMed]
- Siriratsivawong K, Kang J, Riffenburgh R, et al. Immersion team training in a realistic environment improves team performance in trauma resuscitation. Surgery 2016;160:586-90. [Crossref] [PubMed]
- Arreola-Risa C, Mock CN, Padilla D, et al. Trauma care systems in urban Latin America: the priorities should be prehospital and emergency room management. J Trauma 1995;39:457-62. [Crossref] [PubMed]
- Blomberg H, Svennblad B, Michaelsson K, et al. Prehospital trauma life support training of ambulance caregivers and the outcomes of traffic-injury victims in Sweden. J Am Coll Surg 2013;217:1010-9.e1-2.
- Johansson J, Blomberg H, Svennblad B, et al. Prehospital Trauma Life Support (PHTLS) training of ambulance caregivers and impact on survival of trauma victims. Resuscitation 2012;83:1259-64. [Crossref] [PubMed]
- Stiell IG, Nesbitt LP, Pickett W, et al. The OPALS Major Trauma Study: impact of advanced life-support on survival and morbidity. CMAJ 2008;178:1141-52. [Crossref] [PubMed]
- Bowman SM, Sharar SR, Quan L. Impact of a statewide quality improvement initiative in improving the management of pediatric splenic injuries in washington state. J Trauma 2008;64:1478-83. [Crossref] [PubMed]
- Ali J, Adam RU, Gana TJ, et al. Effect of the prehospital trauma life support program (PHTLS) on prehospital trauma care. J Trauma 1997;42:786-90. [Crossref] [PubMed]
- Ali J, Adam RU, Gana TJ, et al. Trauma patient outcome after the Prehospital Trauma Life Support program. J Trauma 1997;42:1018-21; discussion 1021-2. [Crossref] [PubMed]
- Hondo K, Shiraishi A, Fujie S, et al. In-hospital trauma mortality has decreased in Japan possibly due to trauma education. J Am Coll Surg 2013;217:850-7.e1. [Crossref] [PubMed]
- van Olden GD, Meeuwis JD, Bolhuis HW, et al. Clinical impact of advanced trauma life support. Am J Emerg Med 2004;22:522-5. [Crossref] [PubMed]
- Magnone S, Allegri A, Belotti E, et al. Impact of ATLS® guidelines, trauma team introduction, and 24-hour mortality due to severe trauma in a busy, metropolitan Italian hospital: A case control study. Ulus Travma Acil Cerrahi Derg 2016;22:242-6. [PubMed]
- Jayaraman S, Sethi D. Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev 2009.CD004173. [PubMed]
- Jayaraman S, Sethi D, Wong R. Advanced training in trauma life support for ambulance crews. Cochrane Database Syst Rev 2014.CD003109. [PubMed]
- Drimousis PG, Theodorou D, Toutouzas K, et al. Advanced Trauma Life Support certified physicians in a non trauma system setting: is it enough? Resuscitation 2011;82:180-4. [Crossref] [PubMed]
- Ali J, Adam R, Butler AK, et al. Trauma outcome improves following the advanced trauma life support program in a developing country. J Trauma 1993;34:890-8; discussion 898-9. [Crossref] [PubMed]
- Ali J, Adam R, Stedman M, et al. Cognitive and attitudinal impact of the Advanced Trauma Life Support program in a developing country. J Trauma 1994;36:695-702. [Crossref] [PubMed]
- Adam R, Stedman M, Winn J, et al. Improving trauma care in Trinidad and Tobago. West Indian Med J 1994;43:36-8. [PubMed]
- Williams MJ, Lockey AS, Culshaw MC. Improved trauma management with advanced trauma life support (ATLS®) training. J Accid Emerg Med 1997;14:81-3. [Crossref] [PubMed]
- Moore L, Lavoie A, Sirois MJ, et al. A comparison of methods to obtain a composite performance indicator for evaluating clinical processes in trauma care. J Trauma Acute Care Surg 2013;74:1344-50. [Crossref] [PubMed]
- Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care 2006;15 Suppl 1:i50-8. [Crossref] [PubMed]
- Reemtsma K, Morgan M. Outcomes assessment: a primer. Bull Am Coll Surg 1997;82:34-9. [PubMed]
- Vali Y, Rashidian A, Jalili M, et al. Effectiveness of regionalization of trauma care services: a systematic review. Public Health 2017;146:92-107. [Crossref] [PubMed]
- Regionalizing Emergency Care: Workshop Summary. Washington DC: The National Academies Press, 2010.
- Hendrikson H PW. The Right Patient, The Right Palce, The Rigtht Time. Denver Colorado: National Conference of State Legislators, 2012.
- Nowak NA, Rimmasch H, Kirby A, et al. Right care, right time, right place, every time. Healthc Financ Manage 2012;66:82-8. [PubMed]
- Bergman S, Deckelbaum D, Lett R, et al. Assessing the impact of the trauma team training program in Tanzania. J Trauma 2008;65:879-83. [Crossref] [PubMed]
- Kurdin A, Caines A, Boone D, et al. TEAM: A Low-Cost Alternative to ATLS® for Providing Trauma Care Teaching in Haiti. J Surg Educ 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Ziran BH, Barrette-Grischow MK, Hileman B. United States level I trauma centers are not created equal – a concern for patient safety? Patient Saf Surg 2008;2:18. [Crossref] [PubMed]
Cite this article as: Gregory JS, Walker C, Young K, Ralchenko A. Essential processes of successful trauma systems: template for analysis of trauma systems. J Emerg Crit Care Med 2018;2:22.