Catastrophic femoral vein thrombosis in a patient with hypercalcemia due to parathyroid adenoma: a case report
IntroductionOther Section
Hypercalcemia is a common complication in patients with malignant tumor, hyperparathyroidism, end-stage renal disease, and the use of diuretics (1,2). Pathophysiologically, hypercalcemia is a risk factor for thrombosis because ionized calcium is a clotting factor. Calciphylaxis, also known as calcific uremic arteriolopathy (CUA), is a syndrome consists of blood clots, skin necrosis and calcification of blood vessels. CUA is most commonly seen in patients with end-stage renal diseases, and the blood clots are thought to be associated with hypercalcemia. This is a prototype that hypercalcemia can cause blood clot. However, there’s no report on the development of acute femoral vein thrombosis shortly after femoral vein catheterization in a patient with hypercalcemia. Here, we presented a case of severe femoral vein thrombosis, leading to lower limb necrosis and septic shock.
Case presentationOther Section
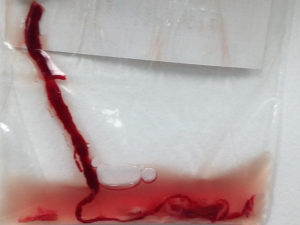
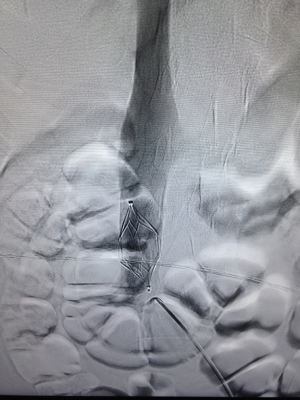
A 40-year old female was presented to our hospital because of intermittent muscular pain, nausea and vomiting for 1 month. On admission, blood chemistry showed hypercalcemia with ionized calcium equal to 6.1 mmol/L. Serum creatinine was 250 mmol/L and the parathyroid hormone was 1,300 pg/mL. Computed tomography (CT) showed inflammatory infiltrates in both lungs and there was a neoplasm measured 2×3 cm in diameter suspected to be associated with parathyroid. Initial treatment included rehydration, pamidronate disodium, synthetic salmon calcitonin and intravenous administration of loop diuretics. The patient was transferred to the intensive care unit (ICU) due to the development of cardiac and renal failures. Meanwhile, serum calcium was not substantially decreased despite intensive treatment. Continuous renal replacement therapy (CRRT) was instituted aiming to reduce serum calcium level. Also, we placed pulse-indicated continuous cardiac output (PiCCO) device to monitor her hemodynamics, and the thermometer was placed in the left femoral artery. Deep vein catheterization was performed in the right leg with under the guidance of color Doppler ultrasound. The process was uneventful. Fifteen hours later, the right leg became swollen and deep vein thrombosis was confirmed by ultrasound. The leg became even more swollen the next day (Figure 1). The temperature of the left leg was low and piebaldness appeared and femoral artery thrombosis was also confirmed. The neoplasm of the parathyroid was removed surgically and a filter was placed in the inferior vena cava to prevent catastrophic pulmonary embolism (Figure 2). At the same time the femoral artery thrombosis was removed after it was confirmed 8 hours (Figure 3). Postoperatively, the pathology showed that that neoplasm was parathyroid adenoma. Intensive anticoagulation was initiated postoperatively to maintain an activated clotting time above 200 seconds. CRRT was resumed immediately after operation. With these treatments, the serum calcium fell to the normal range, urine output increased and cardiac function improved significantly. One week later, CRRT was discontinued and warfarin was started.
Despite these intensive strategies of anticoagulation, the lesion in the lower leg continued to evolve (Figure 4) and eventually, there developed muscular necrosis. Due to the severe necrosis and subsequent infection, the patient developed septic shock. Unfortunately, she died of multiple organ failure on the 18th day after admission.
DiscussionOther Section
Severe hypercalcemia is not rare in hyperparathyroidism, and calciphylaxis is one of the common complications. To the best of our knowledge, there is no report on the development of femoral vein thrombosis in patients with hypercalcemia. Under experienced hand with the use of color Doppler ultrasound, the procedure was uneventful, which excluded vascular injury as the potential cause of thrombosis.
The clinical significance and consequences of hypercalcemia is highlighted by the term hypercalcemic crisis (2). However, this syndrome is rare and is defined as elevated serum ionized calcium levels. The serum ionized calcium levels rarely exceed 3 mmol/L in the literature (1,3,4). Only three cases of hyperthyroidism due to hypercalcemic crisis have been reported (5-7), which have been systematically reviewed by Chen and coworkers (1). In the present case, the patient had a serum ionized calcium level of 6.1 mmol/L, which is very high imposing the patient on the risk of thrombosis. Hypercalcemic crisis may increase the incidence of pancreatitis, mental status changes, fatigue and ectopic glands (8); but it has never been reported to be associated with thrombosis. Manosroi and colleagues reported a case of pulmonary embolism and subclavian vein thrombosis in a patient with parathyroid carcinoma (9). The patient was asymptomatic and the thrombus was thought to be chronic. Furthermore, the extensive formation of thrombus was considered to be associated with hypercoagulability due to paraneoplastic syndrome, which was quite different from that in our case.
As one of the clotting factors, ionized calcium plays an important role in blood coagulation. Our previous study showed that ionized calcium was an independent predictor of filter clotting in patients undergoing CRRT (10), and removing ionized calcium was a way to keep CRRT circuit patent (11). The performance of femoral venous puncture exposes injured endothelium to the blood with high concentrations of ionized calcium. In this situation the release of thrombocinase can be accentuated, predisposing the development of femoral vein thrombosis. To the best of our knowledge, this is the first report showing the development of femoral venous thrombosis in a patient with hypercalcemia. Clinical implications of the case included: (I) if a patient has hypercalcemia, cautions should be practiced in performing femoral vein catheterization. Alternatively, anticoagulation may be considered to prevent femoral venous thrombosis; (II) hypercalcemia maybe a relative contraindication for femoral vein thrombosis, which has never been proposed in the literature.
AcknowledgementsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report.
ReferencesOther Section
- Chen K, Xie Y, Zhao L, et al. Hyperthyroidism-associated hypercalcemic crisis: A case report and review of the literature. Medicine (Baltimore) 2017;96:e6017. [Crossref] [PubMed]
- Ahmad S, Kuraganti G, Steenkamp D. Hypercalcemic crisis: a clinical review. Am J Med 2015;128:239-45. [Crossref] [PubMed]
- Alikhan Z, Singh A. Hyperthyroidism manifested as hypercalcemia. South Med J 1996;89:997-8. [Crossref] [PubMed]
- Iqbal AA, Burgess EH, Gallina DL, et al. Hypercalcemia in hyperthyroidism: patterns of serum calcium, parathyroid hormone, and 1,25-dihydroxyvitamin D3 levels during management of thyrotoxicosis. Endocr Pract 2003;9:517-21. [Crossref] [PubMed]
- Yokomoto M, Minamoto M, Utsunomiya D, et al. Hypercalcemic crisis due to primary hyperparathyroidism occurring concomitantly with Graves’ disease. Intern Med 2015;54:813-8. [Crossref] [PubMed]
- Suzuki H, Kondo K, Saruta T. A case of hypercalcemic crisis with resistant hypertension due to hyperthyroidism. Jpn J Med 1983;22:137-9. [Crossref] [PubMed]
- Endo A, Shigemasa C, Kouchi T, et al. Development of hypercalcemic crisis in a Graves' hyperthyroid patient associated with central diabetes insipidus. Intern Med 1995;34:924-8. [Crossref] [PubMed]
- Cannon J, Lew JI, Solórzano CC. Parathyroidectomy for hypercalcemic crisis: 40 years' experience and long-term outcomes. Surgery 2010;148:807-12; discussion 812-3. [Crossref] [PubMed]
- Manosroi W, Wannasai K, Phimphilai M. Pulmonary Embolism and Subclavian Vein Thrombosis in a Patient with Parathyroid Carcinoma: Case Report and Review of Literature. J Med Assoc Thai 2015;98:925-33. [PubMed]
- Zhang Z, Ni H, Lu B. Variables associated with circuit life span in critically ill patients undergoing continuous renal replacement therapy: a prospective observational study. ASAIO J 2012;58:46-50. [Crossref] [PubMed]
- Zhang Z, Hongying N. Efficacy and safety of regional citrate anticoagulation in critically ill patients undergoing continuous renal replacement therapy. Intensive Care Med 2012;38:20-8. [Crossref] [PubMed]
Cite this article as: Chen L, Zhang Z. Catastrophic femoral vein thrombosis in a patient with hypercalcemia due to parathyroid adenoma: a case report. J Emerg Crit Care Med 2017;1:2.