
The acute respiratory distress syndrome: a clinical review
Introduction
The acute respiratory distress syndrome (ARDS) contributes greatly to the morbidity and mortality of patients admitted to intensive care units. Over the past several decades, a significant amount of research has been devoted to understanding the pathophysiology of the disease, improving ventilator management strategies, and trialing auxiliary medications. The goal of this research has been to provide practitioners with guided management recommendations to minimize lung injury and improve survival. Despite attempts to create a standardized definition of the disease, reports of the incidence of ARDS vary between countries worldwide. Prospective cohort studies from the United States published in the early 2000s have estimated the incidence in mechanically ventilated patients to be 64.2 to 78.9 cases/100,000 person years. Lower incidence rates have been reported in Europe. For example, in Northern Europe incidence rates have been reported to be 17 cases/100,000, while in Spain they have been reported to be as low as 7.2 cases/100,000 (1,2). A recent international observational study documented the prevalence of ARDS in intensive care units worldwide to be 10.4% of admissions during a four-week time period (3). Even in the era of protective lung ventilation strategies, the overall intensive care unit and hospital mortality of ARDS is reported to be between 40–50% (4).
Definition
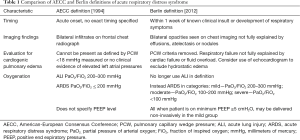
The initial description of ARDS was published in a paper by Ashbaugh and colleagues in 1967. The disease was described as an acute lung injury (ALI) syndrome resulting in severe hypoxemic respiratory failure refractory to supplemental oxygen caused by trauma, sepsis, or aspiration (5). Since that time, there has been much knowledge gained about the pathogenesis, epidemiology, and outcomes of these patients. Multiple attempts have been made at standardizing a definition of the disease in order to allow for proper diagnosis and targeted research efforts. In 1994, the American-European Consensus Conference on ARDS achieved consensus definitions for both ALI and ARDS. They described both diseases as characterized by acute onset of hypoxemia, bilateral infiltrates on frontal chest radiograph, and with a pulmonary artery wedge pressure less than 18 mmHg or absence of left atrial hypertension. Patients with PaO2/FiO2 ratio <300 mmHg fell into the ALI category while patients with PaO2/FiO2 ratio <200 mmHg fell into the category of ARDS (6). This description paved the way for research efforts focused on ARDS by providing a definition that could be used to evaluate clinical and epidemiologic data. Criticisms to the reliability and validity of the definition led to its revision and the establishment of the Berlin Criteria. The development of the Berlin Criteria focused on feasibility, reliability, validity, and objective evaluation of its performance. The Berlin criteria were empirically evaluated using a meta-analysis of greater than 4,000 patients with ARDS. The conclusion was a disease characterized by hypoxemic respiratory failure occurring less than seven days from a predisposing clinical insult, with bilateral opacities on chest radiograph or computed tomography (CT) not fully explained by effusion, atelectasis, or nodules. According to the new definition, the respiratory failure cannot be fully explained by cardiogenic pulmonary edema or volume overload. Oxygenation was redefined and split into three categories and ALI was removed from the definition (Table 1). When compared to the AECC definition, the Berlin criteria had a small but statistically significant advantage in predictive validity for mortality, (AOC 0.577 vs. AOC 0.536) (7,8).
Full table
Pathophysiology
A multitude of etiologies have the potential to trigger the clinical syndrome of ARDS. These have been grouped into direct and indirect causes of the disease. Direct causes would include those that cause primary injury to the lung epithelium, such as: pneumonia, aspiration, toxic inhalation, drowning. Indirect causes would include those that the cause lung injury in the setting of systemic inflammation and diffusely damage the vascular endothelium of the lung. These include but are not limited to extra-pulmonary sepsis, non-cardiogenic shock, trauma, transfusions, pancreatitis, drug overdose, and vasculitis (3,9). ARDS develops after one of these insults provokes a dysregulated host systemic inflammatory response in the lung, usually within the first 12–48 hours of exposure. Diffuse injury to the alveolar capillary membrane precipitates edema of the airspaces and interstitium with development of a protein rich neutrophilic exudate compromising gas exchange and reducing lung compliance (10).
The histological hallmark of ARDS is diffuse alveolar damage (DAD). This has been described as a manifestation of injury to the alveolar lining and the endothelial cells with the characteristic finding of hyaline membranes. Early in the disease course pathologic findings include capillary congestion, intra-alveolar edema, atelectasis, and hemorrhage. In the later phase of the disease, a mononuclear cell infiltrate invades the alveolar space and there is development of interstitial fibrosis (10-12). Pathologic findings of patients with direct versus indirect ARDS have found to be different. Pulmonary specimens of patients with direct pulmonary causes of ARDS have been found to have higher amounts of DAD as compared to samples of patients with extra-pulmonary causes (13). Researchers examining post-mortem lung samples of patients with ARDS found those with direct causes had a predominance of alveolar collapse, fibrinous exudate, and alveolar wall edema compared to those with indirect causes of ARDS (14). Another similar evaluation of autopsy samples of patients in the early phase of the disease showed greater collagen content in samples of patients who had direct pulmonary causes of ARDS consistent, with early remodeling of the extracellular matrix (15). Animal models have demonstrated that direct lung injury is associated with greater alveolar inflammation, and is associated with more damage and worsened lung mechanics (9). Understanding the differences in damage to the epithelium and endothelium between each type of ARDS insult may help to tailor novel targets for treatment beyond our current methods of mechanical ventilation.
Clinically, patients with direct and indirect ARDS were shown to have similar mortality (28% vs. 31%, respectively). However, many other parameters differ between these two categories. Patients with direct ARDS had higher lung injury scores but lower Simplified Acute Physiology (SAPS) II and Acute Physiology and Chronic Health Evaluation (APACHE) II scores as well as fewer non-pulmonary organ failures. Increasing age and lung injury score was predictive of mortality in direct ARDS only. The only predictor of mortality in indirect ARDS was number of organ failures (16).
Diagnosis
Early recognition of ARDS is important for timely initiation of lung protective ventilation strategies. Even after attempts to improve the definition of the disease, ARDS remains under-recognized by clinicians. Oftentimes when a diagnosis is made, it has been after a significant delay. The rate of under diagnosis is reported to be as high as 40%, with higher rates of diagnosis with increasing disease severity (3). ARDS is a syndrome with several different clinical criteria that must be fulfilled; however none of these data points are particularly precise. The current clinical criteria have low specificity, for example, 63% for the Berlin definition to identify DAD at autopsy. There is not currently a biomarker to aid in the diagnosis, and this is now an area of much active research (17). Chest X-rays for the diagnosis of ARDS have a relatively low sensitivity and specificity of approximately 70% when compared to CT scans. CXR performs better when the infiltrates are diffuse or patchy as opposed to focal (18). The use of CT scans and other imaging techniques in the diagnosis and management of ARDS is become increasingly important. Studies focusing on the use of CT scans have demonstrated that the densities seen in ARDS are not homogeneously diffuse, as they sometimes appear on chest radiograph. Instead, the densities are mainly localized to the dependent zones of the lung. Visual inspection of CT scans allows measurements of lung weight, the amount of open tissue, and the percentage of lung that has the potential to be recruited with positive end expiratory pressure (PEEP) and prone positioning (19). Lung ultrasound is another modality that can be used as a bedside tool to facilitate the diagnosis of ARDS. Findings of multiple B lines in a non-homogenous and non-gravity dependent distribution, with decreased or absent lung sliding, consolidation in dependent lung regions, and spared areas in the anterior region have been described as specific findings in patients with ARDS. This has been compared to patients with other causes of acute respiratory failure, including cardiogenic pulmonary edema, COPD/asthma, pulmonary embolism, and pneumothorax (20). One study evaluated the use of ultrasound and a SpO2/FiO2 ratio to diagnose ARDS, utilizing chest X-ray as the reference standard. They demonstrated a sensitivity and specificity for ultrasound of 80% and 62%, respectively. When combining ultrasound with a SpO2/FiO2 ratio ≤315 the sensitivity was 83% with an unchanged specificity (21).
When ARDS is suspected, identification and treatment of the underlying etiology is of significant importance. Infection, whether from a pulmonary or extra-pulmonary source, is one of the leading causes of lung injury in ARDS. Attempts should be made to identify the responsible pathogen in order to target antimicrobial treatment. The differential diagnosis is often broad and can include community or hospital acquired bacterial infection, as well as viral, fungal, or parasitic organisms. Recognition of patients who are immunocompromised is crucial, as the risk of infection with certain specific organisms will require medications that can significantly alter the clinical outcome. Careful review of medications and exposures is paramount, as removal of an offending agent responsible for the disease will be potentially therapeutic. Bronchoalveolar lavage is often utilized for direct sampling of the intra-alveolar material and in some cases where the etiology is not as clear, open lung biopsy may be indicated (11).
Treatments
Mechanical ventilation
Overview
Treatment of ARDS continues to be largely supportive and mostly reliant on mechanical ventilator strategies as the underlying disease process is given the time to resolve. Respiratory mechanics and lung recruitability vary widely between patients, and treatment planning should be performed carefully with therapy tailored to each individual person. The primary goal is to allow for adequate gas exchange in a manner that simultaneously reduces the risk of ventilator induced lung injury (VILI). While mechanical ventilation has been shown to delay mortality and maintain adequate systemic oxygenation in patients with acute respiratory failure, it also has the power to cause or augment existing lung injury. This injury may be indistinguishable from that caused by the underlying disease process. Several forms of VILI are recognized. During mechanical ventilation, the risk of raising transpulmonary pressure to an unphysiologic level creates undo stress and strain resulting in barotrauma and volutrauma (22). More obvious injuries related to barotrauma, such as pneumothorax or pneumomediastinum, are not uncommon complications of an increase in transpulmonary pressure (23). Volutrauma and atelectrauma can create an equally dangerous inflammatory reaction at the molecular level (24). Decades ago, researchers discovered that ventilation can have a significant influence on the inflammatory milieu of the lung. Early studies performed on alveolar lavage samples in animal models have demonstrated that utilization of ventilator strategies employing low end inspiratory lung volumes or high end expiratory volumes overall had lower cytokine levels in the lavage fluid than in those that did not use this lung protective ventilator strategy (25). Similar findings have also been reproduced in human lavage samples of patients with ARDS. The concentration of inflammatory mediators and polymorphonuclear cells are decreased in bronchoalveolar lavage samples when a lung protective ventilator strategy is utilized (26). Much of the research effort has focused on ways to improve oxygenation while reducing VILI by identifying optimal set tidal volumes, PEEP settings, lung recruitment maneuvers, and body positioning during mechanical ventilation.
Setting a tidal volume
Traditional approaches to mechanical ventilation allowed for tidal volumes of up to 10–15 milliliters (mL) per kilogram (kg) of body weight in order to achieve normal partial pressure of arterial carbon dioxide levels and pH. In the modern era, a ventilator strategy using a reduction in the tidal volume to 6 mL per kilogram of ideal body weight, and reducing plateau pressures, has shown to reduce the number of days on the ventilator and mortality among patients with ARDS by 22% (27). These findings were confirmed in two recent meta-analyses that showed a significant reduction in 28-day mortality with lung protective ventilation strategies (28,29). The widely adapted ARDSnet protocol requires the use of a patient’s ideal body weight to calculate the dose of volume delivered per breath, as actual body weight is not an accurate index of lung size. The goal of 6 mL/kg can be achieved with either pressure or volume regulated breath cycles, in addition, the recommended goal plateau pressure is less than 30 mmHg. These recommendations challenge the previous goal of normalizing arterial blood gas values, and require practitioners to feel comfortable with a certain degree of respiratory acidosis that may be associated with air hunger, ventilator dyssynchrony, and alterations in hemodynamics. Therefore, this protocol allows for a degree of permissive hypercapnia with goal pH between 7.3–7.45 (27). Although we know the development of VILI is proportional to the external energy applied by the ventilator to the lung, it has been shown that reducing the tidal volume merely based on the patient’s ideal body weight may not always prevent VILI. This is due to the fact that the distribution of the diseased lung and the lung available for ventilation is not uniform among patients. This “baby lung” concept allows for the understanding that there are two regions of the lung in ARDS. One region is nearly normal with dimensions similar to those of a healthy baby, and the second is consolidated and collapsed and responsible for the impairment of oxygenation. This was first noted on observations of the first CT scan images of patients with ARDS that showed densities in the dependent lung regions with sparing of the non-dependent lung regions (30). Those patients who have a large amount of poorly aerated or non-aerated compartments may have hyperinflation of the normally aerated compartments of the lung, thus perpetuating lung injury. Therefore, limiting tidal volume to 6 ml/kg of ideal body weight may not be sufficient in those patients who have larger non-aerated components of the lung (31). Research has recently been focused on examination of airway driving pressure as a measurement of the risk of lung injury during mechanical ventilation. Airway driving pressure is measured as the airway pressure changes from PEEP to end-inspiratory plateau pressure and is equivalent to the ratio between the tidal volume and the compliance. Taking into account airway driving pressure may better reflect the stress and strain that can promote VILI. A recent study highlighted the measurement of airway driving pressures as a useful tool to titrate delivery of tidal volumes and pressures. Doing so may allow physicians to accurately uncover higher lung stress, and higher lung elastance when compared to those patients with lower airway driving pressures (32).
Lung recruitment and titrating PEEP
Loss of lung volume due to alveolar filling with edema and neutrophilic proteinaceous material, atelectasis, and consolidation are characteristic components of ARDS. The use of PEEP has been studied extensively as a means to combat these abnormalities (5). The goal of using PEEP in ARDS is not only to improve oxygenation, but to recruit atelectatic or flooded lung and prevent the repetitive opening and closing of alveoli during the respiratory cycle. The result of using PEEP is an increase in end-expiratory lung volume (EELV). If a patient has a substantial amount of recruitable lung tissue, the EELV can be increased substantially by opening atelectatic lung tissue providing substantial benefits toward improving oxygenation. If a patient has minimal recruitable lung tissue, an increase in EELV can potentially lead to over-distention and VILI with failure to recruit any collapsed alveoli (33). Several large randomized trials have studied high versus low levels of PEEP, all while limiting tidal volumes and plateau pressures. None found any significant improvement in mortality, but did uncover some benefit with regards to the secondary endpoints of hypoxemia, end organ dysfunction, and ventilator free days (34-36). The concern is that these studies, testing incremental higher levels of PEEP, were confounded by baseline prognostic factors and were underpowered to detect a difference in survival. A subsequent meta-analysis of the trials did demonstrate mortality benefit when higher levels of PEEP were applied to a subgroup of patients labeled as having ARDS at baseline with a cutoff PaO2/FiO2 ratio less than 200 mmHg when compared to patients without ARDS at baseline or PaO2/FiO2 ratio higher than 200 mmHg (37). Questions still remain on how to titrate to the optimal amount of PEEP for each individual patient, with the goal of keeping the alveoli open and at the same time minimizing VILI and hemodynamic compromise. There are various proposed ways of titrating PEEP that are used by clinicians. A popular method is to titrate PEEP to a certain level of oxygenation, however there can be downsides to doing this alone out of concerns for precipitating lung injury and compromising hemodynamics. Another commonly practiced method began with the ARDSNET study, whereby a pre-set table is used to guide adjustment of PEEP according to the level of FiO2 that is set (27,36). Another method, which has been studied in animal models, is to use a pressure volume curve and maintain a constant tidal volume and increase PEEP in a stepwise manner while monitoring for excessive elevations in airways pressures (38). Others propose the “open lung concept” where a recruitment maneuver is performed, followed by a decremental reduction in PEEP until there is deterioration in compliance or oxygenation. This allows for titrating down to the minimum PEEP required to prevent derecruitment (39). Some researchers have looked at the use of measuring variation in esophageal pressure using esophageal balloon catheters to estimate transpulmonary pressure as a marker of lung stress (40). Other recommendations include visual assessment of alveolar recruitability via identification of lung collapse on CT scan, however given the time consuming nature and risk of repeated radiation exposure, risk practicality of this method remains in question. Practitioners currently use all of these approaches to varying degrees, however they still require further validation studies.
Use of proning
The benefits of the prone position can be described by the “shape matching” model. In the supine position, there is a decrease in size of alveoli from sternum to vertebrae. There is also a difference in shape that exists between the lung and the chest wall, which results in non-homogenous expansion of the alveolar units in order for them to occupy the same volume. This ultimately generates greater distention in the ventral lung regions. The “shape-matching model” describes a lung that naturally forms a conical shape but has to fit into the rigid cylinder of the chest wall. In this model the upper lung zones expand more than the lower ones (41). During pronation, the opposite is true such that the gravitational forces compress the ventral region. The need for the lung and chest wall to adapt their shapes in this position, allows for both to regionally expand, thus dampening the forces that compress the ventral region of the lung. The overall result of proning is that lung inflation is more homogenous from dorsal to ventral than in the supine position. In ARDS there is an overall increased lung mass and the dependent area of the lung collapses due to edema and an increased superimposed pressure. Proning allows for increased aeration and recruitment of these regions of the lung, which exceeds any derecruitment that will occur in the ventral regions of the lung (42). There have been five major trials over the past 15 years evaluating prone positioning. The first four demonstrated some improvement in oxygenation, and only a small but not statistically significant benefit in mortality. This was, however met with some safety concerns. Patients in each trial had progressively more severe disease and the prone positioning was tested at longer intervals each time (43-46). Proning Severe ARDS Patients (PROSEVA), one of the most recent trials, included patients with severe ARDS which they defined as PaO2/FiO2 ratio less than 150 mmHg. Patients were prone for 16 hours per day for approximately 4 days while employing low tidal ventilation and PEEP selection as per the ARDSnet table. The results showed a significant decrease in both 28- and 90-day mortality, with ARR of 17% for proned patients (47). After this trial, prone positioning has been suggested for patients with moderate to severe ARDS with PaO2/FiO2 ratio less than 150 mmHg with PEEP equal or greater to 5 cmH2O and an FiO2 greater than or equal to 0.6. Absolute contraindications to prone positioning include spinal instability and increased intracranial pressure. Relative contraindications include open abdominal wounds, unstable fractures, pregnancy, and severe hemodynamic instability. The risks of extubation and line removal are real with proning, and the practice should be performed at a center with experienced staff and clinicians carefully weighing the risks and benefits for each individual patient (42).
Non-invasive ventilation (NIV)
The use of NIV has shown to produce positive outcomes in patients with hypercapnic respiratory failure, COPD exacerbation, and cardiogenic pulmonary edema (48,49). The utility of NIV in ARDS is still under debate, with concerns of a high risk of failure and delay to mechanical ventilation. A multicenter study in 2001 uncovered an eventual intubation rate of 51% in ARDS patients treated initially with NIV, with the risk of failure being highest in those with a higher SAPS II score or older age. Among those patients treated with NIV initially, there was a longer duration of ICU stay and higher ICU mortality (50). A recent observational study also shed light on the concerns of the use of NIV in patients with moderate to severe ARDS. The study examined a cohort of patients with hypoxemic respiratory failure from all causes receiving NIV. The subgroup of ARDS patients, specifically those with a PaO2/FiO2 ratio <150, had a significantly higher intubation and ICU mortality rate when compared to non-ARDS patients (51). A recent single center trial comprised only of patients with ARDS evaluated different interfaces of NIV. Patients were assigned to nasal facemask or helmet mask, and those assigned to helmet NIV required intubation less often and had higher survival rate. This poses the question of whether the mode of delivery of the NIV (i.e., with nasal mask or facemask instead of helmet) affected its efficacy in this trial as well as in previous trials (52). High Flow Nasal Cannula (HFNC) has also been considered as a treatment for patients with ARDS as an alternative to NIV or mechanical ventilation. HFNC allows oxygen to be delivered via a higher flow (up to 60 L/min) while at the same time being heated and humidified via a wide bore nasal cannula. This device minimizes oxygen dilution and allows the delivered FiO2 to be as close to the set FiO2 as possible. HFNC has also been found to generate a certain amount of PEEP, and has the effect of decreased work of breathing (53). A single observational study looked at the use of HFNC in patients with acute respiratory failure, 45 of whom had ARDS and found a 40% secondary intubation rate. Interestingly, 82% of these patients had pneumonia as the etiology of respiratory failure. It is difficult to ascertain if HFNC avoided intubation in some subjects, or if those patients would have improved regardless (54). More investigation with a larger number of subjects is needed in order to answer this question.
Non-ventilatory treatments
Neuromuscular blockade
Oftentimes, patients with ARDS will have severe gas exchange impairments, and the use of sedative medications alone to adequately facilitate mechanical ventilation will prove to be insufficient, especially when trying to enforce lower delivered tidal volumes. The use of neuromuscular blockade agents (NMBA) in the ICU has been a common practice among physicians with several indications cited in the literature, including the facilitation of mechanical ventilation, control of ICP, ablation of muscle spasms associated with tetanus, and decreasing oxygen consumption of the skeletal muscles. Non-depolarizing NMBAs are most commonly used in intensive care units. They work as competitive antagonists of the acetylcholine receptors by binding to the receptor and preventing depolarization of the post synaptic membrane of the muscle by acetylcholine (55). The use of NMBA in ARDS became an area of interest to researchers in the early 2000s, during which time three RCTs were published. The first, randomized patients to 48 hours of cisatracurium vs. placebo and found a statistically significant improvement in the primary endpoint of oxygenation through 120 hours after randomization, with a trend towards improvement in mortality, which unfortunately was not statistically significant (56). Researchers then evaluated the effect of NMBA on pulmonary and systemic inflammation in patients with ARDS and found a decrease in IL-1, IL-6, and IL-8 in BAL and IL-1, and IL-6 in the serum of patients given NMBA after 48 hours of treatment (57). In 2010, a multicenter RCT demonstrated a mortality benefit before discharge or at 90 days when cisatracurium was used early in the course of severe ARDS. This benefit was shown after adjustment for PaO2 to FiO2 ratio, SAPS II score, and plateau pressure. The greatest benefit was demonstrated in patients with PaO2/FiO2 ratio less than 120 mmHg (58).
A meta-analysis in 2012 including these three RCTs found that that use of NMBA in the early phase of ARDS improves overall outcomes as demonstrated by increased overall ICU survival and survival at 28 days, as well as a higher number of ventilator free days. In addition, they found an overall increase in the PaO2/FiO2 ratio and reduced incidence of barotrauma. The incidence of critical illness neuropathy was similar between the intervention and control groups (59). The main concern with using NMBA is the potential development of critical illness polyneuropathy and myopathy (CIPM). The risk is higher with prolonged use of these agents, concomitant corticosteroid administration and in patients with septic shock. However, there is little evidence showing harm with use of NMBA for less than 48 hours (60).
In 2016 the clinical practice guidelines for use of NMBA in critically ill patients was updated to reflect the recent research. Recommendations now specifically include the use of NMBA administration via continuous IV infusion early in the course of ARDS with a PaO2/FiO2 ratio of <150 mmHg (61).
Fluid management
One question that had remained unanswered for some time was the optimal fluid management in patients with ARDS. One main component in the pathophysiology of ARDS is injury to the alveolar capillary membrane generating edema in the airspaces and interstitium. Researchers theorized that a more conservative fluid management strategy may in fact improve outcomes in ARDS. The Fluids and Catheters Treatment Trial (FACTT) was a multicenter RCT that looked at 1,000 intubated patients with ARDS diagnosed within 48 hours and randomized them to conservative versus liberal fluid management strategies as measured by central venous pressure (CVP) and pulmonary capillary wedge pressure (PCWP). The group assigned to a conservative strategy had an overall statistically significant less net positive fluid balance than the liberal fluid management group. There was not a significant difference in the primary outcome of all-cause mortality, however results showed the conservative strategy group had more ventilator free days, and ICU free days as well less extra-pulmonary organ dysfunction. The patients in this study were not hemodynamically unstable, so the results cannot be generalized to the entire population of patients with ARDS, as we know hemodynamics will vary based on severity of illness and additional comorbidities. The other caveat to this study is that there was a significant amount of diuretic use in the conservative management group to keep the patients closer to net even (62). Based on that trial, it is now recommended to continue with a conservative fluid strategy in patients with ARDS who do not require aggressive fluid resuscitation for other reasons.
Corticosteroid therapy
We understand from years of extensive research into the pathophysiology of ARDS, that there is a hallmark of dysregulated inflammation. This inflammatory response is compounded by the use of mechanical ventilation, which increases the risk of VILI, further perpetuating the inflammatory response both in the lung and systemically. Corticosteroids work to inhibit inflammatory and immune responses to a diverse number of inflammatory insults via several signaling pathways with positive therapeutic effects (63). The use of corticosteroids has been studied for both the prevention and treatment of ARDS. Several trials in the 1980s looked at corticosteroids for the prevention of ARDS in patients with sepsis, trauma, pneumonia, aspiration, and burns. Not only were steroids found to be of little use in prevention, but there was an association with increased development of ARDS coupled with increased infectious complications and mortality (64,65). Trials evaluating the use of corticosteroids for treatment of known ARDS have shown conflicting results. For example, in 1998 a RCT of 24 patients showed a decrease in hospital mortality for those patients receiving corticosteroids after 7 days of mechanical ventilation, sparking the idea that steroids could possibly be beneficial in the late phase of ARDS (66). These results were sharply contrasted by the Late Steroid Rescue Study (LaSRS) published in 2006, which randomized patients with methylprednisolone after at least 7 days of mechanical ventilation and showed no mortality benefit and an increased risk of death if steroids were started more than 14 days after the onset of ARDS (67). Another group of investigators performed a secondary analysis of a prospective randomized control trial originally looking at statin use in ARDS. The secondary analysis focused on the use of IV or PO corticosteroids in this population totaling more than 20 mg methylprednisolone equivalents. They found that corticosteroids were more likely to be used in patients who were more critically ill, with higher APACHE scores, and in the group of patients who were non-survivors. Overall there was not a mortality benefit found for the use of corticosteroids in that analysis (68). The effect of corticosteroid therapy on mortality continues to remain uncertain. For now steroids are not routinely recommended for use in for treatment of ARDS, and more conclusive data is needed to answer the question of steroid utility in this disease (69).
Pulmonary vasodilators
Inhaled vasodilators are another group of auxiliary medications that have been studied as a potential therapy for patients with ARDS. Their mechanism of action is to dilate pulmonary vasculature in the well-ventilated areas of the lungs, thereby decreasing overall pulmonary arterial pressure and vascular resistance and improving ventilation-perfusion mismatch and oxygenation. Inhaled nitric oxide (INO) is the most studied selective pulmonary vasodilator in ARDS. INO has been found to improve oxygenation in patients with ARDS and severe hypoxemia, as well as to prevent cardiovascular collapse in patients who have developed right ventricular failure (70). Despite these physiologic benefits of INO, the evidence for a meaningful benefit in patients is lacking. A systematic review and meta-analysis of nine trials randomizing patients with ARDS to treatment with 5–10 ppm of INO versus placebo found that INO does not reduce hospital mortality in patients regardless of the severity of hypoxemia.
Given this finding, along with the high cost associated with of use of INO, it is not routinely recommended for use in patients with severe ARDS (71).
Extracorporeal membrane oxygenation (ECMO)
Respiratory support via veno-venous ECMO has been considered as a treatment for those in severe acute respiratory failure. ECMO has the potential to reduce or eliminate the effects of positive pressure ventilation by serving as an adjunct to mechanical ventilation, or in place of it in some cases. The use of ECMO became popular in 2009 and 2010 when there was a high rate of morbidity and mortality among young patients with pneumonia and ARDS as a result of the H1N1 pandemic. In this group, ECMO showed some promise of a favorable outcome (72). Several other studies conducted during this same time period produced mixed results (73). One of the most well-known trials in the critical care literature, the Conventional ventilation or ECMO for Severe Adult Respiratory failure (CESAR) trial, was conducted as a multicenter trial in the UK around the same time period. The objective was to formally evaluate the use of ECMO as a treatment for patients with severe but presumed reversible ARDS. Patients were randomized to conventional mechanical ventilation vs. ECMO and investigators reported a higher rate of survival without disability after 6 months in those placed on ECMO. Limitations to this study include the fact that not all patients who were randomized to ECMO received it, and practices in the control arm were not standardized. These limitations left it difficult to make conclusions and to define the role of ECMO in adults with severe ARDS (74). ECMO is an endeavor that requires significant resources and referral to a center that has a multidisciplinary team trained in its implementation and use. Although there are not concrete recommendations on the use of ECMO in respiratory failure, patients are still being referred to select centers, and ideally more controlled trials are needed to define indications for this therapy.
Future directions
Much of the research on ARDS to date has been focused on patients with already established lung injury of varying degrees of severity. These studies have focused on management strategies to reduce further lung injury and mortality. In recent years, there has been a shift of focus that is centered on prevention of the disease. The National Heart, Lung and Blood Institute (NHLBI) awarded funding for the formation of a network of 12 clinical centers to perform clinical trials under the title Prevention and Early Treatment of Acute Lung Injury (PETAL). The purpose of this network is to develop innovative approaches to prevent and improve outcomes of patients at risk for ARDS. Collaborative partnership with those who care for patients when the development of the inciting disease occurs, i.e., emergency medicine and primary physicians is one of these goals, as this is a crucial part in prevention of disease. Focusing on prevention of the most common etiologies of ARDS will prove to be important in the coming years. Strategies to optimize vaccination of patients for influenza and pneumococcus, as well as proper practice of aspiration precautions, early recognition of sepsis, reduction of excessive fluid administration, and restrictive transfusion protocols are all high yield areas of research. There has also been interest in development of clinical prediction scores to evaluate the likelihood of development of ARDS such as the Lung Injury Prediction Score (LIPS) (75). Pharmacological therapies for prevention of ARDS are now also being investigated. Previous observational studies had suggested a potential role for antiplatelet therapy in patients at high risk for ARDS. A recent RCT evaluated the use of aspirin as prevention in adult patients admitted to the emergency department at high risk for developing ARDS. Results suggested there was no effect on the incidence of the disease in these patients (76). There has been a large focus on identifying biomarkers associated with the development of ARDS or the risk of mortality among patients already diagnosed with the disease. Several biomarkers including KL-6, LDH, sRAGE and vWF, have been found to have some clinical association with the development of ARDS. More research is needed in order to further validate the use of these markers in a widespread population (77).
Conclusions
Since the first definition of ARDS in the 1960s, we have come a long way in the understanding of the disease and development of treatment options. Despite this, the incidence remains high, and there is a significant overall reported mortality. Early identification of patients at risk, rapid identification of the underlying cause, and early lung protective management strategies are crucial. Mechanical ventilation strategies should focus on minimizing lung injury, while at the same time allowing for adequate gas exchange and focus on preventing extra-pulmonary organ injury. It should be understood that all patients will present with different lung mechanics, and lung recruitability needs to be assessed in each patient individually when formulating a treatment strategy. The upfront use of neuromuscular blockade should be a consideration for the first 48 hours and prone positioning should be considered in patients with severe ARDS who have the highest potential for benefit. The critical care community is now focused on conducting trials that will assist with uncovering strategies aimed at prevention of the disease. Partnership with our emergency medicine and primary care colleagues is now the future of research to help identify patients at risk of the disease before they end up in the intensive care unit.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Walkey AJ, Summer R, Ho V, et al. Acute respiratory distress syndrome: epidemiology and management approaches. Clin Epidemiol 2012;4:159-69. [Crossref] [PubMed]
- Rubenfeld GD, Caldwell E, Peabody E, et al. Incidence and outcomes of acute lung injury. N Engl J Med 2005;353:1685-93. [Crossref] [PubMed]
- Bellani G, Laffey JG, Pham T, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016;315:788-800. [Crossref] [PubMed]
- Villar J, Blanco J, Anon JM, et al. The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive Care Med 2011;37:1932-41. [Crossref] [PubMed]
- Ashbaugh DG, Bigelow DB, Petty TL, et al. Acute respiratory distress in adults. Lancet 1967;2:319-23. [Crossref] [PubMed]
- Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:818-24. [Crossref] [PubMed]
- Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012;307:2526-33. [PubMed]
- Ferguson ND, Fan E, Camporota L, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med 2012;38:1573-82. [Crossref] [PubMed]
- Shaver CM, Bastarache JA. Clinical and biological heterogeneity in acute respiratory distress syndrome: direct versus indirect lung injury. Clin Chest Med 2014;35:639-53. [Crossref] [PubMed]
- Meduri GU, Annane D, Chrousos GP, et al. Activation and regulation of systemic inflammation in ARDS: rationale for prolonged glucocorticoid therapy. Chest 2009;136:1631-43. [Crossref] [PubMed]
- Papazian L, Calfee CS, Chiumello D, et al. Diagnostic workup for ARDS patients. Intensive Care Med 2016;42:674-85. [Crossref] [PubMed]
- Katzenstein AL, Bloor CM, Leibow AA. Diffuse alveolar damage--the role of oxygen, shock, and related factors. A review. Am J Pathol 1976;85:209-28. [PubMed]
- Peres e Serra A, Parra ER, Eher E, et al. Nonhomogeneous immunostaining of hyaline membranes in different manifestations of diffuse alveolar damage. Clinics (Sao Paulo) 2006;61:497-502. [Crossref] [PubMed]
- Hoelz C, Negri EM, Lichtenfels AJ, et al. Morphometric differences in pulmonary lesions in primary and secondary ARDS. A preliminary study in autopsies. Pathol Res Pract 2001;197:521-30. [PubMed]
- Negri EM, Hoelz C, Barbas CS, et al. Acute remodeling of parenchyma in pulmonary and extrapulmonary ARDS. An autopsy study of collagen-elastic system fibers. Pathol Res Pract 2002;198:355-61. [Crossref] [PubMed]
- Luo L, Shaver CM, Zhao Z, et al. Clinical Predictors of Hospital Mortality Differ Between Direct and Indirect ARDS. Chest 2017;151:755-63. [Crossref] [PubMed]
- Laffey JG, Pham T, Bellani G. Continued under-recognition of acute respiratory distress syndrome after the Berlin definition: what is the solution? Curr Opin Crit Care 2017;23:10-7. [Crossref] [PubMed]
- Figueroa-Casas JB, Brunner N, Dwivedi AK, et al. Accuracy of the chest radiograph to identify bilateral pulmonary infiltrates consistent with the diagnosis of acute respiratory distress syndrome using computed tomography as reference standard. J Crit Care 2013;28:352-7. [Crossref] [PubMed]
- Pesenti A, Musch G, Lichtenstein D, et al. Imaging in acute respiratory distress syndrome. Intensive Care Med 2016;42:686-98. [Crossref] [PubMed]
- Lichtenstein DA, Meziere GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 2008;134:117-25. [Crossref] [PubMed]
- Bass CM, Sajed DR, Adedipe AA, et al. Pulmonary ultrasound and pulse oximetry versus chest radiography and arterial blood gas analysis for the diagnosis of acute respiratory distress syndrome: a pilot study. Crit Care 2015;19:282. [Crossref] [PubMed]
- Gattinoni L, Marini JJ, Collino F, et al. The future of mechanical ventilation: lessons from the present and the past. Crit Care 2017;21:183. [Crossref] [PubMed]
- Hsu CW, Sun SF. Iatrogenic pneumothorax related to mechanical ventilation. World J Crit Care Med 2014;3:8-14. [Crossref] [PubMed]
- Protti A, Andreis DT, Milesi M, et al. Lung anatomy, energy load, and ventilator-induced lung injury. Intensive Care Med Exp 2015;3:34. [Crossref] [PubMed]
- Tremblay L, Valenza F, Ribeiro SP, et al. Injurious ventilatory strategies increase cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest 1997;99:944-52. [Crossref] [PubMed]
- Ranieri VM, Suter PM, Tortorella C, et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA 1999;282:54-61. [Crossref] [PubMed]
- Brower RG, Matthay MA, Morris A, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8. [Crossref] [PubMed]
- Petrucci N, De Feo C. Lung protective ventilation strategy for the acute respiratory distress syndrome. Cochrane Database Syst Rev 2013.Cd003844. [PubMed]
- Burns KE, Adhikari NK, Slutsky AS, et al. Pressure and volume limited ventilation for the ventilatory management of patients with acute lung injury: a systematic review and meta-analysis. PLoS One 2011;6:e14623. [Crossref] [PubMed]
- Gattinoni L, Marini JJ, Pesenti A, et al. The "baby lung" became an adult. Intensive Care Med 2016;42:663-73. [Crossref] [PubMed]
- Terragni PP, Rosboch G, Tealdi A, et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med 2007;175:160-6. [Crossref] [PubMed]
- Chiumello D, Carlesso E, Brioni M, et al. Airway driving pressure and lung stress in ARDS patients. Crit Care 2016;20:276. [Crossref] [PubMed]
- Rittayamai N, Brochard L. Recent advances in mechanical ventilation in patients with acute respiratory distress syndrome. Eur Respir Rev 2015;24:132-40. [Crossref] [PubMed]
- Brower RG, Lanken PN, MacIntyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 2004;351:327-36. [Crossref] [PubMed]
- Mercat A, Richard JC, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 2008;299:646-55. [Crossref] [PubMed]
- Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 2008;299:637-45. [Crossref] [PubMed]
- Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA 2010;303:865-73. [Crossref] [PubMed]
- Protti A, Cressoni M, Santini A, et al. Lung stress and strain during mechanical ventilation: any safe threshold? Am J Respir Crit Care Med 2011;183:1354-62. [Crossref] [PubMed]
- Suarez-Sipmann F, Bohm SH. Recruit the lung before titrating the right positive end-expiratory pressure to protect it. Crit Care 2009;13:134. [Crossref] [PubMed]
- Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008;359:2095-104. [Crossref] [PubMed]
- Koulouras V, Papathanakos G, Papathanasiou A, et al. Efficacy of prone position in acute respiratory distress syndrome patients: A pathophysiology-based review. World J Crit Care Med 2016;5:121-36. [Crossref] [PubMed]
- Gattinoni L, Taccone P, Carlesso E, et al. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Respir Crit Care Med 2013;188:1286-93. [Crossref] [PubMed]
- Gattinoni L, Tognoni G, Pesenti A, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med 2001;345:568-73. [Crossref] [PubMed]
- Guerin C, Gaillard S, Lemasson S, et al. Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. Jama 2004;292:2379-87. [Crossref] [PubMed]
- Mancebo J, Fernandez R, Blanch L, et al. A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med 2006;173:1233-9. [Crossref] [PubMed]
- Taccone P, Pesenti A, Latini R, et al. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. Jama 2009;302:1977-84. [Crossref] [PubMed]
- Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013;368:2159-68. [Crossref] [PubMed]
- Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995;333:817-22. [Crossref] [PubMed]
- Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet 2009;374:250-9. [Crossref] [PubMed]
- Antonelli M, Conti G, Moro ML, et al. Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study. Intensive Care Med 2001;27:1718-28. [Crossref] [PubMed]
- Thille AW, Contou D, Fragnoli C, et al. Non-invasive ventilation for acute hypoxemic respiratory failure: intubation rate and risk factors. Crit Care 2013;17:R269. [Crossref] [PubMed]
- Patel BK, Wolfe KS, Pohlman AS, et al. Effect of Noninvasive Ventilation Delivered by Helmet vs Face Mask on the Rate of Endotracheal Intubation in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. Jama 2016;315:2435-41. [Crossref] [PubMed]
- Ricard JD. High flow nasal oxygen in acute respiratory failure. Minerva Anestesiol 2012;78:836-41. [PubMed]
- Messika J, Ben Ahmed K, Gaudry S, et al. Use of High-Flow Nasal Cannula Oxygen Therapy in Subjects With ARDS: A 1-Year Observational Study. Respir Care 2015;60:162-9. [Crossref] [PubMed]
- Murray MJ, Cowen J, DeBlock H, et al. Clinical practice guidelines for sustained neuromuscular blockade in the adult critically ill patient. Crit Care Med 2002;30:142-56. [Crossref] [PubMed]
- Gainnier M, Roch A, Forel JM, et al. Effect of neuromuscular blocking agents on gas exchange in patients presenting with acute respiratory distress syndrome. Crit Care Med 2004;32:113-9. [Crossref] [PubMed]
- Forel JM, Roch A, Marin V, et al. Neuromuscular blocking agents decrease inflammatory response in patients presenting with acute respiratory distress syndrome. Crit Care Med 2006;34:2749-57. [Crossref] [PubMed]
- Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 2010;363:1107-16. [Crossref] [PubMed]
- Neto AS, Pereira VG, Esposito DC, et al. Neuromuscular blocking agents in patients with acute respiratory distress syndrome: a summary of the current evidence from three randomized controlled trials. Ann Intensive Care 2012;2:33. [Crossref] [PubMed]
- Price D, Kenyon NJ, Stollenwerk N. A fresh look at paralytics in the critically ill: real promise and real concern. Ann Intensive Care 2012;2:43. [Crossref] [PubMed]
- Murray MJ, DeBlock H, Erstad B, et al. Clinical Practice Guidelines for Sustained Neuromuscular Blockade in the Adult Critically Ill Patient. Crit Care Med 2016;44:2079-103. [Crossref] [PubMed]
- Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006;354:2564-75. [Crossref] [PubMed]
- Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids--new mechanisms for old drugs. N Engl J Med 2005;353:1711-23. [Crossref] [PubMed]
- Weigelt JA, Norcross JF, Borman KR, et al. Early steroid therapy for respiratory failure. Arch Surg 1985;120:536-40. [Crossref] [PubMed]
- Luce JM, Montgomery AB, Marks JD, et al. Ineffectiveness of high-dose methylprednisolone in preventing parenchymal lung injury and improving mortality in patients with septic shock. Am Rev Respir Dis 1988;138:62-8. [Crossref] [PubMed]
- Meduri GU, Headley AS, Golden E, et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA 1998;280:159-65. [Crossref] [PubMed]
- Steinberg KP, Hudson LD, Goodman RB, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med 2006;354:1671-84. [Crossref] [PubMed]
- Zhang Z, Chen L, Ni H. The effectiveness of Corticosteroids on mortality in patients with acute respiratory distress syndrome or acute lung injury: a secondary analysis. Sci Rep 2015;5:17654. [Crossref] [PubMed]
- Lamontagne F, Brower R, Meade M. Corticosteroid therapy in acute respiratory distress syndrome. Cmaj 2013;185:216-21. [Crossref] [PubMed]
- Siobal MS, Hess DR. Are inhaled vasodilators useful in acute lung injury and acute respiratory distress syndrome? Respir Care 2010;55:144-57; discussion 157-61. [PubMed]
- Adhikari NK, Dellinger RP, Lundin S, et al. Inhaled nitric oxide does not reduce mortality in patients with acute respiratory distress syndrome regardless of severity: systematic review and meta-analysis. Crit Care Med 2014;42:404-12. [Crossref] [PubMed]
- Holzgraefe B, Broome M, Kalzen H, et al. Extracorporeal membrane oxygenation for pandemic H1N1 2009 respiratory failure. Minerva Anestesiol 2010;76:1043-51. [PubMed]
- Ventetuolo CE, Muratore CS. Extracorporeal life support in critically ill adults. Am J Respir Crit Care Med 2014;190:497-508. [Crossref] [PubMed]
- Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 2009;374:1351-63. [Crossref] [PubMed]
- Yadav H, Thompson BT, Gajic O. Fifty Years of Research in ARDS. Is Acute Respiratory Distress Syndrome a Preventable Disease? Am J Respir Crit Care Med 2017;195:725-36. [Crossref] [PubMed]
- Kor DJ, Carter RE, Park PK, et al. Effect of Aspirin on Development of ARDS in At-Risk Patients Presenting to the Emergency Department: The LIPS-A Randomized Clinical Trial. JAMA 2016;315:2406-14. [Crossref] [PubMed]
- Terpstra ML, Aman J, van Nieuw Amerongen GP, et al. Plasma biomarkers for acute respiratory distress syndrome: a systematic review and meta-analysis*. Crit Care Med 2014;42:691-700. [Crossref] [PubMed]
Cite this article as: Aronson K, Rajwani K. The acute respiratory distress syndrome: a clinical review. J Emerg Crit Care Med 2017;1:25.


