
Sedation of the trauma patient in the intensive care unit
Introduction
Sedation in the intensive care patient is a fine art; gone are the days of perfectly paralysed, quietly ventilated patients neatly tucked into starched white sheets. What was once essentially an extended general anaesthetic often infusing etomidate and benzodiazepines; has become a richer, and more complicated, aspect of ICU care.
Advances in ventilator technology and efforts to reduce length of stay, iatrogenic ill effects, delirium and extended rehabilitation have led to a more considered approach.
The trauma patient is a greater challenge—they often have multi system dysfunction, significant analgesic requirements and a likelihood of repeated surgeries; they constitute a significant proportion of the critically ill. Intensive care units (ICUs) in the United Kingdom admitted 11,953 major trauma patients in 2015 (1); in the United States the National Trauma Databank 2015 report described 184,851 patients with an injury severity score greater than 16 (2).
Why sedate trauma patients?
The trauma patient often requires initially deep sedation to alleviate pain, anxiety and agitation and to allow initial management of their condition; sedation facilitates treatment that would otherwise be painful or distressing including traction, splinting or dressing change. Targeted sedation may be used as a treatment modality in itself, for example in the head injured patient requiring management of intracranial pressure.
Common sedatives
The ideal sedative agent would combine sedation, analgesia and anxiolysis, it would have a fast onset and not accumulate in organ dysfunction, have minimal cardiorespiratory depressant effects, minimal interactions with other drugs and ideally cost little.
A plethora of studies have failed to find the superior sedative agent (3), indeed the specific requirements of the trauma patient tend to require a more balanced polypharmaceutical approach to achieve an adequately sedated, analogized patient who can be nursed safely.
Propofol
Propofol is an intravenous, alkylphenol derivative, which facilitates inhibitory neurotransmission mediated by gamma-aminobutyric acid (GABA) acting on the GABAA receptor. It is sedative, hypnotic, anxiolytic, anti-emetic and produces anterograde amnesia (4).
Propofol has gained favour as an intensive care sedative due to its rapid onset and offset, and dose dependent level of sedation (5); it has a high degree of lipid solubility with a half-life of 2–3 minutes. It has been used in the ICU since the 1980’s and as such physicians are very comfortable in its use (6).
Propofol suppresses cellular oxygen consumption and carbon dioxide production without increasing anaerobic metabolism and thus preserves cerebral autoregulation. It reduces intracranial pressure and at high doses can suppress the EEG (5).
However propofol does cause peripheral vasodilatation and has negative inotropic and chronotropic effects which can cause a drop in cerebral perfusion pressure. Its high calorie load can impair oxidation of fatty acid chains and inhibit mitochondrial oxidative phosphorylation—the propofol infusion syndrome or PRISS (7).
PRISS is associated with high doses (>4 mg/kg per hour or >67 µg/kg per minute) and long-term (>48 hours) use of propofol (8,9). The presenting features of PRIS are cardiac dysfunction (88%), severe metabolic acidosis (86%) rhabdomyolysis (cardiac and skeletal muscle) (45%), renal failure (37%), and hypertriglyceridaemia (15%). Other significant features include hepatomegaly, hyperkalemia, and lipaemia (10). PRIS carries a high mortality (11). Not only is PRISS is more common in trauma patients (12) and head injured patients (13,14) but may be more difficult to diagnose in patients who may have acidosis, rhabdomyolysis and raised CK secondary to their initial injury.
Opioids
There are a number of opioids used in the ICU, each affecting the various subsets of opiate receptors µ1, µ2, κε and δ to differing degrees (15). The trauma patient requires significant amounts of opioid, often infused as part of a co-sedation strategy over what may be a lengthy ICU stay. It is common to see cardiovascular depression, respiratory depression, dysphoria, hallucinations, nausea and constipation. Indeed in some cases activation of the δ receptor can cause seizures (16).
When considering which opioid to use, awareness of each drug’s pharmacokinetics and pharmacodynamics is vital (Table 1). For example, prolonged use of morphine can lead to tachyphylaxis, accumulation and unpredictable waking; this is exacerbated in renal failure due to the active metabolites (17). The more lipid soluble opioids such as fentanyl, alfentanil, and sufentanil, are shorter acting but can still accumulate over lengthy infusions.
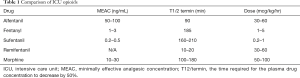
Full table
Remifentanil differs from other opioids in that it is rapidly metabolized by plasma esterases and has the shortest half-life of 3 minutes; the lack of accumulation confers an added advantage in rapid assessment of the patient’s neurology on desedating (18-20). In comparison, a modelled context-sensitive half-time for a 3-h infusion of alfentanil is 50–55 min (21).
Benzodiazepines
Benzodiazepines act at GABAA receptors, causing an influx of chloride ions that result in central nervous system depression. The effect on the patient is anxiolysis, anticonvulsant and amnesic. Cerebral blood flow is reduced, as is intracranial pressure. Critical care units in the United Kingdom preferentially use midazolam due to its shorter half-life whereas lorazepam is more common in the United States (22).
Benzodiazepines are highly lipid soluble, metabolized in the liver and excreted renally. The main disadvantage of their use is accumulation, delirium and withdrawal reactions (22,23). A recent study found lorazepam was an independent risk factor for delirium in ICU patients (OR, 1.2; 95% CI, 1.2–1.4), while fentanyl, morphine, and propofol were not (24). Like many of the sedative agents used in the ICU, benzodiazepines are immunosuppressant (25).
Ketamine
Ketamine is a phencyclidine derivative that acts as a non-competitive NMDA receptor antagonist. It is highly lipid soluble and undergoes rapid breakdown and redistribution to peripheral tissues. It is metabolized extensively in the liver and produces an active metabolite that can accumulate (26).
Ketamine is a novel agent in that it produces a dissociate state and dose dependent anaesthesia, with amnesia, in the absence of cardiorespiratory depression (27). It also has anti-inflammatory properties (28). Ketamine can be beneficial in the lung injured or bronchospastic patient as it relaxes bronchial smooth muscle (29).
It was previously thought that the sympathetic stimulation produced by ketamine could cause an increase in intracranial pressure and as such should not be given to head injured patients. However recent studies suggest this may not be the case for mechanically ventilated patients (30,31). Careful consideration should be given to using this drug in traumatic brain injury, and intracranial pressure should be closely monitored.
There is certainly a role for ketamine sedation, both as an analgosedating drug (32), and in the difficult to sedate patient (33). There are ongoing studies into the exploitation of the action of ketamine on the NMDA receptor to treat depression and post-traumatic stress disorder- a common occurrence in trauma patients (34).
Barbiturates
Modern day sedation practice limits the infusion of barbiturates to management of refractory status epilepticus and reduction of intracranial hypertension (35). Thiopentone rapidly reduces cerebral blood flow and oxygen utilisation and at higher doses of greater than 40 mg/L cause burst suppression on the electroencephalogram (36); such doses may have a negative cardiovascular impact. The zero order pharmacokinetics at plasma levels greater than 30 mg/L can lead to saturation of enzyme pathways and accumulation. Thiopentone exhibits a dose dependent inhibition of neutrophil activity (37) and can cause dyskalemia in infusion (38).
Alpha two agonists
The α-2 adrenergic receptor agonists inhibit adenylyl cyclase, reducing cyclic adenosine monophosphate and causing hyperpolarization of noradrenergic neurons in the locus ceruleus (39). The net effect is prevention of calcium ions entering the nerve terminal, suppressing release of noradrenaline (Figure 1).
There are two main alpha 2 agonists used in ICU, clonidine and dexmedetomidine. Dexmedetomidine is more selective for the alpha 2 receptor; 1,620:1 versus 200:1 and as such displays greater efficacy and a reduced incidence of dose dependent side effects such as bradycardia and hypotension (41,42). Further discussion will concentrate on dexmedetomidine alone (43).
Dexmedetomidine has a half-life of 6 minutes, is hepatically metabolized and does not accumulate (40). Within thirty minutes of commencing an infusion the patient is seen to be in a state of ‘conscious’ sedation, whereby they are calm and co-operative but easily roused; no respiratory depression and display relatively well preserved psychomotor function (44). Dexmedetomidine can be effective in improving tolerance to non-invasive ventilation (45).
In the PRODEX and MIDEX studies (46) dexmedetomidine in infusion demonstrated a significantly reduced time to extubation compared to midazolam, and a non-statistically significant reduction in comparison to propofol. Median length of stay in ICU was shorter for dexmedetomidine against both midazolam and propofol, but differences were not statistically significant. Those in the dexmedetomidine arm required less morphine and were found to have a lower incidence of agitation in comparison to those in the propofol and midazolam arms (46,47).
Dexmedetomidine significantly attenuated surgical stress and neuroendocrine response (IL-6, cortisol) in comparison with morphine and reduced the incidence and duration of delirium after cardiac surgery (48). The trauma patient suffers a profound stress response, and the ability to attenuate the reaction may improve the clinical course.
The main disadvantage to the use of an alpha two agonists is the cardiodepressant effects of bradycardia and hypotension, which can limit the demographic this drug may be used in. It should be avoided in those with bradyarrhythmias, in the initial stages of resuscitation and is contraindicated in those with a history of malignant hyperpyrexia (Table 2) (49).
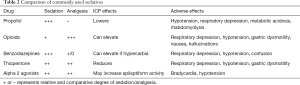
Full table
Monitoring sedation in the trauma patient
Severely injured trauma patients often undergo lengthy intensive care stays with multiple interventions. As such it is of the utmost importance to regularly asses the need for, depth and effectiveness of the sedation strategy.
Over-sedation can lengthen artificial ventilation time, which increase the risk of pneumonia and lung injury, the requirement for tracheostomy and delayed weaning. There is an increased risk of cardiovascular depression, ileus, and delirium. Prolonged immobility will increase the risk of thrombosis, critical illness myopathy and lengthen rehabilitation. When we consider the immunosupression effects of many commonly used sedative agents, it is clear oversedation can be highly detrimental to these patients (50).
Under-sedation can increase sympathetic activation, increase oxygen utilisation, cause anxiety, pain and hypercoagulability. The agitated, under sedated patient may cause harm to themselves by dislodging endotracheal tubes, access and monitoring lines; they pose a significant nursing challenge.
Haemodynamic responses as a measure of sedation are unreliable in the critically ill patient, hence the need for formal sedation scoring and assessment for delirium (51).
The most commonly used sedation scares are the Riker Sedation-Agitation Scale (52) and the Richmond Agitation-Sedation Scale (53). Comparison of the two has not found one to be a superior measure (54).
The Riker score ranges from 1 to 7, with a score of less than 4 indicating deeper sedation, 4 being a cooperative patient. The Richmond Agitation scale ranges from −5 to +4 with 0 considered a calm cooperative patient. Sedation scores should be monitored regularly; patients who spend more time at their target sedation level have a better outcome (55).
When considering a sedation strategy, aim for or prescribe a particular score on whichever system the unit uses. This improves communication between the multidisciplinary teams and also indicates the progress of weaning from sedation. In conjunction with sedation monitoring, a daily assessment for delirium should be made.
Pain, agitation and delirium in the trauma patient
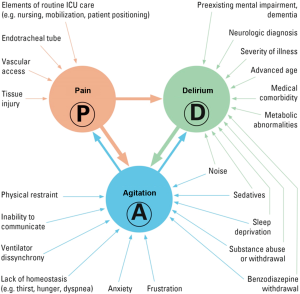
When considering the trauma patient in the ICU, the myriad of influences on their physical and mental condition can be overwhelming. Consideration of all factors, and the relationship between them, is necessary to improve the standard of care and patient outcome (Figure 2).
Pain
The trauma patient can be any age, any race, any gender but almost universally will be in pain; this may be from their initial injury or medical or surgical interventions to treat their trauma. This is in addition to the often painful procedures these patients undergo in the ICU—including endotracheal intubation, vascular access and the discomfort of being immobile.
Adequate analgesia is humane and the right of the patient; it obtunds the surgical stress response and promotes healing. Early healing allows reduced length of stay, early rehabilitation and a lower incidence of chronic pain (57-61). More than 60% of patients suffering major trauma report at least moderately severe pain at 1-year postinjury (61).
Poorly treated pain increases myocardial oxygen demand and can cause cardiac arrhythmias and myocardial ischaemia, pain induced hypoventilation causes atelectasis and reduces functional residual capacity. Pain increases the risk of agitation, delirium and the development of post-traumatic stress disorder and has a negative immunomodulatory effect (62-64).
Effective pain management will consist of regular simple analgesia and an opioid in conjunction with a sedative agent that has analgesic properties, such as propofol an alpha two agonist. If appropriate, regional anaesthetic techniques such as epidural infusions, nerve blocks or wound catheters can highly effective at reducing overall analgesia requirements.
Assessment of pain in the deeply sedated patient can be difficult, there are tools available such as the Behavioural Pain Scale (65) and the Critical Care Pain Observation Tool (66) allow repeatable, reliable assessment.
Agitation
Agitation is a psychomotor disturbance characterized by a marked increase in motor and psychological activity in a patient (67), it often occurs in conjunction with pain and delirium and is extremely common in intensive care patients, up to 71 percent suffer an agitated state at some time during their ICU stay (67,68).
Agitation is dangerous for the trauma patient; it causes an increased oxygen consumption, may remove or disconnect lines, have difficulty synchronizing with the ventilator and may even self extubate (69-75). Longer term, there are associations between agitation and the development of post-traumatic stress disorder (76-82).
Agitation in the trauma patient has more contributive factors; increased immobility from splints, traction, or casts; heightened anxiety due to recent trauma, cognitive or memory deficits and an inability to communicate these issues if they are sedated and intubated.
The nature of the trauma will have a significant bearing on agitation if, for example, there were multiple causalities, injuries or death to family or friends of the patient, and of course, if, when and how his is communicated to the patient.
Ventilator dyssynchrony may be a significant source of agitation. A study by Thille et al. (83) found that 24% of patients experienced asynchrony in at least 10% of their breaths and that this mismatch of respiratory cycling and flow of ventilation resulted in a longer duration of mechanical ventilation.
Patient factors to consider include the output of the respiratory centre which requires input from the cerebral cortex; this may not be functioning normally in the trauma patient; the autonomic pneumotaxic and apneustic centres in the brain stem and the respiratory groups in the medulla (84). Efferents are sent via the phrenic and intercostal nerves which again may not be fully functional in the trauma patient.
The degree of sedation a patient is receiving may reduce effective ventilator triggering and cause dyssynchrony (72). Conversely an under-sedated patient in pain or with increased metabolic rate may increase respiratory drive such that the ventilator will double trigger (85); or reduce their inspiratory effort (86). Post trauma ileus and abdominal distension may also cause diaphragmatic splinting and adversely affect ventilation and synchronisation. Decreased muscular strength—for example in the spinal injury patients, may also cause dyssynchrony due to diaphragmatic deconditioning, or indeed if the diaphragm is injured. Anxiety can also induce synchrony due to tachypnoea.
Sleep deprivation
Sleep deprivation almost invariably occurs in intensive care patients (87,88) and causes changes in memory, cognition, vascular tone, blood pressure and immunity, increasing the physiological stress placed on the patient (89). Analysis of electroencephalogram data of intensive care patients demonstrates a sleep pattern that is fragmented with prolonged latencies, frequent waking, predominance of stage 1 and 2 sleep and decreased or absent stage 3, 4 and rapid eye movement or REM sleep (90-93). Day/night cycling is altered, with half of sleep occurring in the day (94). Studies have found that the sleep deprived undergo reduced cerebral oxygenation, reduced response to hypoxia and hypercapnia (95,96), followed by increased ventilatory motor function and ventilator dyssynchrony (97). An increase in cytokines and decrease in melatonin secretion as seen in the trauma stress response will alter the sleep wake cycle (92,93).
Noise and environment
The World Health Organization recommends that the average background noise in hospitals should not exceed 30 A-weighted decibels [dB(A)], and that peaks during the night time should be <40 dB(A) (98). Noise studies have found that nebulizers are as loud as 80 dB(A), and continuous positive airway pressure hoods have sound pressure levels of above 100 dB(A) (99). In terms of patient care, prolongation of the time taken to fall asleep can be seen at maximum noise levels of 45 dB(A) (100,101). Major sources of noise identified ventilators, suctioning, alarms, telephones, televisions and radios, trolleys and bin noises, staff bleeps and talking (102).
Perceived lack of control over ambient noise also acts as a stressor (103,104) although there is great variability in noise sensitivity amongst individuals.
Ambient light on the ICU does not follow natural circadian rhythms, patients are exposed to constant light interruptions through the night (105). This can have deleterious effects on immune function (106), cognitive function (107) and is linked to the development of delirium (108).
Withdrawal
Withdrawal from addictive substances is common in the ICU; the causative agents are commonly alcohol, nicotine and illicit drugs. Withdrawal may also be iatrogenic, either by withholding previously prescribed medications or introducing and then reducing new agents; particularly benzodiazepines. Withdrawal greatly increase agitation, and may not be readily apparent in the heavily sedated trauma patient (109).
Looking at the potential for withdrawal in the trauma patient, nearly 50% have a positive blood alcohol concentration upon admission (110,111). A study of 225,081 patients from the National Trauma Database found alcohol was present in 40, 714 or 18.1% of cases, drugs in 58, 353 (25.9%) and a combination of drugs and alcohol in 51, 702 or 23%. Drug or alcohol use was significantly more common in males n=162,227, 72% (112).
Sedation strategies in those known, or suspected to be suffering withdrawal should include tapering doses of benzodiazepines, consideration of supplementation, for example a nicotine patch; and attention to nutrition and potential vitamin deficiencies. Alpha two agonists can be effective in reducing requisite benzodiazepines and assist in managing withdrawal (113).
Delirium
The rapid onset of fluctuating disturbance of consciousness and cognition that delineates delirium is common in the ICU; up to 80% of patients are thought to develop some aspect of delirium during their stay (114). Two recent studies found 36% (115) and 38.8% (116) of ICU trauma patients to be delirious. As diagram 2 shows, the many multifactorial elements that combine to induce delirium are not all amenable to treatment, but may allow us to predict which of our patients are more likely to become delirious. If one considers the trauma patient they are at higher risk of developing delirium due to multiple painful injuries necessitating high doses of opioids and sedation, increased likelihood of neurological involvement and often a protracted stay.
Early recognition and management is paramount; delirious patients are three times more likely to die than similar non-delirious patients (117-119); they spend more time mechanically ventilated and have a greater risk of re-intubation (120). Those that survive have a greater risk of long term cognitive dysfunction and require more long term care (102). Risk factors for the development of delirium are increasing age, use of sedation, neurological impairment and increased severity of illness (121).
Assessment of delirium
There are two commonly used tools to asses delirium in intensive care patients, the Confusion Assessment Method for the ICU (CAM-ICU) (121) and the Intensive Care Delirium Screening Checklist (ICDSC) (122).
CAM-ICU is designed to be used in lightly sedated patients—those with a The Richmond Agitation-Sedation Scale score of −3 to +4. The aim is to assess the content of patient consciousness, to identify fluctuating levels of consciousness, the presence of inattention and disorganized thinking. This is a snapshot assessment that may be repeated, and should be undertaken at least daily. A CAM-ICU positive patient is delirious.
The ICDSC scores level of consciousness, inattention, disorientation, sleep disturbance, hallucinations and psychomotor retardation over the period of a nursing shift.
It should be remembered that there are two types of delirium; hypoactive and hyperactive, and a patient may suffer one, or both-a mixed delirium.
The hypoactive delirious patient suffers inattention, disorganized thinking and a decreased level of consciousness in the absence of agitation. It is easy to miss a diagnosis of hypoactive delirium as the patient is calm, quiet and easily overlooked; it is this group that has the delirium related greatest mortality (111).
Measures to reduce the onset of delirium include noise reduction, cognitive stimulation and reorientation and early mobilisation (122). There is some evidence to suggest sedation with dexmedetomidine can reduce the incidence of delirium (45,123).
Sedation in the brain injured patient
The aim of the sedation strategy in brain injured patients is not only to manage pain, agitation, reduce delirium and improve ventilator synchrony but also to reduce cerebral metabolic demand, attenuate intracranial pressure and blunt central hyperventilation; some patients may also require control of refractory seizures. Brain injured patients have impaired auto-regulation of cerebral blood flow (124); many sedative agents, with the exception of ketamine, compound this with a dose dependent decrease in flow (125,126).
The cumulative effect is a predisposition to lowered cerebral perfusion pressure and hence secondary neuronal injury (127). This secondary injury is associated with a slow velocity depolarisation wave across the grey matter (128-130), failure of ion homeostasis, efflux of excitatory amino acids and an increase in cell metabolism, requiring increased blood flow that may not be available in the injured brain (131,132). There is current interest in the use of ketamine to reduce the incidence of spreading depolarisations (133-135).
Anti-epileptic agents are often used in conjunction with sedatives, indeed in this situation propofol in combination with benzodiazepines can be very effective. Propofol is now considered a treatment for status epilepticus (136-139).
Barbiturates are effective to cause burst suppression but are not indicated as a maintenance sedative or as a prophylaxis against raise intracranial pressure (140).
Sedation and clinical observation
The trauma patient requires close monitoring of their injuries to diagnose any deterioration in their condition; this is of particular importance in abdominal trauma or those at risk of compartment syndrome. In patients requiring heavy sedation such assessment is not possible. In those receiving light, multi-modal sedation which includes opioids pain assessment can be more challenging. It is important to establish a clear baseline of patient pain and physiological parameters and maintain a consistent approach regarding choice of agents. Reassessment should be frequent and in conjunction with other observations including motor and sensory function, examination of body systems and if there are concerns, early imaging and specialist review. Any abrupt alteration in sedation requirements should prompt a search for the cause (141).
Similarly, hypotension from a developing injury may be erroneously attributed to sedation. Once the trauma patient has settled on a sedative regime, it is vital to monitor for aberrant physiology and again thoroughly reassess for occult bleeding, signs or symptoms of sepsis or anaphylaxis to new agents. Arterial blood gases, urine output, laboratory bloods, imaging and expert review will aid in determining the cause of any deterioration.
Sedation holds and weaning
In the acute phase of trauma, sedation holds may not be appropriate; particularly in patients with brain injury and raised intracranial pressure.
Sedation holds allow assessment of the underlying neurological condition of the patient and are associated with reduced time to extubation, length of stay (142) and in one study a statistically non-significant reduction in mortality (143). In a cohort of ICU patients, the duration of delirium was halved with a programme of sedation breaks and early mobilisation (144).
Sedation holds also allow assessment of minimal tolerable levels of sedation. A study by Shehabi et al. (145) found that depth of sedation was independently associated with the duration of ventilation, in-hospital mortality, and rates of death within 180 days. In terms of longer term effects, studies examining psychiatric outcomes such as quality of life, depression, anxiety, and post-traumatic stress disorder found either an improvement or no change (146-148).
Adjuncts to sedation
A firm grasp of the interplay between the causes of pain, agitation and delirium and subsequent sedation requirements allows the use of appropriate adjuncts such as noise reduction strategies. The nightly use of earplugs reduced the incidence of confusion in a study of 69 ICU patients, an effective, cost effective and minimally invasive solution (149).
Melatonin supplementation is often used to restore a sleep-wake balance, as yet there is there is no conclusive high grade evidence that melatonin is beneficial in sleep deprivation (150-152), although some studies are suggesting a benefit (153); a trial is currently recruiting to examine the role of melatonin in preventing delirium (154).
Antipsychotics such as haloperidol or the atypical antipsychotics—quetiapine, risperidone, may be beneficial in reducing the incidence of delirium and aid sedation and can often be beneficial in trauma patients who have a higher incidence of post-traumatic stress disorder (155-157).
Conclusions
Devising a sedation strategy for the trauma patient can be challenging. A full assessment of the patient and their comorbidities, the nature of the trauma and assessment of potential withdrawal is vital. The mainstay of management is adequate analgesia incorporating regular simple analgesia, adjuncts such as regional anaesthesia techniques where appropriate, and regular, often infusions of, opioid.
A fast acting agent with analgesic and amnesic properties allows rapid targeting to the desired sedation level, and in many cases propofol or dexmedetomidine can prove the preferred agent.
The brain injured patient requires close attention to cerebral blood flow and intracranial pressure management and it is this group in particular that benefits from the use of rapid acting agents such as remifentanil.
Reducing stimulation and the preventing development of delirium using noise reduction strategies, earplugs, regular orientation and early mobilisation will reduce overall sedation requirements, length of stay and overall mortality.
Many hospitals now employ care bundles to unify the approach to sedation, namely the ‘pain, agitation, and delirium’ (PAD) guidelines (158) and the spontaneous awakening and breathing coordination, attention to the choice of sedation, delirium monitoring, and early mobility and exercise (ABCDE) bundle (159). This multidisciplinary approach enables us to get ever closer to our goal—calm, cooperative, comfortable patients who make a smooth and swift journey through the ICU to ward level care or rehabilitation with minimal long term psychological disturbance.
Acknowledgements
I would like to thank Dr. Jim Gregory, MD for his contribution to this article.
Footnote
Conflicts of Interest: Dr. Joseph lectures for and has received honoraria from Orion Pharmaceuticals.
References
- National Trauma Database. Available online: https://www.facs.org/~/media/files/quality%20programs/trauma/ntdb/ntdb%20annual%20report%202015.ashx
- ICNARC. Management of patients. Available online: https://www.icnarc.org/Our-Audit/Audits/Cmp/Our-National-Analyses/Management-Of-Patients
- Roberts DJ, Haroon B, Hall RI. Sedation for critically ill or injured adults in the intensive care unit: a shifting paradigm. Drugs 2012;72:1881-916.[Crossref][PubMed]
- Hales TG, Lambert JJ. The actions of propofol on inhibitory amino acid receptors of bovine adrenomedullary chromaffin cells and rodent central neurones. Br J Pharmacol 1991;104:619-28.[Crossref][PubMed]
- Barr J. Propofol: a new drug for sedation in the intensive care unit. Int Anesthesiol Clin 1995;33:131-54.[Crossref][PubMed]
- Grounds RM, Lalor JM, Lumley J, et al. Propofol infusion for sedation in the intensive care unit: preliminary report. Br Med J (Clin Res Ed) 1987;294:397-400.[Crossref][PubMed]
- Wolf A, Weir P, Segar P, et al. Impaired fatty acid oxidation in propofol infusion syndrome. Lancet 2001;357:606-7.[Crossref][PubMed]
- McKeage K, Perry CM. Propofol: a review of its use in intensive care sedation of adults. CNS Drugs 2003;17:235-72.[Crossref][PubMed]
- Iyer VN, Hoel R, Rabinstein AA. Propofol infusion syndrome in patients with refractory status epilepticus: an 11-year clinical experience. Crit Care Med 2009;37:3024-30.[Crossref][PubMed]
- Roberts RJ, Barletta JF, Fong JJ, et al. Incidence of propofol-related infusion syndrome in critically ill adults: a prospective, multicenter study. Crit Care 2009;13:R169.[Crossref][PubMed]
- Vasile B, Rasulo F, Candiani A, et al. The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med 2003;29:1417-25.[Crossref][PubMed]
- Cremer OL, Moons KG, Bouman EA, et al. Long-term propofol infusion and cardiac failure in adult head-injured patients. Lancet 2001;357:117-8.[Crossref][PubMed]
- Otterspoor LC, Kalkman CJ, Cremer OL. Update on the propofol infusion syndrome in ICU management of patients with head injury. Curr Opin Anaesthesiol 2008;21:544-51.[Crossref][PubMed]
- Urwin SC, Menon DK. Comparative tolerability of sedative agents in head-injured adults. Drug Saf 2004;27:107-33.[Crossref][PubMed]
- Jutkiewicz EM, Baladi MG, Folk JE, et al. The convulsive and electroencephalographic changes produced by nonpeptidic delta-opioid agonists in rats: comparison with pentylenetetrazol. J Pharmacol Exp Ther 2006;317:1337-48.[Crossref][PubMed]
- Osborne RJ, Joel SP, Slevin ML. Morphine intoxication in renal failure: the role of morphine-6-glucuronide. Br Med J (Clin Res Ed) 1986;292:1548-9.[Crossref][PubMed]
- Michelsen LG, Hug CC Jr. The pharmacokinetics of remifentanil. J Clin Anesth 1996;8:679-82.[Crossref][PubMed]
- Egan TD, Lemmens HJ, Fiset P, et al. The pharmacokinetics of the new short-acting opioid remifentanil (GI87084B) in healthy adult male volunteers. Anesthesiology 1993;79:881-92.[Crossref][PubMed]
- Karabinis A, Mandragos K, Stergiopoulos S, et al. Safety and efficacy of analgesia-based sedation with remifentanil versus standard hypnotic-based regimens in intensive care unit patients with brain injuries: a randomised, controlled trial Crit Care 2004;8:R268-80. [ISRCTN50308308].[Crossref][PubMed]
- Kapila A, Glass PS, Jacobs JR, et al. Measured context-sensitive half-times of remifentanil and alfentanil. Anesthesiology 1995;83:968-75.[Crossref][PubMed]
- Spina SP, Ensom MH. Clinical pharmacokinetic monitoring of midazolam in critically ill patients. Pharmacotherapy 2007;27:389-98.[Crossref][PubMed]
- Swart EL, Zuideveld KP, de Jongh J, et al. Comparative population pharmacokinetics of lorazepam and midazolam during long-term continuous infusion in critically ill patients. Br J Clin Pharmacol 2004;57:135-45.[Crossref][PubMed]
- Pandharipande P, Shintani A, Peterson J, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology 2006;104:21-6.[Crossref][PubMed]
- Frendl G. Benzodiazepines: revealing of the secrets of GABAA-mediated immunosuppression: GABAA subtype-specific benzodiazepines are the hope. Crit Care Med 2013;41:1807-8.[Crossref][PubMed]
- Revers JG, Glass PS, Lubarsky DA, et al. Intravenous Anesthetics. In: Miller RD, editor. Miller’s Anesthesia. 7th edition. Philadelphia, USA: Churchill Livingstone, 2010;1:719-68.
- Goyal S, Agrawal A. Ketamine in status asthmaticus: A review. Indian J Crit Care Med 2013;17:154-61.[Crossref][PubMed]
- Yoon SH. Concerns of the anesthesiologist: anesthetic induction in severe sepsis or septic shock patients. Korean J Anesthesiol 2012;63:3-10.[Crossref][PubMed]
- White PF, Elig MR. Intravenous anaesthetics. In: Barash PG, editor. Clinical Anaesthesia. 6th edition. China: Lippincott Williams and Wilkins, 2013:478-500.
- Himmelseher S, Durieux ME. Revising a dogma: ketamine for patients with neurological injury? Anesth Analg 2005;101:524-34. table of contents.[Crossref][PubMed]
- Bar-Joseph G, Guilburd Y, Tamir A, et al. Effectiveness of ketamine in decreasing intracranial pressure in children with intracranial hypertension. J Neurosurg Pediatr 2009;4:40-6.[Crossref][PubMed]
- Patanwala AE, Martin JR, Erstad BL. Ketamine for Analgosedation in the Intensive Care Unit: A Systematic Review. J Intensive Care Med 2017;32:387-95.[Crossref][PubMed]
- Benken ST, Goncharenko A. The Future of Intensive Care Unit Sedation: A Report of Continuous Infusion Ketamine as an Alternative Sedative Agent. J Pharm Pract 2017;30:576-81.[Crossref][PubMed]
- Feder A, Parides MK, Murrough JW, et al. Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry 2014;71:681-8.[Crossref][PubMed]
- Mirski MA, Hemstreet MK. Critical care sedation for neuroscience patients. J Neurol Sci 2007;261:16-34.[Crossref][PubMed]
- Evers A, Crowder C. General anesthetics. In: Hardman JG, Limbird LE, Gilman AG, editors. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. 10th edition. New York: McGraw-Hill, 2001:337-65.
- Nishina K, Akamatsu H, Mikawa K, et al. The inhibitory effects of thiopental, midazolam, and ketamine on human neutrophil functions. Anesth Analg 1998;86:159-65.[PubMed]
- Ng SY, Chin KJ, Kwek TK. Dyskalaemia associated with thiopentone barbiturate coma for refractory intracranial hypertension: a case series. Intensive Care Med 2011;37:1285-9.[Crossref][PubMed]
- Pichot C, Ghignone M, Quintin L. Dexmedetomidine and clonidine: from second- to first-line sedative agents in the critical care setting? J Intensive Care Med 2012;27:219-37.[Crossref][PubMed]
- Dexdor—Summary of Product Characteristics. Available online: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR__Product_Information/human/002268/WC500115631.pdf
- Masuki S, Dinenno FA, Joyner MJ, et al. Selective alpha2-adrenergic properties of dexmedetomidine over clonidine in the human forearm. J Appl Physiol 1985;2005:587-92.[PubMed]
- Srivastava U, Sarkar ME, Kumar A, et al. Comparison of clonidine and dexmedetomidine for short-term sedation of intensive care unit patients. Indian J Crit Care Med 2014;18:431-6.[Crossref][PubMed]
- Zhang Z, Chen K, Ni H, et al. Sedation of mechanically ventilated adults in intensive care unit: a network meta-analysis. Sci Rep 2017;7:44979.[Crossref][PubMed]
- Hall JE, Uhrich TD, Barney JA, et al. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg 2000;90:699-705.[Crossref][PubMed]
- Demuro JP, Mongelli MN, Hanna AF. Use of dexmedetomidine to facilitate non-invasive ventilation. Int J Crit Illn Inj Sci 2013;3:274-5.[Crossref][PubMed]
- Jakob SM, Ruokonen E, Grounds RM, et al. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA 2012;307:1151-60.[Crossref][PubMed]
- Riker RR, Shehabi Y, Bokesch PM, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA 2009;301:489-99.[Crossref][PubMed]
- Al-Medani SM, Neemat-Allah FA, El-Sawy MM, et al. Effects of dexmedetomidine versus morphine on surgical stress response and analgesia in postoperative open cardiac surgery. Res Opin Anesth Intensive Care 2015;2:16-23.
- Keating GM. Dexmedetomidine: A Review of Its Use for Sedation in the Intensive Care Setting. Drugs 2015;75:1119-30.[Crossref][PubMed]
- Hughes CG, McGrane S, Pandharipande PP. Sedation in the intensive care setting. Clin Pharmacol 2012;4:53-63.[PubMed]
- Oddo M, Crippa IA, Mehta S, et al. Optimizing sedation in patients with acute brain injury. Crit Care 2016;20:128.[Crossref][PubMed]
- Riker RR, Picard JT, Fraser GL. Prospective evaluation of the Sedation-Agitation Scale for adult critically ill patients. Crit Care Med 1999;27:1325-9.[Crossref][PubMed]
- Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 2002;166:1338-44.[Crossref][PubMed]
- Pun BT, Dunn J. The sedation of critically ill adults: Part 1: Assessment. The first in a two-part series focuses on assessing sedated patients in the ICU. Am J Nurs 2007;107:40-8.[PubMed]
- De Jonghe B, Bastuji-Garin S, Fangio P, et al. Sedation algorithm in critically ill patients without acute brain injury. Crit Care Med 2005;33:120-7.[Crossref][PubMed]
- Reade MC, Finfer S. Sedation and delirium in the intensive care unit. N Engl J Med 2014;370:444-54.[Crossref][PubMed]
- Hedderich R, Ness TJ. Analgesia for trauma and burns. Crit Care Clin 1999;15:167-84.[Crossref][PubMed]
- Aisuodionoe-Shadrach OI, Olapade-Olaopa EO, Soyannwo OA. Preoperative analgesia in emergency surgical care in Ibadan. Trop Doct 2006;36:35-6.[Crossref][PubMed]
- Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science 2000;288:1765-9.[Crossref][PubMed]
- Cohen SP, Christo PJ, Moroz L. Pain management in trauma patients. Am J Phys Med Rehabil 2004;83:142-61.[Crossref][PubMed]
- Malchow RJ, Black IH. The evolution of pain management in the critically ill trauma patient: Emerging concepts from the global war on terrorism. Crit Care Med 2008;36:S346-57.[Crossref][PubMed]
- Rivara FP, Mackenzie EJ, Jurkovich GJ, et al. Prevalence of pain in patients 1 year after major trauma. Arch Surg 2008;143:282-7; discussion 288.[Crossref][PubMed]
- Stein-Parbury J, McKinley S. Patients' experiences of being in an intensive care unit: a select literature review. Am J Crit Care 2000;9:20-7.[PubMed]
- Swinamer DL, Phang PT, Jones RL, et al. Effect of routine administration of analgesia on energy expenditure in critically ill patients. Chest 1988;93:4-10.[Crossref][PubMed]
- Payen JF, Bru O, Bosson JL, et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med 2001;29:2258-63.[Crossref][PubMed]
- Gélinas C, Fillion L, Puntillo KA, et al. Validation of the critical-care pain observation tool in adult patients. Am J Crit Care 2006;15:420-7.[PubMed]
- Chevrolet JC, Jolliet P. Clinical review: agitation and delirium in the critically ill--significance and management. Crit Care 2007;11:214.[Crossref][PubMed]
- Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002;30:119-41.[Crossref][PubMed]
- Fraser GL, Riker RR, Berthiaume DR, et al. A Prospective study of the incidence, severity, and therapeutics used for agitation in elderly versus younger critically ill patients. Chest 1998;26:101A.
- Fraser GL, Prato BS, Riker RR, et al. Frequency, severity, and treatment of agitation in young versus elderly patients in the ICU. Pharmacotherapy 2000;20:75-82.[Crossref][PubMed]
- Chevron V, Ménard JF, Richard JC, et al. Unplanned extubation: risk factors of development and predictive criteria for reintubation. Crit Care Med 1998;26:1049-53.[Crossref][PubMed]
- Boulain T. Unplanned extubations in the adult intensive care unit: a prospective multicenter study. Association des Réanimateurs du Centre-Ouest. Am J Respir Crit Care Med 1998;157:1131-7.[Crossref][PubMed]
- Dick CR, Sassoon CS. Patient-ventilator interactions. Clin Chest Med 1996;17:423-38.[Crossref][PubMed]
- Epstein SK. Optimizing patient-ventilator synchrony. Semin Respir Crit Care Med 2001;22:137-52.[Crossref][PubMed]
- Kallet RH, Alonso JA, Luce JM, et al. Exacerbation of acute pulmonary edema during assisted mechanical ventilation using a low-tidal volume, lung-protective ventilator strategy. Chest 1999;116:1826-32.[Crossref][PubMed]
- Atkins PM, Mion LC, Mendelson W, et al. Characteristics and outcomes of patients who self-extubate from ventilatory support: a case-control study. Chest 1997;112:1317-23.[Crossref][PubMed]
- Schelling G, Stoll C, Haller M, et al. Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 1998;26:651-9.[Crossref][PubMed]
- Simini B. Patients' perceptions of intensive care. Lancet 1999;354:571-2.[Crossref][PubMed]
- Scragg P, Jones A, Fauvel N. Psychological problems following ICU treatment. Anaesthesia 2001;56:9-14.[Crossref][PubMed]
- Jones C, Griffiths RD, Humphris G, et al. Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med 2001;29:573-80.[Crossref][PubMed]
- Nelson BJ, Weinert CR, Bury CL, et al. Intensive care unit drug use and subsequent quality of life in acute lung injury patients. Crit Care Med 2000;28:3626-30.[Crossref][PubMed]
- Rotondi AJ, Chelluri L, Sirio C, et al. Patients' recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med 2002;30:746-52.[Crossref][PubMed]
- Thille AW, Rodriguez P, Cabello B, et al. Patient-ventilator asynchrony during mechanical ventilation: Prevalence and risk factors. Intensive Care Med 2006;32:1515-22.[Crossref][PubMed]
- Kacmarek RM. Neurologic control of ventilation. In: Kacmarek RM, Dimas S, Mack CW, editors. The Essentials of Respiratory Care. 4. St Louis, MO: Elsevier Mosby, 2005:113-24.
- Prinianakis G, Kondili E, Georgopoulos D. Patient-ventilator interaction: an overview. Respir Care Clin N Am 2005;11:201-24.[Crossref][PubMed]
- Nilsestuen JO, Hargett KD. Using ventilator graphics to identify patient-ventilator asynchrony. Respir Care 2005;50:202-34; discussion 232-4.[PubMed]
- Howard RS, Radcliffe J, Hirsch NP. General medical care on the neuromedical intensive care unit. J Neurol Neurosurg Psychiatry 2003;74 Suppl 3:iii10-5.[Crossref][PubMed]
- Cabello B, Parthasarathy S, Mancebo J. Mechanical ventilation: let us minimize sleep disturbances. Curr Opin Crit Care 2007;13:20-6.[Crossref][PubMed]
- Parthasarathy S, Tobin MJ. Effect of ventilator mode on sleep quality in critically ill patients. Am J Respir Crit Care Med 2002;166:1423-9.[Crossref][PubMed]
- Cooper AB, Thornley KS, Young GB, et al. Sleep in critically ill patients requiring mechanical ventilation. Chest 2000;117:809-18.[Crossref][PubMed]
- Friese RS, Diaz-Arrastia R, McBride D, et al. Quantity and quality of sleep in the surgical intensive care unit: are our patients sleeping? J Trauma 2007;63:1210-4.[Crossref][PubMed]
- Gabor JY, Cooper AB, Crombach SA, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med 2003;167:708-15.[Crossref][PubMed]
- Weinhouse GL, Schwab RJ. Sleep in the critically ill patient. Sleep 2006;29:707-16.[Crossref][PubMed]
- Cummings KJ, Swart M, Ainslie PN. Morning attenuation in cerebrovascular CO2 reactivity in healthy humans is associated with a lowered cerebral oxygenation and an augmented ventilatory response to CO2. J Appl Physiol 1985;2007:1891-8.[PubMed]
- Richards KC, Anderson WM, Chesson AL Jr, et al. Sleep-related breathing disorders in patients who are critically ill. J Cardiovasc Nurs 2002;17:42-55.[Crossref][PubMed]
- Chowdhuri S, Pierchala L, Aboubakr SE, et al. Long-term facilitation of genioglossus activity is present in normal humans during NREM sleep. Respir Physiol Neurobiol 2008;160:65-75.[Crossref][PubMed]
- Himmelfarb J, McMonagle E, Freedman S, et al. Oxidative stress is increased in critically ill patients with acute renal failure. J Am Soc Nephrol 2004;15:2449-56.[Crossref][PubMed]
- Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit Care 2013;17:R187.[Crossref][PubMed]
- Wenham T, Pittard A. Intensive care unit environment. Crit Care Pain 2009;9:178-83.
- Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev 2003;7:215-25.[Crossref][PubMed]
- MacKenzie DJ, Galbrun L. Noise levels and noise sources in acute care hospital wards. Build Serv Eng Res Technol 2007;28:117-31.[Crossref]
- Freedman NS, Gazendam J, Levan L, et al. Abnormal sleep/wake cycles and the effect of environmental noise on sleep disruption in the intensive care unit. Am J Respir Crit Care Med 2001;163:451-7.[Crossref][PubMed]
- Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001;286:2703-10.[Crossref][PubMed]
- Castro R, Angus DC, Rosengart MR. The effect of light on critical illness. Crit Care 2011;15:218.[Crossref][PubMed]
- Nelson RJ, Drazen DL. Melatonin mediates seasonal changes in immune function. Ann N Y Acad Sci 2000;917:404-15.[Crossref][PubMed]
- Kent ST, McClure LA, Crosson WL, et al. Effect of sunlight exposure on cognitive function among depressed and non-depressed participants: a REGARDS cross-sectional study. Environ Health 2009;8:34.[Crossref][PubMed]
- Van Rompaey B, Elseviers MM, Schuurmans MJ, et al. Risk factors for delirium in intensive care patients: a prospective cohort study. Crit Care 2009;13:R77.[Crossref][PubMed]
- Lucidarme O, Seguin A, Daubin C, et al. Nicotine withdrawal and agitation in ventilated critically ill patients. Crit Care 2010;14:R58.[Crossref][PubMed]
- Lukan JK, Reed DN Jr, Looney SW, et al. Risk factors for delirium tremens in trauma patients. J Trauma 2002;53:901-6.[Crossref][PubMed]
- Field CA, Claassen CA, O’Keefe G. Association of alcohol use and other high-risk behaviors among trauma patients. J Trauma 2001;50:13-9.[Crossref][PubMed]
- Cowperthwaite MC, Burnett MG. Treatment course and outcomes following drug and alcohol-related traumatic injuries. J Trauma Manag Outcomes 2011;5:3.[Crossref][PubMed]
- Rayner SG, Weinert CR, Peng H, et al. Dexmedetomidine as adjunct treatment for severe alcohol withdrawal in the ICU. Ann Intensive Care 2012;2:12.[Crossref][PubMed]
- Girard TD, Pandharipande PP, Ely EW. Delirium in the intensive care unit. Crit Care 2008;12 Suppl 3:S3.[Crossref][PubMed]
- Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 2004;291:1753-62.[Crossref][PubMed]
- Von Rueden KT, Wallizer B, Thurman P, et al. Delirium in Trauma Patients: Prevalence and Predictors. Crit Care Nurse 2017;37:40-8.[Crossref][PubMed]
- Duceppe MA, Elliott A, Para M, et al. Modifiable risk factors for delirium in critically ill trauma patients: a multicenter prospective study. Critical Care 2015;19:478.[Crossref]
- Lin SM, Liu CY, Wang CH, et al. The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med 2004;32:2254-9.[Crossref][PubMed]
- Ouimet S, Kavanagh BP, Gottfried SB, et al. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med 2007;33:66-73.[Crossref][PubMed]
- van den Boogaard M, Schoonhoven L, Evers AW, et al. Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med 2012;40:112-8.[Crossref][PubMed]
- Zhang Z, Pan L, Ni H. Impact of delirium on clinical outcome in critically ill patients: a meta-analysis. Gen Hosp Psychiatry 2013;35:105-11.[Crossref][PubMed]
- van den Boogaard M, Pickkers P, Slooter AJ, et al. Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for intensive care patients: observational multicentre study. BMJ 2012;344:e420.[Crossref][PubMed]
- Bergeron N, Dubois MJ, Dumont M, et al. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med 2001;27:859-64.[Crossref][PubMed]
- Vidán MT, Sánchez E, Alonso M, et al. An intervention integrated into daily clinical practice reduces the incidence of delirium during hospitalization in elderly patients. J Am Geriatr Soc 2009;57:2029-36.[Crossref][PubMed]
- Pandharipande PP, Pun BT, Herr DL, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA 2007;298:2644-53.[Crossref][PubMed]
- Oddo M, Steiner LA. Sedation and analgesia in the neurocritical care unit. In: Smith MM, Citerio GG, Kofke WA, editors. Oxford textbook of neurocritical care. Oxford: Oxford University Press, 2016.
- Adembri C, Venturi L, Pellegrini-Giampietro D. Neuroprotective effects of propofol in acute cerebral injury. CNS Drug Rev. 2007;13:333-51.[Crossref][PubMed]
- Stephan H, Sonntag H, Schenk HD, et al. Anaesthesist 1987;36:60-5. [Effect of Disoprivan (propofol) on the circulation and oxygen consumption of the brain and CO2 reactivity of brain vessels in the human].[PubMed]
- Paul BS, Paul G. Sedation in neurological intensive care unit. Ann Indian Acad Neurol 2013;16:194-202.[Crossref][PubMed]
- Leao AA. Spreading depression of activity in the cerebral cortex. J Neurophysiol 1947;10:409-14.[Crossref][PubMed]
- Strong AJ, Hartings JA, Dreier JP. Cortical spreading depression: an adverse but treatable factor in intensive care? Curr Opin Crit Care 2007;13:126-33.[Crossref][PubMed]
- Hartings JA, Bullock MR, Okonkwo DO, et al. Spreading depolarisations and outcome after traumatic brain injury: a prospective observational study. Lancet Neurol 2011;10:1058-64.[Crossref][PubMed]
- Hartings JA, Strong AJ, Fabricius M, et al. Spreading depolarizations and late secondary insults after traumatic brain injury. J Neurotrauma 2009;26:1857-66.[Crossref][PubMed]
- Lauritzen M, Dreier JP, Fabricius M, et al. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J Cereb Blood Flow Metab 2011;31:17-35.[Crossref][PubMed]
- Hertle DN, Dreier JP, Woitzik J, et al. Effect of analgesics and sedatives on the occurrence of spreading depolarizations accompanying acute brain injury. Brain 2012;135:2390-8.[Crossref][PubMed]
- Sakowitz OW, Kiening KL, Krajewski KL, et al. Preliminary evidence that ketamine inhibits spreading depolarizations in acute human brain injury. Stroke 2009;40:e519-22.[Crossref][PubMed]
- Carlson AP. Spreading Depolarization and Ketamine Suppression (SAKS). Available online: https://clinicaltrials.gov/ct2/show/NCT02501941
- van Gestel JP, Blussé van Oud-Alblas HJ, Malingré M, et al. Propofol and thiopental for refractory status epilepticus in children. Neurology 2005;65:591-2.[Crossref][PubMed]
- Parviainen I, Uusaro A, Kälviäinen R, et al. Propofol in the treatment of refractory status epilepticus. Intensive Care Med 2006;32:1075-9.[Crossref][PubMed]
- Meierkord H, Boon P, Engelsen B, et al. EFNS guideline on the management of status epilepticus in adults. Eur J Neurol 2010;17:348-55.[Crossref][PubMed]
- Holtkamp M. The anaesthetic and intensive care of status epilepticus. Curr Opin Neurol 2007;20:188-93.[Crossref][PubMed]
- Roberts I, Sydenham E. Barbiturates for acute traumatic brain injury. Cochrane Database Syst Rev 2012;12:CD000033.[PubMed]
- Alpen MA, Morse C. Managing the pain of traumatic injury. Crit Care Nurs Clin North Am 2001;13:243-57.[PubMed]
- Jackson DL, Proudfoot CW, Cann KF, et al. A systematic review of the impact of sedation practice in the ICU on resource use, costs and patient safety. Crit Care 2010;14:R59.[Crossref][PubMed]
- Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet 2008;371:126-34.[Crossref][PubMed]
- Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009;373:1874-82.[Crossref][PubMed]
- Shehabi Y, Chan L, Kadiman S, et al. Sedation depth and long-term mortality in mechanically ventilated critically ill adults: a prospective longitudinal multicentre cohort study. Intensive Care Med 2013;39:910-8.[Crossref][PubMed]
- Treggiari MM, Romand JA, Yanez ND, et al. Randomized trial of light versus deep sedation on mental health after critical illness. Crit Care Med 2009;37:2527-34.[Crossref][PubMed]
- Kress JP, Gehlbach B, Lacy M, et al. The long-term psychological effects of daily sedative interruption on critically ill patients. Am J Respir Crit Care Med 2003;168:1457-61.[Crossref][PubMed]
- Strøm T, Stylsvig M, Toft P. Long-term psychological effects of a no-sedation protocol in critically ill patients. Crit Care 2011;15:R293.[Crossref][PubMed]
- Jackson DL, Proudfoot CW, Cann KF, et al. The incidence of sub-optimal sedation in the ICU: a systematic review. Crit Care 2009;13:R204.[Crossref][PubMed]
- Van Rompaey B, Elseviers MM, Van Drom W, et al. The effect of earplugs during the night on the onset of delirium and sleep perception: a randomized controlled trial in intensive care patients. Crit Care 2012;16:R73.[Crossref][PubMed]
- Buscemi N, Vandermeer B, Hooton N, et al. Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ 2006;332:385-93.[Crossref][PubMed]
- Ibrahim MG, Bellomo R, Hart GK, et al. A double-blind placebo-controlled randomised pilot study of nocturnal melatonin in tracheostomised patients. Crit Care Resusc 2006;8:187-91.[PubMed]
- Shilo L, Dagan Y, Smorjik Y, et al. Effect of melatonin on sleep quality of COPD intensive care patients: a pilot study. Chronobiol Int 2000;17:71-6.[Crossref][PubMed]
- Mistraletti G, Umbrello M, Sabbatini G, et al. Melatonin reduces the need for sedation in ICU patients: a randomized controlled trial. Minerva Anestesiol 2015;81:1298-310.[PubMed]
- Martinez FE, Anstey M, Ford A, et al. Prophylactic Melatonin for Delirium in Intensive Care (Pro-MEDIC): study protocol for a randomised controlled trial. Trials 2017;18:4.[Crossref][PubMed]
- Practice guideline for the treatment of patients with delirium. American Psychiatric Association. Am J Psychiatry 1999;156:1-20.[PubMed]
- Skrobik YK, Bergeron N, Dumont M, et al. Olanzapine vs haloperidol: treating delirium in a critical care setting. Intensive Care Med 2004;30:444-9.[Crossref][PubMed]
- Milbrandt EB, Kersten A, Kong L, et al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med 2005;33:226-9; discussion 263-5.[Crossref][PubMed]
- Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the mnagement of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263-306.[Crossref][PubMed]
Cite this article as: Joseph A. Sedation of the trauma patient in the intensive care unit. J Emerg Crit Care Med 2018;2:8.



