The effect of early mobilization for critical ill patients requiring mechanical ventilation: a systematic review and meta-analysis
Introduction
With the treatment measures in intensive care unit (ICU), more and more critically ill patients survived and discharged from hospital. The increasing rate of survivors in the ICU brings a new problem: recent studies of recovery after ICU found that many survivors of ICU suffer long-term poor physical and psychological outcomes associated with the ICU experience (1,2). For critical ill patients undergoing mechanical ventilation (MV) in ICU, it is common to keep complete or nearly complete limb immobilization. The muscle inactivity has been proved to be an important risk factor for intensive care unit-acquired weakness (ICU-AW) (3). And the ICU-AW tends to extend the duration of MV, prolong the length of ICU and hospital stay, increase the risk of mortality at hospital discharge (4,5).
A widely accepted definition of early mobilization is the application of physical activity within the first 2 to 5 days of critical illness or injury (6). The safety consideration used to be a major barrier to generalize the early mobilization in clinical practice (7). But recent systematic reviews and meta-analysis have proved conclusively that early mobilization for ICU patients is safe, with low incidence of adverse events (8,9).The application of early mobilization for patients could maintain the muscle strength and improve physical function (6). For this reason, we can infer that early mobilization could have positive effect on hospital outcomes like increasing the weaning success rate, decreasing the duration of MV, shortening the length of stay (LOS) in ICU and hospital. Previous meta-analysis pointed out the early mobilization appears to have benefit in improving hospital outcomes and quality of life (10,11).
And in recent years, there are increasing number of new studies and researches about early mobilization, an update meta-analysis based on high quality studies and focusing on the effectiveness of early mobilization is quite necessary. Hence, the purpose of this meta-analysis was to explore the effect of early mobilization for critical ill patients on duration of MV, ICU and hospital LOS, patient mortality at hospital discharge.
Methods
Inclusion criteria
The studies fulfilled all of the criteria would be included: (I) the patients enrolled should be adults (at least 18 years old), and they were mechanically ventilated in any type of ICU; (II) the study should be the randomized controlled trial (RCT), cohort study or other comparative study with concurrent controls; (III) the intervention should be mobilization, active or passive exercise such as stretching exercises in-bed, bedside sitting training, bed to chair transferring and walking training; (IV) the control group should receive standard medical and nursing therapy. Exclusion criteria: (I) animal studies; (II) the patients are minors (under 18 years of age); (IV) studies haven’t reported the concerned outcomes.
Outcome
Primary outcomes are the ICU and hospital LOS, the duration of MV. Secondary outcome is the mortality at hospital discharge.
Search strategy
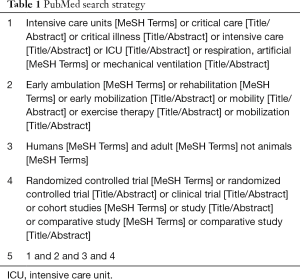
We searched the electronic databases of PubMed, Scopus, EBSCO and Embase from the earliest available date until November 2017. We designed a search strategy for PubMed and the detailed search strategy is included in the Table 1. There is no restrictions in language.
Full table
Study selection
Two authors independently conducted the initial search and selection by reading the titles and abstracts. And potential relevant studies were further checked based on the inclusion criteria previously described. All these review authors conducted searches and evaluated the full text of each record independently. Differences in assessment screening were resolved by a third opinion.
Data extraction
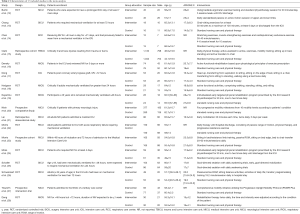
The data extraction was accomplished independently by three authors by using a predesigned data extraction form (Table 2). If the data was incomplete or needed further details, review authors would send e-mails to the article author for clarification of results. The primary study end points of included studies were the ICU and hospital LOS, the duration of MV. The secondary study end point was the mortality at hospital discharge. Relevant information such as the Acute Physiology and Chronic Health Evaluation (APACHE) II Score, patients enrollment and interventions were abstracted from original articles.
Full table
Quality assessment
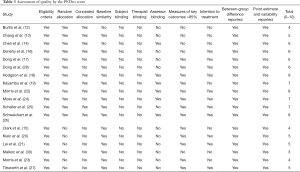
The risk of bias for these included studies were independently assessed by two authors. The Physiotherapy Evidence Database (PEDro) scale (29) was used in the quality assessment. We assessed every potential source of bias as “yes” or “no” according to the articles, every “yes” got 1 point and “no” got 0 point. Finally, a score out of 10 was obtained and a higher score showing high quality trials. We also made a “Assessment of quality by the PEDro score” (Table 3) to show the quality assessment result.
Full table
Statistical analysis
We used the Review Manager 5.3 to implement the meta-analysis. For the primary outcomes, we reported mean difference (MD) between groups and 95% CI in the article. And the mortality at hospital discharge was reported by odds ratio (OR) and 95% CI. To investigate the potential publication bias, we used the Begg’s rank correlation test and the Egger’s regression test in the study (31). The I2 statistic was calculated to evaluate the heterogeneity between studies and we could conclude substantial heterogeneity when I2≥50% (32). Due to the obvious heterogeneity, we performed subgroup analysis stratified by ethnic group, mean age, mean APACHE II Score, and disease groups to explore the potential contributing factors. In addition, we conducted a sensitivity analysis to find out the influence of one study on the overall risk.
Results
Study selection
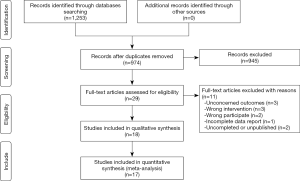
Our initial search identified 1,253 potentially relevant articles from electronic databases and no further articles were included from other sources, of which 17 studies (12-28) of early mobilization in the ICU were finally included. Within the 17 studies, there are 12 RCTs (12-14,16-19,22,24-26,28) and 5 observational study (15,20,21,23,27). The selection process was presented in the Figure 1. These studies were published from 2008 to 2016. Some important characteristics of included articles were showed in Table 2. Of the 17 studies, the sample size ranged from 27 to 2,176, and the mean age ranged between 50 and 70 years. The APACHE II score had no statistical difference between the intervention and control group in included studies.
Risk of bias assessment
The risk of bias assessment was outlined in Table 3. Ten RCTs (14,16-19,22,24-26,28) had good quality and tiny bias with the scores ranged 6 to 8. One historical controlled study (30) had a high risk of bias so we excluded it. Other studies’ (12,13,15,20,21,23,27) bias assessment scores ranged 4 to 5. All included studies had eligibility criteria for the included patients, reported between-group difference, measured point estimate and variability. But subject blinding and therapist blinding were impossible to implement for these studies. All the RCTs were random allocated while three trials (17,24,28) didn’t reported whether the allocation was concealed. Six RCTs (14,18,19,22,24,26) had assessor blinding and eight RCTs (17-19,22,24-26,28) had measured the key outcomes >85% subjects after allocation. For the observational studies (15,20,21,23,27,30), the scores ranged from 3 to 5. These studies didn’t have random or concealed allocation, and the assessor blinding were not mentioned.
Sensitivity and subgroup analysis
We found substantial heterogeneity among studies of LOS in ICU and hospital. Our sensitivity analyses for included RCTs (Figure 2) suggested that one study (17) might contribute to the heterogeneity. The study’s participants were patients who had been operated coronary artery bypass surgery. The highly similarities of patients’ disease types between the intervention and control group in the study would overestimate the effect of early mobilization and we decided to exclude the study.
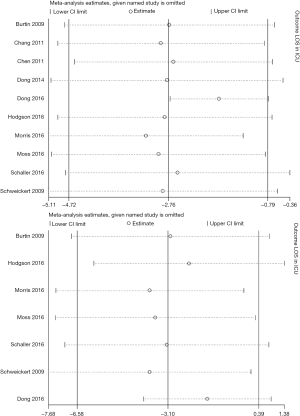
We also did the subgroup analyses stratified by ethnic group, mean age, mean APACHE II Score and cause of ICU stay, and the heterogeneity disappeared when we divided the studies into three subgroups by the participants’ disease types. Thus, the different kinds of diseases are the source of heterogeneity among included studies. We also compared the difference between the RCTs and observational studies in the effect of early mobilization.
Hospital outcomes
Nine RCTs (12-14,18,22,24-26,28) and four observational studies (15,20,21,23) provided the LOS in ICU and we used a fixed effects model to analyse the data (P=0.43, I2=1%). The LOS in ICU had a significant reduction in intervention group MD =−1.75, 95% CI: −2.70 to −0.79; P=0.0003, Figure S1). There are four observation studies (15,20,21,23) recorded the LOS in ICU and we used a random model to compare the difference between RCTs and observation (Figure S2). We found the decrease in the observational group is more obvious. Through subgroup analysis for included RCTs, the impact of early mobilization for patients in respiratory intensive care unit (RICU) is lower than other groups (Figure S3).
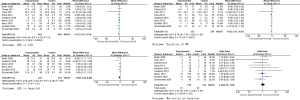
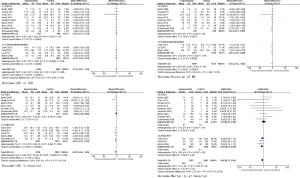
Eight RCTs (12-14,18,24-26,28) reported data for the duration of MV measured in number of days with data pooled using a fixed effects model (P=0.46, I2 =0%). Through analyzing the results we found the duration of MV was significant shortened in intervention group (MD =−1.64, 95%: CI −2.41 to −0.87; P<0.0001, Figure S1). Three observation studies (15,21,23) also reported the data and the result (MD =−1.64, 95% CI: −2.59 to −0.68; P=0.008, Figure S2) had no statistical difference with the RCTs.
Six RCTs (12,18,22,24-26) and five observational studies (15,20,21,23,27) provided the LOS in hospital data and we used a random effects model to pool the data (P<0.00001, I2 =82%). By analyzing the data from RCTs, we found there is no statistical difference in patient’s hospital LOS between the intervention and control group (MD =−1.58, 95% CI: −4.02 to 0.86; P=0.21, Figure S1). But observation studies discovered the early mobilization could shorten the LOS in hospital (MD =−3.87, 95% CI: −5.23 to −2.51; P<0.00001, Figure S2). The subgroup analysis found the early mobilization for the patients in surgery intensive care unit (SICU) or RICU couldn’t evidently decrease the LOS in hospital, but medical intensive care unit (MICU) patients’ hospital LOS was obviously reduced (Figure S3).
Nine RCTs (12,14,16,18,19,22,25,26,28) provided hospital mortality data and we used a fixed effects model to pool the data (P=0.49, I2=0%). According to the analytical result (OR =1.10, 95% CI: 0.76 to 1.59; P=0.62, Figure S1), there is no statistical difference in mortality risk between the intervention and control group. However, the observation studies (15,20,23) demonstrated that early mobilization could slightly decrease the mortality risk in the intervention group (OR =0.80, 95% CI: 0.65 to 0.99; P=0.04, Figure S2). The subgroup analysis found early mobilization might increase the hospital mortality for the patients in SICU (OR =1.98, 95% CI: 1.00 to 3.91; P=0.05, Figure S3).
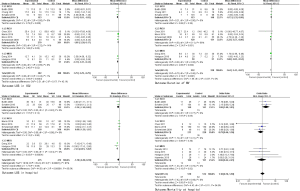
Publication bias
Visual inspection of the Begg’s funnel plot did not find substantial asymmetry (Figure 3). For the LOS in ICU, Egger’s test showed 0.776 and Begg’s test showed 0.260. For the LOS in hospital, Egger’s test showed 0.139 and Begg’s test showed 0.537. For the duration of MV, Egger’s test showed 0.242 and Begg’s test showed 0.951. For the mortality at hospital discharge, Egger’s test showed 0.689 and Begg’s test showed 0.837. There was no evidence of publication bias among included studies.
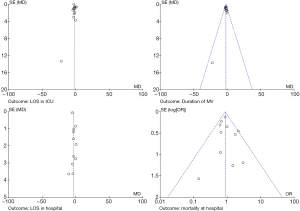
Publication bias assessed by funnel plot. Publication bias was assessed using the effect size of OR of hospital mortality, weighted mean difference of the hospital LOS, ICU, LOS and duration of MV. The results showed that there was no potential publication bias in the present analysis. OR, odds ratio; LOS, length of stay; ICU, intensive care unit; LOS, length of stay.
Discussion
This meta-analysis synthesized data from 1,837 intervention group patients and 1,579 control group patients, described an assessment of early mobilization intervention on hospital outcomes. We found that early mobilization therapy for patients receiving MV in ICU had a positive effect on hospital outcomes such as decreasing the LOS in ICU and reducing the duration of MV. And early mobilization therapy in ICU appears to be safe and did not increase mortality at hospital discharge in research settings.
There is a widely accepted consensus that patients undergoing MV in ICU for prolonged periods of time and are likely to have weak muscle strength. The prolonged immobilization and bed ridden take an important part in the ICU-acquired weakness. The early mobilization therapy for critical ill patients could prevent muscle atrophy, enhance muscle force and better muscle coordination. With the benefits of early mobilization therapy, patients could improve functional status with lower MV demands and increase the weaning rate (33). In the meta-analysis, eight RCTs (12-14,18,24-26,28) and three observation studies (15,21,23) compared the duration of MV in intervention group with control group. The duration of MV was consistently shorter in patients receiving early mobilization therapy. These improvements could also possibly shorten the LOS in ICU and hospital. By analyzing the data from included studies (12-14,18,22,24-26,28), for the patients in intervention group, the LOS in ICU had a significant reduction but there was no statistical for the LOS in hospital. And improving muscle function is a long-term process so it might not have instant positive influence on the mortality rate. The comparison of hospital mortality risk between intervention and control group demonstrated that early mobilization had no significant positive or negative effect on hospital mortality.
Our subgroup analysis demonstrated that difference disease and ICU types may have potential influence on the outcomes (Figure S3). For the surgical patients in SICU, the hospital mortality in intervention group had distinctly increased. That demonstrated early mobilization therapy should be more careful and adjust the protocol by the patients’ wounds and illness, some improper mobilization therapy will lead to adverse events or mortality. For the patients without respiratory system diseases, the impact of reducing the LOS in ICU and hospital is more significant than the RICU patients with respiratory system diseases. And different study design also had effect on the outcomes (Figure S2), the observational studies tend to report over-rated results compared with the RCTs. Especially for the hospital mortality, three observation studies (15,20,23) found early mobilization could decrease the mortality rates while the RCTs suggested there was no statistical difference between intervention and control group.
Similarly, a recent study in pediatric intensive care unit (PICU) found that the early mobilization is safe and beneficial like improving the functional status and decreasing the LOS in PICU (34). Engel et al. (35) found that early mobilization could significantly improve the physical and neurocognitive outcomes. Tipping et al. (9) proved conclusively that early mobilization for ICU patients is safe. Our study pays specific attention to the effect of early mobilization in ICU with quantitative results and included five up-to-date studies (18,21,22,24,25). And the subgroup analysis demonstrated that difference disease and ICU types may have potential influence on the clinic outcomes. Finally, we reported the differentia between the RCTs evidence and observational studies evidence.
Study strengths and limitations
The study strengths stem from the clear, targeted inclusion and exclusion criteria, credibility in the data extraction and analysis, comprehensive sensitivity and subgroup analyses. Five of the studies (18,21,22,24,25) included in this study are newly published and have good quality with low risk of bias. Our subgroup analysis found that different disease group may be an influence factor on the outcomes and observational studies might over-rated the effect of early mobilization.
Weakness include there are six (12-14,18,19,28) of the included studies with small sample size (n<100), which may cause small-study effects and tend to report larger beneficial effects (36). In subgroup analysis, there were only two studies in the minimal subgroup and therefore it might cause some bias. The intensity and amount of early mobilization therapy for the intervention group in different studies were manifold and some specific factual information was unavailable, that limited the subgroup analysis in this meta-analysis.
Conclusions
The early mobilization for critical ill patients undergoing MV in ICU can improve hospital outcomes like shortening the duration of MV, decreasing the LOS in ICU. The result also suggests the early mobilization therapy is safe and won’t increase the mortality at hospital discharge.
Further study should determine the effect of different early mobilization protocol for critical ill patients. More specific studies should be assessed to find out the most effective and safe mobilization protocols.
Acknowledgements
The study was registered in PROSPERO (http://www.crd.york.ac.uk/PROSPERO/) under registration number CRD 42017079190.
Funding: This work was supported in part by grant from the National Natural Science Foundation of China (No. 81570017, GS Zhang)
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med 2011;39:371-9. [Crossref] [PubMed]
- Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med 2012;40:502-9. [Crossref] [PubMed]
- de Jonghe B, Lacherade J, Sharshar T, et al. Intensive care unit-acquired weakness: risk factors and prevention. Crit Care Med 2009;37:S309-15. [Crossref] [PubMed]
- De Jonghe B, Sharshar T, Lefaucheur JP, et al. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA 2002;288:2859-67. [Crossref] [PubMed]
- Ali NA, O'Brien JM Jr, Hoffmann SP, et al. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med 2008;178:261-8. [Crossref] [PubMed]
- Hodgson CL, Berney S, Harrold M, et al. Clinical review: early patient mobilization in the ICU. Crit Care 2013;17:207. [Crossref] [PubMed]
- Bakhru RN, McWilliams DJ, Wiebe DJ, et al. Intensive Care Unit Structure Variation and Implications for Early Mobilization Practices. An International Survey. Ann Am Thorac Soc 2016;13:1527-37. [Crossref] [PubMed]
- Nydahl P, Sricharoenchai T, Chandra S, et al. Safety of Patient Mobilization and Rehabilitation in the Intensive Care Unit. Systematic Review with Meta-Analysis. Ann Am Thorac Soc 2017;14:766-77. [Crossref] [PubMed]
- Tipping CJ, Harrold M, Holland A, et al. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med 2017;43:171-83. [Crossref] [PubMed]
- Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Critical Care Medicine 2013;41:1543-54. [Crossref] [PubMed]
- Li Z, Peng X, Zhu B, et al. Active mobilization for mechanically ventilated patients: a systematic review. Arch Phys Med Rehabil 2013;94:551-61. [Crossref] [PubMed]
- Burtin C, Clerckx B, Robbeets C, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med 2009;37:2499-505. [Crossref] [PubMed]
- Chang MY, Chang LY, Huang YC, et al. Chair-sitting exercise intervention does not improve respiratory muscle function in mechanically ventilated intensive care unit patients. Respir Care 2011;56:1533-8. [Crossref] [PubMed]
- Chen YH, Lin HL, Hsiao HF, et al. Effects of exercise training on pulmonary mechanics and functional status in patients with prolonged mechanical ventilation. Respir Care 2012;57:727-34. [Crossref] [PubMed]
- Clark DE, Lowman JD, Griffin RL, et al. Effectiveness of an early mobilization protocol in a trauma and burns intensive care unit: a retrospective cohort study. Phys Ther 2013;93:186-96. [Crossref] [PubMed]
- Denehy L, Skinner E, Edbrooke L, et al. Exercise rehabilitation for patients with critical illness: a randomized controlled trial with 12 months of follow-up. Crit Care 2013;17:R156. [Crossref] [PubMed]
- Dong Z, Yu B, Zhang Q, et al. Early Rehabilitation Therapy Is Beneficial for Patients With Prolonged Mechanical Ventilation After Coronary Artery Bypass Surgery. Int Heart J 2016;57:241. [Crossref] [PubMed]
- Hodgson CL, Bailey M, Bellomo R, et al. A Binational Multicenter Pilot Feasibility Randomized Controlled Trial of Early Goal-Directed Mobilization in the ICU. Crit Care Med 2016;44:1145-52. [Crossref] [PubMed]
- Kayambu G, Boots R, Paratz J. Early physical rehabilitation in intensive care patients with sepsis syndromes: a pilot randomised controlled trial. Intensive Care Med 2015;41:865-74. [Crossref] [PubMed]
- Klein K, Mulkey M, Bena JF, et al. Clinical and psychological effects of early mobilization in patients treated in a neurologic ICU: a comparative study. Crit Care Med 2015;43:865-73. [Crossref] [PubMed]
- Lai CC, Chou W, Chan KS, et al. Early Mobilization Reduces Duration of Mechanical Ventilation and Intensive Care Unit Stay in Patients With Acute Respiratory Failure. Arch Phys Med Rehabil 2017;98:931-9. [Crossref] [PubMed]
- Morris PE, Berry MJ, Files DC, et al. Standardized Rehabilitation and Hospital Length of Stay Among Patients With Acute Respiratory Failure: A Randomized Clinical Trial. JAMA 2016;315:2694-702. [Crossref] [PubMed]
- Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med 2008;36:2238-43. [Crossref] [PubMed]
- Moss M, Nordon-Craft A, Malone D, et al. A Randomized Trial of an Intensive Physical Therapy Program for Patients with Acute Respiratory Failure. Am J Respir Crit Care Med 2016;193:1101-10. [Crossref] [PubMed]
- Schaller SJ, Anstey M, Blobner M, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 2016;388:1377-88. [Crossref] [PubMed]
- Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009;373:1874-82. [Crossref] [PubMed]
- Titsworth WL, Hester J, Correia T, et al. The effect of increased mobility on morbidity in the neurointensive care unit. J Neurosurg 2012;116:1379-88. [Crossref] [PubMed]
- Dong ZH, Yu BX, Sun YB, et al. Effects of early rehabilitation therapy on patients with mechanical ventilation. World J Emerg Med 2014;5:48. [Crossref] [PubMed]
- Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 2003;83:713-21. [PubMed]
- Malkoç M, Karadibak D, Yildirim Y. The effect of physiotherapy on ventilatory dependency and the length of stay in an intensive care unit. Int J Rehabil Res 2009;32:85-8. [Crossref] [PubMed]
- Egger M, Smith GD, Phillips AN. Meta-analysis: principles and procedures. BMJ 1997;315:1533-7. [Crossref] [PubMed]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine 2002;21:1539. [Crossref] [PubMed]
- Hashem MD, Parker AM, Needham DM. Early mobilization and rehabilitation of patients who are critically Ill. Chest 2016;150:722-31.
- Wieczorek B, Burke C, Al-Harbi A, et al. Early mobilization in the pediatric intensive care unit: a systematic review. J Pediatr Intensive Care 2015;2015:129-70.
- Engel HJ, Needham DM, Morris PE, et al. ICU early mobilization: from recommendation to implementation at three medical centers. Crit Care Med 2013;41:S69. [Crossref] [PubMed]
- Zhang Z, Xu X, Ni H. Small studies may overestimate the effect sizes in critical care meta-analyses: a meta-epidemiological study. Crit Care 2013;17:R2. [Crossref] [PubMed]
Cite this article as: Zhang G, Zhang K, Cui W, Hong Y, Zhang Z. The effect of early mobilization for critical ill patients requiring mechanical ventilation: a systematic review and meta-analysis. J Emerg Crit Care Med 2018;2:9.